Open Journal of Obstetrics and Gynecology
Vol.04 No.14(2014), Article ID:50670,7 pages
10.4236/ojog.2014.414124
Maternal and Neonatal Outcome for Singleton and Twin Pregnancies in Emergency Cesarean Section vs. Urgent Cesarean Section in a Retrospective Evaluation from 2003-2012
Andrea Mölgg, Stefan Jirecek, Victoria Girtler, Rainer Lehner*
Department of Obstetrics and Gynecology, Medical University of Vienna, Vienna, Austria
Email: *rainer.lehner@meduniwien.ac.at
Academic Editor: Moon Whanim, Inha University School of Medicine, South Korea
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 29 August 2014; revised 23 September 2014; accepted 15 October 2014
ABSTRACT
Objectives: Emergency cesarean is performed, when a situation requires immediate action in order to reduce the risk to mother and/or child, while urgent cesarean is done if a non-life threatening but compromising situation occurs. The aim of the study was to investigate the maternal and fetal outcome for emergency and urgent cesarean. Study Design: A retrospective case-control study was performed; cases underwent emergency cesarean section, while controls underwent urgent cesarean section. We included 303 cases of women and 336 cases of children, and controls were matched. Maternal and fetal outcome parameters for singleton and twin pregnancies were investigated using the Wilcoxon test and the Chi-square-test. Results: Maternal outcome: Higher blood loss (cases: mean 383.12 ± 232.89, range 100 - 2500 vs. controls: 336.06 ± 129.19, range 100 - 1000, p = 0.008), hemorrhage (34 vs. 11, p < 0.001) and puerperal anemia (30 vs. 10, p < 0.001). Neonatal outcome: One, five, and ten minutes Apgar levels and umbilical cord pH values are lower for cases (p < 0.001 and p < 0.001, respectively). Twins had lower five and ten minutes Apgar levels (p = 0.040 and 0.002), but higher umbilical cord pH values than singletons (p < 0.001). The perinatal mortality among singletons was 3.8%, among twins 8.1%. For cases the perinatal mortality among singletons was 5.7% and 17.14% for twins (control group 1.41% and 2.63%, respectively). Conclusion: The maternal and fetal outcome is poorer in emergency cesarean section. Especially the perinatal mortality is high in emergency cesarean section, particular for twins.
Keywords:
Emergency Cesarean Section, Maternal Outcome, Neonatal Outcome, Twins, Urgent Cesarean Section

1. Introduction
Previous published data classified cesarean, which were not performed as an elective cesarean, in an inconsistent way. The cases, classified as emergency cesareans, were very inhomogeneous. Lucas et al. performed a study in the year 2000 which had the aim to set a new classification for emergency cesareans, and they proposed the following:
1) Emergency cesarean: immediate threat of life for woman or fetus;
2) Urgent: maternal or fetal compromise which is not immediately life threatening;
3) Scheduled: needing early delivery but no maternal or fetal compromise;
4) Elective: at a time to suit the woman and the maternity team [1] .
Emergency cesarean section (ECS) is conducted, when a situation requires immediate action for decreasing the risk to mother and/or child, e.g. placental abruption, bleeding caused by placenta previa or imminent intrauterine asphyxia [2] [3] . An urgent cesarean section (UCS) was conducted during birth process, though a vaginal birth was planned, e.g. a protracted birth [3] . The performance and specifically the time management of emergency cesarean section were discussed in many studies, especially regarding the decision-to-delivery interval (DDI).
The DDI is the time interval between the decision to perform a cesarean and the delivery of the child [4] [5] . The German society for gynecology and obstetrics allows a DDI of 20 minutes, while the American College of Obstetricians and Gynecologists and the Royal College of Obstetricians and Gynecologists recommend a DDI of 30 minutes [6] [7] .
To obey the recommendation of 20 minutes in our institution, a tertiary care hospital with 3500 births per year, the management of emergency cesareans was adapted to the following:
1) On admission the patients are screened for risk factors which could predict complications, e.g. twin pregnancies, former cesareans, especially former emergency of urgent cesarean sections or intrauterine fetal retardation. If risk factors are found, the patients are admitted in a special equipped delivery room (with equipment as lamps or anesthesia machine for an emergency cesarean).
2) If these patients would need an emergency cesarean, it is directly performed in the delivery room.
3) After consultation with the anesthesiologist women without former epidural anesthesia received general anesthesia.
4) The obstetric staff is equipped with an ECS beeper. When ECS alarm is given, the staff has to call back immediately. In the ECS protocol the time of the alarm, the call back time, the indication for the ECS, the gestational age, the birth weight, the pH and the Apgar score are registered.
