International Journal of Clinical Medicine
Vol.2 No.5(2011), Article ID:8779,5 pages DOI:10.4236/ijcm.2011.25099
Dilemmas Faced by Nurses Regarding the Physical Restraint of Elderly Patients with Dementia in Japan
![]()
Department of Nursing, Faculty of Nursing and Rehabilitation, Aino University, Osaka, Japan.
Email: tokiwa27@hotmail.com
Received August 8th, 2011; revised September 28th, 2011; accepted October 14th, 2011.
Keywords: Dilemma, Physical Restraint, Elderly Patients, Dementia, Nurse
ABSTRACT
This study aimed to clarify the dilemma of nurses working in general wards who face the ethical dilemma of restraining older people with dementia in Midwestern Japan. The study used the questionnaire method with an independently prepared questionnaire. The questionnaire was designed to ensure privacy and anonymity. The privacy and anonymity of study participants was assured. Of the 340 survey questionnaires distributed, 291 (85.6%) completed surveys were eligible number (12 additional surveys were returned without answers). An explanatory factor analysis revealed four dilemma factors among 15 items investigated (KMO value 0.84). These were: factor 1: “Execution of treatment and security,” α = 0.91; factor 2: “approach in the nursing of older people with dementia,” α = 0.93; factor 3: “A cooperative relationship in nursing of older people with dementia,” α = 0.87; and factor 4: “Priorities in nursing,” α = 0.81. The cumulative contribution ratio was 79.1%. We suggest that the program would enable nurses to cope with these dilemmas.
1. Introduction
In 2000, Japan established long-term care insurance, a system created in response to society’s major concern regarding the aging population and how to care for them. This system was established to assure citizens that they will receive care and be supported by society as a whole. Long-term care insurance is separate from medical care insurance, and was set up as a first step towards revising the structure of social security. In addition, the Ministry of Health, Labour and Welfare passed a bill prohibiting the physical restraint of elderly patients receiving treatment under the long-term care insurance program. As a result, those caring for elderly patients at various institutions became legally prohibited from physically restraining them. Nonetheless, at many general hospitals in Japan, physical restraint is not illegal when treating patients under medical care insurance. In Japan, nursing care continues to include the practice of physical restraint of patients [1], partly due to a lack of effective alternative practices in many general wards where the regulation does not specifically prohibit physical restraint. These practices are likely to continue as cures and effective treatments for dementia are still on the distant horizon. The continued use of restraints has been necessitated by the absence of alternative nursing care techniques to ensure the safety of senile older people with dementia. A patient with dementia hospitalised in a general hospital differs from a senior citizen who enters an institution for medical caretaking. Extra care is necessary for patients with dementia as they may remove intravenous infusion tubes. As a result, nurses in many countries often resort to using physical restraints in order to perform treatment [2].
On the other hand, several trials have demonstrated that physical restraints, rather than protecting the patient, can often cause undue harm [3-6]. Therefore, this phenomenon—whereby restraints are actively used for practical purposes but are not in compliance with current regulations—leaves nurses facing an ethical dilemma [7,8]. Several scholarly articles have addressed the challenges and conflicting feelings faced by nurses in restraining elderly patients with dementia [9]. These issues can cause nurses to question their abilities to deliver high-quality care. The stress, anxiety, and indecision they experience as a result of this ethical dilemma may also contribute to clinical misjudgements. Moreover, the causes of dementia have not yet been clarified, and there is currently no effective treatment or cure available. However, healthcare needs of the elderly with dementia are changing, and are made worse with increasing age. This makes it difficult to care for such patients in hospitals in Japan. At the same time, greater societal awareness of the plight of elderly patients with dementia has placed increased emphasis on delivering high-quality and efficient care to these patients. Nurses, as front-line providers of healthcare, are under enormous pressure to deliver effective and humane service. I already researched ethical dilemma by text date from nurses about ethical dilemma [10]. This study means caught ethical dilemma from elderly people with dementia greater than just elderly patient. Given this background, nurses, particularly those working in general wards, are likely to experience ethical challenges when caring for people with dementia.