Due to consequent implementation of these steps and good interdisciplinary communication, the DDI decreased from average 15.39 to 9.43 minutes.
Although the recommended 20 minutes are an accurate goal in most patients, the situation itself has high stress potential for women and child, and the life threatening situation leading to the decision to undertake an ECS could also affect the outcome. Recommendations for time management for UCS do not exist.
The aim of the study was to investigate the maternal and neonatal outcomes for ECS and UCS, in respect.
2. Methods
The study was conducted as a case-control study. In the study period from 2003 to 2012 all women undergoing a cesarean section in our institution were recorded in an in-house database. All women undergoing an ECS in the study period (singleton and twin pregnancies) were included in the case group. Controls were matched by age.
All children (singleton and twins) born by ECS during the study period were included in the case group, controls were matched by sex and gestational age.
In the case group 303 women and 336 children were included and 303 women and 336 children were matched as controls.
The maternal outcome was defined by blood loss, hemorrhage, integrity of the placenta, anomaly of placental separation, eclampsia, hysterectomy, puerperal fever, sepsis, anemia and death. The new-born outcome was defined by stillbirth, Apgar score, umbilical cord pH, admission to NICU and death within seven days.
The study was approved by the local ethic committee (#1282/2013, 17.04.2013).
Statistics
First descriptive analyses were performed to describe both groups. Epidemiologic and anamnestic parameters were compared, e.g. age, obstetric parameters, gestational age, weight of the new-born, sex or malformations. The frequency of maternal and neonatal morbidities were investigated and compared between cases and controls, also regarding singleton and twin pregnancies. The Wilcoxon test and the Chi-square-test were conducted. p < 0.05 was considered statistically significant. All statistical analyses were performed with IBM SPSS Statistics 19 for windows.
3. Results
3.1. Maternal Outcome
The women age ranged from 15 to 51 (median 31, mean 30.73 ± 6.63). The obstetric parameters are listed in Table 1. No differences were was found between the two groups.
Table 1. Descriptive parameters cases vs. controls.
ECS: emergency cesarean section, UCS: urgent cesarean section.
The women had the same median BMI and weight, no differences were found regarding infections status as HIV, hepatitis, toxoplasmosis or lues.
Premature rupture of membranes was found in 80 cases and 100 controls, the difference was significant (p = 0.004). 29 cases and 51 controls had induction of labor (p = 0.011). Women undergoing ECS had general anesthesia more often than women undergoing UCS (175 cases vs. 8 controls), while controls were more likely to have a spinal anesthesia (61 cases vs. 212 controls; p < 0.001). Use of oxitocin for bradytocia was found in 28 cases and 53 controls (p = 0.011). The most common fetal presentation was vertex presentation (n = 405, 66.83%), followed by breech presentation (n = 56, 9.24%). The most common indications for ECS were imminent intrauterine asphyxia and unspecified threat of life of the fetus, for UCS the most common indication was protracted birth. The median week of gestation in the case group was 36th (mean 34.56 ± 6.02), in the control group 38th (mean 36.65 ± 4.47; p < 0.001).
The blood loss in the case group was higher than in the control group (cases: mean 383.12 ± 232.89, range 100 - 2500 vs. controls: 336.06 ± 129.19, range 100 - 1000, p = 0.008). Hemorrhage was found in 34 cases and 11 controls (p < 0.001). 30 cases and 10 controls had anemia (p < 0.001), the median hemoglobin level of patients with anemia was 8.9 for cases and 9.40 for controls (cases: mean 8.59 ± 1.11, range 6.6 - 9.9 g/dl vs. controls: mean 9.01 ± 0.90, range 7.7 - 9.9 g/dl).
Regarding integrity of the placenta, anomaly of placental separation, eclampsia, hysterectomy, puerperal fever and sepsis no differences were found between the two groups. No maternal death was recorded.
We investigated, if there is a difference between singleton and twin pregnancies. 521 singleton and 85 twin pregnancies were found. No differences were found regarding blood loss, hemorrhage, integrity of the placenta, anomaly of placental separation, eclampsia, hysterectomy, puerperal fever, sepsis and anemia.
No differences were found between singleton and twin pregnancies in the case and control group.
3.2. Neonatal Outcome
The children were in the 35th week of gestation (mean 24.17 ± 5.72). 398 were male, 274 female. No significant differences were found regarding head circumference, weight, height and frequency of malformations (see Table 1).
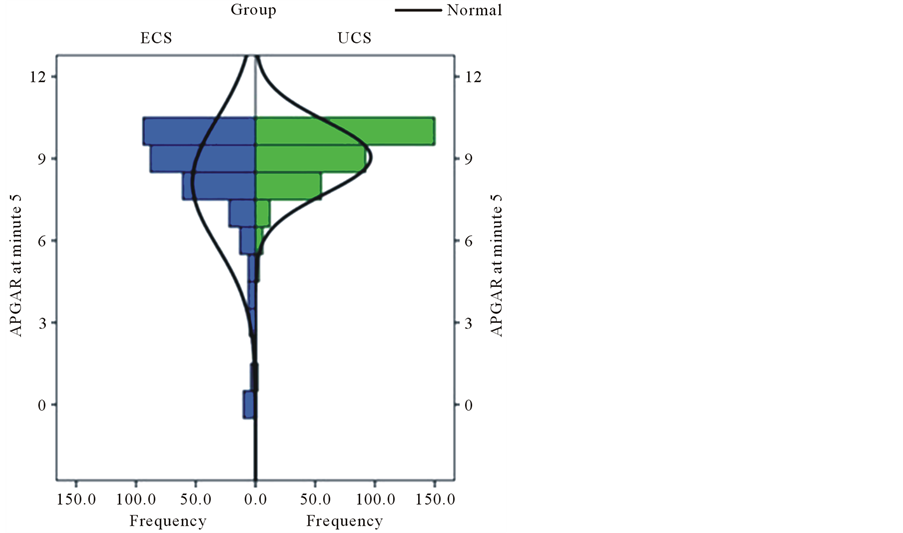
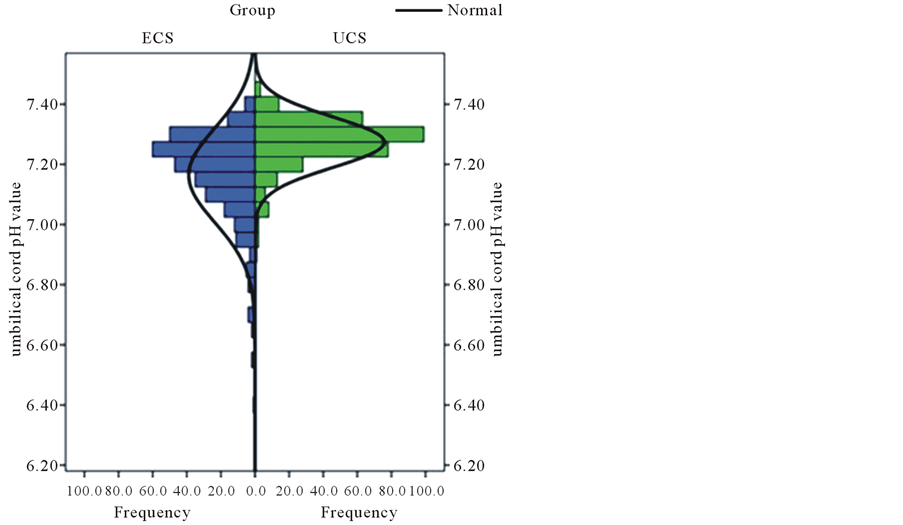
The Apgar levels at one, five and ten minutes were lower in the case group than in the control group (p < 0.001). The umbilical cord pH level was also lower in the case group (p < 0.001). The data is shown in Table 2 and graphs 1 and 2. Children born by ECS were more likely to be transferred to the NICU than children born by UCS (169 vs. 135, p = 0.002). 7 stillbirths were found in the case group vs. 1 stillbirth in the control group. Of
Table 2. Apgar scores and umbilical cord pH values cases vs. controls with comparison of singletons and twins.
Differences between cases and controls for APGAR 1, APGAR 5, APGAR 10, and umbilical cord pH were significant with p < 0.001. The data was evaluated with the Wilcoxon test.
336 children in the case group 21 died within the first week, in the control group 5 children died within the first week (p < 0.001). The most common reasons were respiratory problems and immaturity due to preterm delivery. The perinatal mortality was 8.3% for cases and 1.7% for controls.
471 children were singletons and 184 were twins. The Apgar levels after five and ten minutes and the umbilical cord pH were not the same among singletons and twins. The Apgar level after five minutes were higher for singletons than for twins (median 9, mean 8.65 ± 1.97 vs. median 9, mean 8.53 ± 1.88, p = 0.040). The Apgar level after 10 minutes were higher for singletons than for twins (median 10, mean 9.06 ± 1.91 vs. median 9, mean 8.90 ± 1.95, p = 0.002). Twins had higher umbilical cord pH levels than singletons (median 7.28, mean 7.26 ± 0.09 vs. median 7.24, mean 7.20 ± 1.91, p < 0.001) (Figure 1, Figure 2).