2. Objective
The purpose of this study was to clarify the dilemmas experienced by nurses working in general wards who face decisions of physically restraining elderly patients with dementia.
3. Definition of Terms
3.1. Dilemma
Dilemma is a situation in which one must choose between two or more equally unsatisfactory choices. Ham defined ethical dilemma as situations with conflict between two or more ethical principles and each solution may contain unpleasant outcomes for one or more involved parties [11]. We define dilemma in the context of restraining elderly patients as mixed feelings that nurses have when they cannot arrive at a clear answer on a situation and where the basic responsibilities of nursing result in a conflict of whether or not to use restraints on an elderly patient while nursing at a clinical site.
3.2. Elderly People with Dementia
Elderly people who are hospitalized in general wards, more over nurse recognize present in a dementia symptoms state. There is no guarantee that provides confirmation of the diagnosis about dementia from medical doctor.
4. Methods
4.1. Subjects
Participants were 340 nurses at general wards (excluding wards of emergency, psychiatry, pediatrics, obstetrics, outpatient, operating rooms, and intensive care units). Dilemmas were assessed using a questionnaire consisting of 20 items previously developed by the author based on dilemma items (a low score of 1 - 5 points suggest that nurses experienced dilemmas) [8,12]
4.2. Conceptual Framework
The conceptual framework of this study was based upon the MORAL model [13,14] schemata for describing relationships among constructs, concepts, and measurement tools (referents) relevant to a research question. The MORAL model facilitates the understanding of how to cope with ethical dilemmas. M-O-R-A-L involves the following processes: M = Massage the Dilemma, O = Outline Options, R = Review Criteria and Resolve, A = Affirm Position and Act, and L = Look Back.
Massage the dilemma: The first step involves developing a full understanding of the ethical conflict after gathering significant information about the situation. This process includes recognising whose interests are involved, defining the dilemma, and describing conflicting loyalties. Outline options: Nurses who understand the dilemma recognise the conflict involved in the situation. After recognising the conflict, a nurse can then consider how to solve the problem. Review Criteria and Resolve: The third step in the model aims to identify moral criteria and then define a course of action most congruent with those criteria. This step, therefore, is crucial to making a moral judgment that will resolve the dilemma. To complete the R step of the model, examination of moral principles is essential, and it is ideal that a nurse has ample experience in nursing and philosophy. Affirm Position and Act: The first three steps of the Model result in a moral judgment. The A step of the Model moves to acting on one’s knowledge. While developing a moral judgment is the essential preparation for moral action, this alone is insufficient to follow through with the process of the model. A decision-making grid, with actions listed by criteria, may be useful in diagramming this key choice. Look back: In this step, nurses reflect on their perception of the ethical conflict, resourcefulness in generating options, clarification of moral criteria and assessment of options by these criteria. Their solution to the ethical dilemma brings new insights. M clarifies the most recurrent ethical dilemmas in a practice. O includes assessing the nature and adequacy of the alternative strategies. R involves reviewing basic moral principles. Thus, the MORAL model provides an ethical decision-making process enabling nurses to respond to ethical dilemmas in their own practice.
An important aspect of the theoretical framework is the conceptualisation of the term dilemma. The concepttual framework of this study was based upon the MORAL model described by Crisham. We assumed that nurses felt a dilemma when faced with the decision to restrain an elderly patient. Situations in which the nurses would feel a dilemma while physical restraints were being during nursing practice was also assumed. Areas of dilemma were comprised of the following: 1) practice of nursing (No1-4); 2) cooperative relationship in nursing (No1-4); 3) execution of treatment and security (No1-4); 4) individual value system of the nurse (No1-4); and 5) nursing elderly patients with dementia (No1-4). The study was performed using an independently prepared questionnaire addressing the hypothesis. We developed an original 20 item survey based on Crisham [13,14] and Yamamoto [8], and used Kojima et al. as a reference for nursing dilemma items [15]. We assigned each item to the area of best fit. This yielded 20 items, with each of the five areas receiving four items. It was further assumed that dilemmas could be measured using a five-point Likert scale, with a higher score indicating the likelihood that nurses would have mixed feelings. Internal consistency and reliability of the constructed dilemma items were examined using Cronbach’s α coefficient with the criterion set at a coefficient of >0.6. Construction validity was assessed using factor analysis [16]. Internal consistency of the 20 independently prepared items used to measure dilemmas was tested and had a Cronbach’s α coefficient value of 0.87. The correlation coefficient for 15 of the 20 items was lower than 0.5 (0.31 to 0.49), indicating independent responses. Deletion of any single item resulted only in negligible changes in the αcoefficient (Table 1).