The data for cases and controls are shown in Table 2.
183 (of 399, 45.86%) of singletons were transferred to NICU, 107 (of 156, 68.58%) of twins were transferred to NICU (p < 0.001).
The perinatal mortality among singletons was 3.8%, among twins 8.1%. In the case group (ECS—259 singletons and 70 twins) the perinatal mortality among singletons was 5.7% (2 stillbirths and 13 deaths within the first week) and 17.14% for twins (5 stillbirths and 7 deaths within the first week). In the control group (UCS—212 singletons and 114 twins) the perinatal mortality among singletons was 1.41% (0 stillbirths and 3 deaths within the first week) and 2.63% for twins (1 stillbirth and 2 deaths within the first week).
54.26% of Singletons born by ECS were transferred to NICU, twins 77.7%. For UCS it was 35.22% and 63.72%, respectively.
The outcome was investigated regarding the sequence at the birth. No differences were found for the Apgar levels, the umbilical cord pH, transfer to NICU or perinatal mortality between the first or the second born twin.
4. Discussion
An unpredictable event, which leads to the conduction of an ECS, is a strong stressor for the mother and her child. The additional stress may influence the maternal and neonatal outcome. Differences in the maternal and
Figure 1. Distribution of APGAR value after 5 minutes for cases and controls. The figure shows the five minute APGAR levels of neonates which underwent emergency cesarean section and urgent cesarean section. The difference between the two groups was significant in the Wilcoxon test with p < 0.001.
Figure 2. Distribution of umbilical cord pH value for cases and controls. The figure shows the umbilical cord pH values of neonates born by emergency cesarean section compared with neonates which underwent urgent cesarean section. The difference between the two groups was significant in the Wilcoxon test with p < 0.001.
neonatal outcome are partially explainable regarding the underlying pathologies. Indications for ECS are acute life threatening events, whereas UCS are conducted for maternal or fetal compromise which is not immediately life threatening.
Studies have shown that a shorter DDI is associated with poorer fetal outcomes [8] -[10] , tough the hypoxic event is finished earlier. Theories to explain this phenomenon include, that the anxiety for the woman generated by the decision for ECS may provoke increased maternal catecholamine release that initially causes reduced perfusion of the placental bed and gas exchange, causing temporal fetal acidosis [8] . Even though the uterine vessels should be constricted due to catecholamine release, the blood loss of women undergoing ECS was higher than in women undergoing UCS. The vasoconstriction of blood vessels in the uterus is induced by norepinephrine, whereas epinephrine causes vasodilatation. Segal et al. showed that the beginning of efficient analgesia reduces the level of epinephrine [11] . The analgesia at ECS is probably not as efficient as at UCS because of the fast induction of anesthesia. However not every circumstance having influence to the blood loss is known.
Women undergoing ECS were in the 36th week of gestation, whereas women with UCS were in the 38th week. This fact surely affects the outcome, especially the neonatal outcome. The mortality of “late preterm” is higher compared with mature new-born [12] . Even though in this study the neonates were matched by gestational week to diminish this influence of gestational age at the mortality, the perinatal mortality was higher for ECS than UCS (8.3% vs. 1.7%). The perinatal mortality was also influenced by the fact, if the pregnancy was singleton or multiple. Singletons had a perinatal mortality of 3.8%, twins of 8.1%. Singletons born with ECS had a higher mortality than singletons born with UCS (5.7% vs. 1.4%). Twins born with ECS had a higher mortality than twins born with UCS (17.41% vs. 2.63%). Admission to NICU was more frequent for twins; in the case group the probability was higher than in the control group. (ECS vs. UCS singletons 54.26% vs. 35.22%, twins 77.7% vs. 63.72%). Other studies showed that the perinatal mortality is higher for twins than for singletons and that twins were more often transferred to NICU [13] [14] . The Apgar score after one, five and ten minutes was different in the case and the control groups. The Apgar score was initially conceived as predictor for survival and to evaluate resuscitation, but not to predict the long term outcome. The score is not only influenced by gestational age, maternal medication and resuscitation but also by neurological and respiratory complications. The five-minute Apgar score is not a good marker for an acute hypoxic event during birth [15] [16] . In addition the condition leading to the conduction of an ECS may have influence on the Apgar levels. In our study singletons had a higher five and ten minute Apgar score than twins. Although the Apgar levels were significantly lower in the case group, the validity is questionable because most of the children in the case and the control groups achieved high levels from 7 - 10, which are classified as normal [15] .