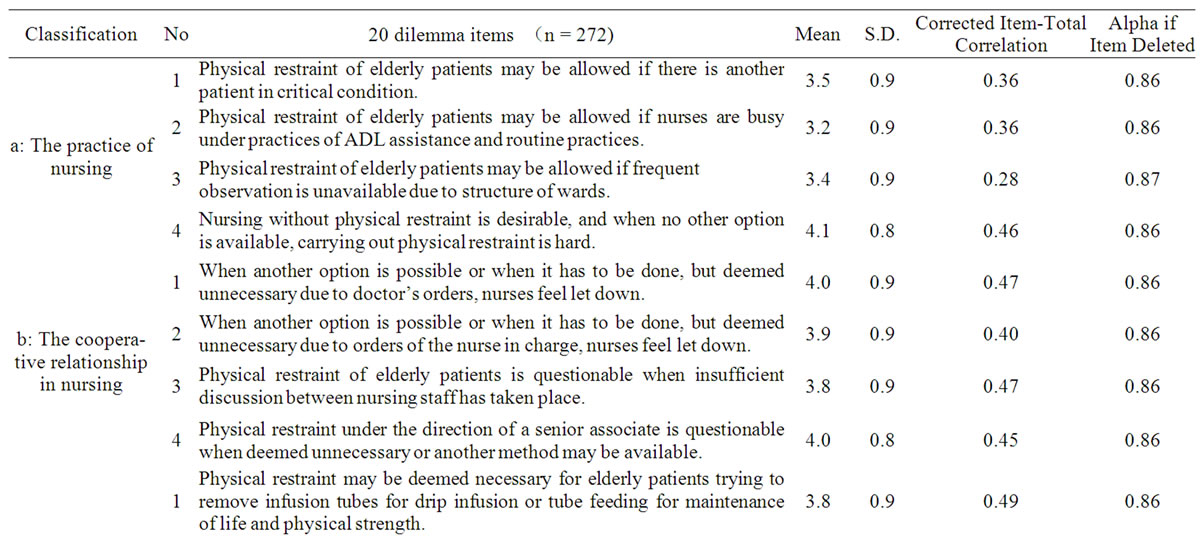
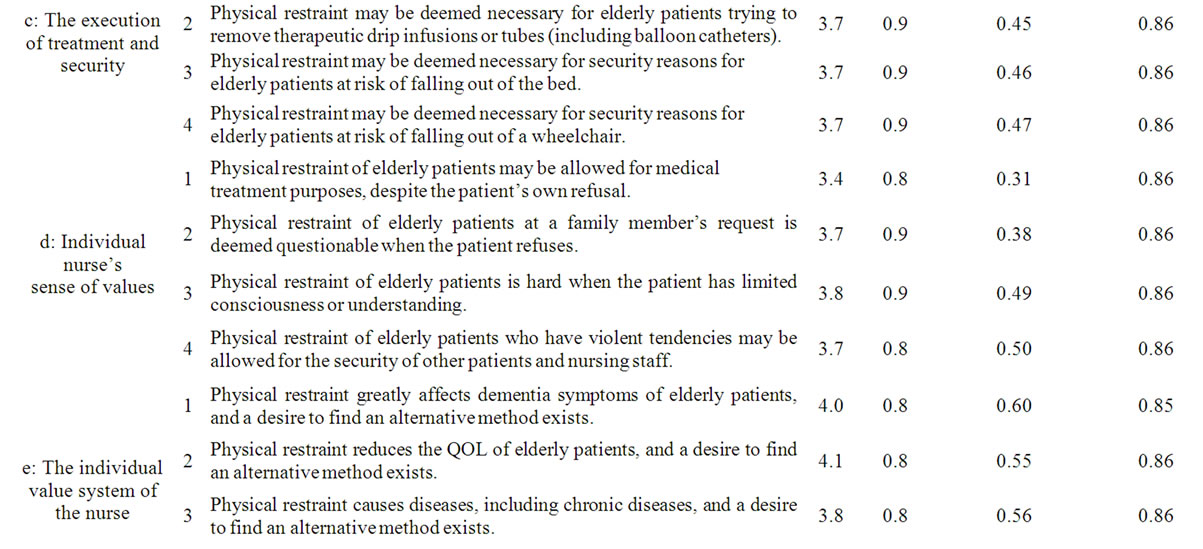
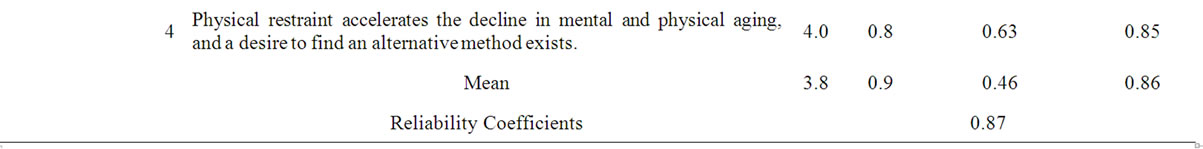
Table 1.Mean and SD of items with dilemma to physical restraints of older people with dementia and reliability coefficients.
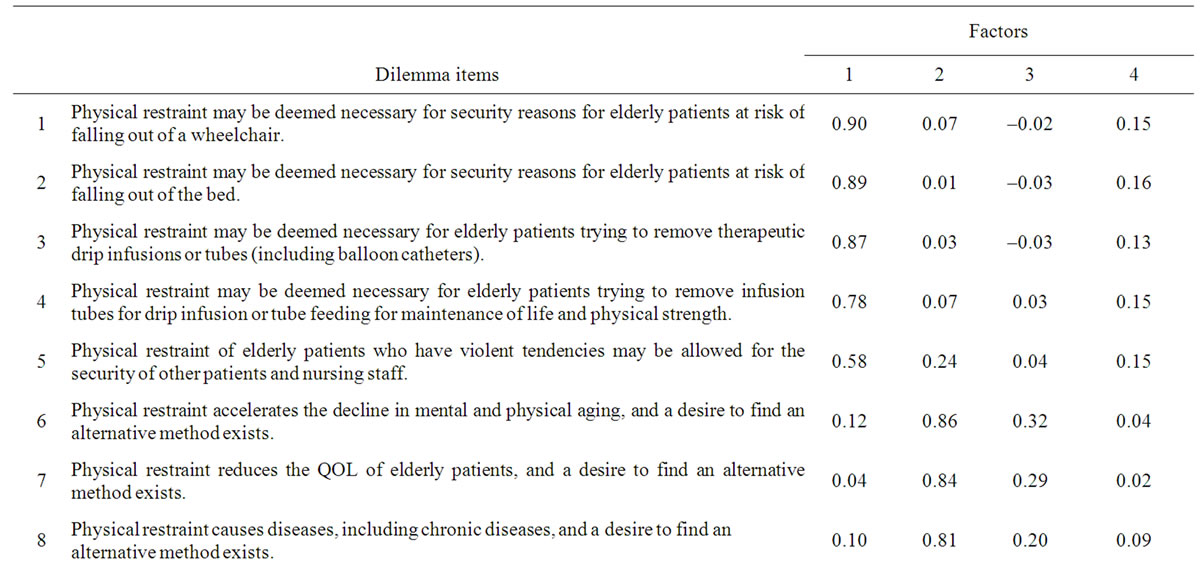
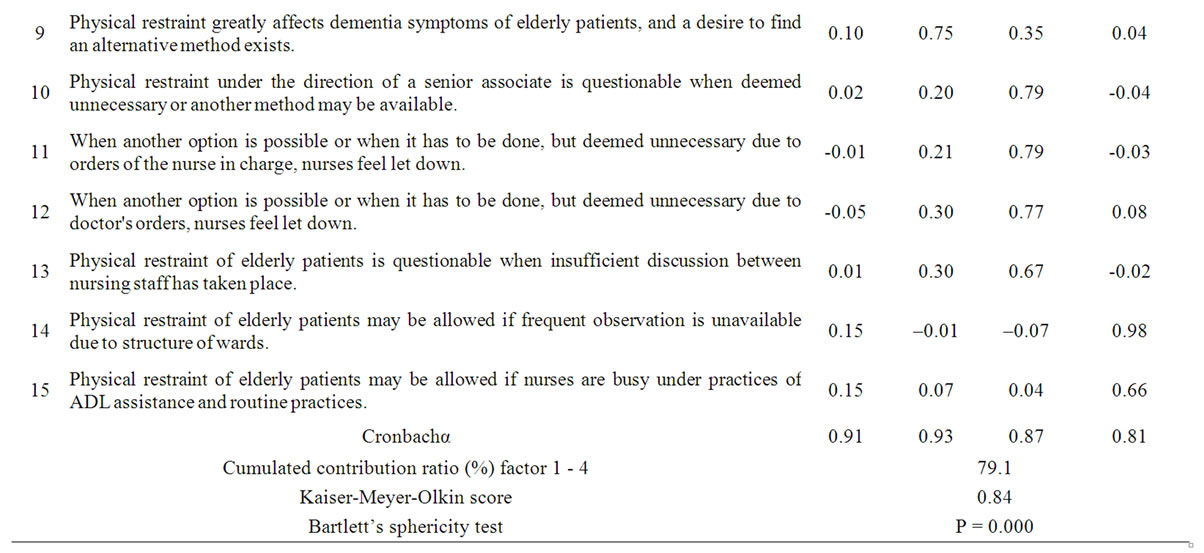
Table 2. Results of factor analysis.
Request sheets disclosing the objective of the study, methods of distribution and retrieval of questionnaires, and addresses of the investigators were distributed.
Alternatively, investigators were interviewed. Details of the study were explained to persons in charge of nursing in the targeted hospitals/wards. A request sheet defining the terms physical restraint and elderly patients, explaining how to fill out the questionnaires, the period of response, and the objective of the present study was were sent to individual nurses. Addresses of the investigators were also enclosed to help facilitate understanding of the study by nurses. A preliminary survey was carried out with 10 nurses working in orthopedic surgery wards in community hospitals (general hospitals with 400 beds) and the obtained results were used to improve the questionnaire. The resulting revised questionnaire was used in this study.
4.3. Ethical Considerations
The questionnaire was designed to ensure privacy and anonymity while allowing participants to complete the form themselves. Participants inserted and sealed the completed questionnaire into an envelope that was provided in advance. The study was conducted with the approval of the ethics committee at Meiji University of Integrative Medicine.
4.4. Statistical Analysis
The factor structure was confirmed after exploratory factor analysis (maximum likelihood method: promax rotation) to assess construct validity. The criteria of sample validity for the factor analysis aimed at a Kiser-Meyer-Olkin measure value of >0.6 and a cumulative contribution ratio of >60.0% [17]. The inclusion of items was applied to a factor loading of >0.4 without any difficulty in interpretation.
5. Results
Subjects’ Characteristics and Validity of Item Selection and Dilemma Factors
To test the validity of item selection and dilemma factorsitems were subjected to factor analysis (maximum likelihood method: promax rotation). Of the 20 items, four had a factor loading of 0.4 or a difficulty in interpretation and were thus excluded; the 15 remaining items were used for analysis. Three items with a characteristic value of 1 were extracted and had a Kaiser-Meyer-Olkin measure value of 0.84 and a cumulative contribution ratio of 79.1% (Table 2). Explanatory factor analysis revealed four dilemma factors among the 15 items: 1) factor 1: execution of treatment and security, α = 0.91; 2) factor 2: approach in nursing elderly patients with dementia, α = 0.93; 3) factor 3: cooperative relationship in nursing elderly patients with dementia, α = 0.87; and 4) factor 4: priorities in nursing, α = 0.81.
6. Discussion
The 20 independently prepared dilemma items produced a high Cronbach’s α coefficient value of 0.84. A low correlation coefficient was found in 15 of the 20 items with independent responses, and only negligible changes were observed regardless of the deletion of any one item. Thus, these items were considered to adequately express the dilemmas. A factor analysis of 15 of the dilemma items extracted four factors as having a characteristic
REFERENCES
- S. Ujiie and Y. Aso, “Physical Restraints,” 6th Edition, Igaku Syoin, Tokyo, 2005.
- J. P. Hamers and A. R. Huizing, “Why Do We Use Physical Restraints in the Elderly?” Zeitschrift Für Gerontologie Udn Geriatrie, Vol. 38, No. 1, 2005, pp. 19-25. doi:10.1007/s00391-005-0286-x
- H. Catchen, “Repeaters: Inpatient Accidents among the Hospitalized Elderly,” The Gerontologist, Vol. 23, No. 3, 1983, pp. 273-276. doi:10.1093/geront/23.3.273
- L. Evans, “Restraint Effectiveness, Occupant Ejection from Cars, and Fatality Reductions,” Accident Analysis & Prevention, Vol. 22, No. 2, 1990, pp. 167-175. doi:10.1016/0001-4575(90)90067-U
- L. C. Burton, et al., “Physical Restraint Use and Cognitive Decline among Nursing Home Residents,” Journal of the American Geriatrics Society, Vol. 40, No. 8, 1992, pp. 811-816.
- K. Parker and S. H. Miles, “Deaths Caused by Bedrails,” Journal of the American Geriatrics Society, Vol. 45, No. 7, 1997, pp. 797-802.
- Y. K. Scherer, et al., “The Nursing Dilemma of Restraints,” Journal of Gerontological Nursing, Vol. 17, No. 2, 1991, pp. 14-17.
- M. Yamamoto, I. Kyoko and K. Usui, “Dilemmas Facing Japanese Nurses Regarding the Physical Restraint of Elderly Patients,” Japan Journal of Nursing Science, Vol. 3, No. 1, 2006, pp. 43-50. doi:10.1111/j.1742-7924.2006.00056.x
- L. K. Evans and V. T. Cotter, “Avoiding Restraints in Patients with Dementia: Understanding, Prevention, and Management Are the Keys,” American Journal of Nursing, Vol. 108, No. 3, 2008, pp. 40-49. doi:10.1097/01.NAJ.0000311827.75816.8b
- M. Yamamoto and Y. Aso, “Placing Physical Restraints on Older People with Dementia,” Nursing Ethics, Vol. 16, No. 2, 2009, pp. 192-202. doi:10.1177/0969733008100079
- K. Ham, “Principled Thinking: A Comparison of Nursing Students and Experienced Nurses,” Journal of Continuing Educction in Nursing, Vol. 35, No. 2, 2004, pp. 66-73.
- International Council of Nursing, “ICN Code for Nursing, Ethical Concepts Applied to Nursing,” Boletin-Colegio de Profesionales de la Enfermería Puerto Rico, Vol. 2, No. 5, 1976, pp. 12-13.
- P. Crisham, “Measuring Moral Judgment in Nursing Dilemmas,” Nursing Research, Vol. 30, No. 2, 1981, pp. 104- 110. doi:10.1097/00006199-198103000-00012
- P. Crisham, “Moral: How Can I Do What’s Right?” Nursing Management, Vol. 16, No. 3, 1985, pp. 42A-42N.
- M. Kojima, “Mapping for Management of Dilemmas of Nurses—Communication with Doctors for Nursing Focused on Patients,” Igaku Syoin, Tokyo, 1997.
- T. Kan, “Analysis of Questionnaire,” Gendai-Sugaku, Kyoto, 1998, in Japanese.
- S. Ishimura and D. Allen, “Dictionary of Statistics,” 8th Edition, Tkyou Tosyo, Tokyo, 2001.
- S. T. Fry, “Nursing Ethics: Current State of the Art,” Journal of Medicine and Philosophy, Vol. 16, No. 3, 1991, pp. 231-234.