The pH values were lower in the case group (median 7.20) than in the control group (median 7.29). Eskes et al. had shown that at fetal bradycardia, which is often associated with hypoxia, the pH value declines every minute about 0.006 units [17] . This may also have influence on the lower pH in the case group. Interestingly the umbilical cord pH value was lower for singletons than for twins, especially in the case group. Georgieva et al. had shown that the umbilical cord pH is a good predictor for low Apgar score, need for resuscitation, ventilation with mask, seizures and other cerebral problems including death [18] .
Various studies had shown that the second born twin has a poorer outcome than the first born [19] [20] . This could not be repeated in this study.
5. Conclusions
In summary, the maternal and fetal outcome is poorer in ECS than UCS. The maternal blood loss is higher, hemorrhage is more frequent, just as puerperal anemia. Apgar levels and umbilical cord pH values are lower at neonates born by ECS. Twins had lower Apgar levels, but higher umbilical cord pH values. The perinatal mortality is higher for singletons than for twins.
The study has some limitations, in parts caused by the retrospective design with possible errors in data selection. The number of investigated patients was low, especially for twin pregnancies, which could also reduce the validity of the study.
Condensation
Comparison of the maternal and neonatal outcome for singletons and twins between emergency and urgent cesarean sections.
Conflict of Interest
The authors report no conflict of interest.
References
- Lucas, D.N., Yentis, S.M., Kinsella, S.M., Holdcroft, A., May, A.E., Wee, M., et al. (2000) Urgency of Caesarean Section: A New Classification. Journal of the Royal Society of Medicine, 93, 346-350.
- Lurie, S., Sulema, V. and Kohen-Sacher, B. (2004) The Decision to Delivery Interval in Emergency and Non-Urgent Cesarean Sections. European Journal of Obstetrics & Gynecology and Reproductive Biology, 113, 182-185. http://dx.doi.org/10.1016/j.ejogrb.2003.09.022
- Helmy, W.H., Jolaoso, A.S., Ifaturoti, O.O., Afify, S.A. and Jones, M.H. (2002) The Decision-to-Delivery Interval for Emergency Caesarean Section: Is 30 Minutes a Realistic Target? BJOG: An International Journal of Obstetrics & Gynaecology, 109, 505-508. http://dx.doi.org/10.1111/j.1471-0528.2002.00491.x
- Hillemanns, P.H.H., Rebhan, H. and Knitza, R. (1996) Notsectio-Organisation und E-E-Zeit. Geburtshilfe und Frauen- heilkunde, 56, 423-430. http://dx.doi.org/10.1055/s-2007-1023258
- DGGG (2010) Stellungnahme zur Frage der erlaubten Zeit zwischen Indikationsstellung und Sectio (E-E-Zeit) bei einer Notlage. Leitlinien, Empfehlungen, Stellungnahmen.
- ACOG (2009) ACOG Committee Opinion No. 433: Optimal Goals for Anesthesia Care in Obstetrics. Obstetrics & Gynecology, 113, 1197-1199. http://dx.doi.org/10.1097/AOG.0b013e3181a6d04f
- Royal College of Obstetricians and Gynaecologists, Royal College of Anaesthetists, Royal College of Midwives, Royal College of Paediatrics and Child Health (2008) Standards for Maternity Care: Report of a Working Party. RCOG Press, London. https://www.rcm.org.uk/sites/default/files/WPRMaternityStandards2008.pdf
- MacKenzie, I.Z. and Cooke, I. (2001) Prospective 12 Month Study of 30 Minute Decision to Delivery Intervals for “Emergency” Caesarean Section. British Medical Journal, 322, 1334-1335. http://dx.doi.org/10.1136/bmj.322.7298.1334
- MacKenzie, I.Z. and Cooke, I. (2002) What Is a Reasonable Time from Decision-to-Delivery by Caesarean Section? Evidence from 415 Deliveries. BJOG: An International Journal of Obstetrics & Gynaecology, 109, 498-504. http://dx.doi.org/10.1111/j.1471-0528.2002.01323.x
- Thomas, J., Paranjothy, S. and James, D. (2004) National cross Sectional Survey to Determine whether the Decision to Delivery Interval Is Critical in Emergency Caesarean Section. British Medical Journal, 328, 665. http://dx.doi.org/10.1136/bmj.38031.775845.7C
- Segal, S. and Wang, S.Y. (2008) The Effect of Maternal Catecholamines on the Caliber of Gravid Uterine Microvessels. Anesthesia & Analgesia, 106, 888-892. http://dx.doi.org/10.1213/ane.0b013e3181617451
- Tomashek, K.M., Shapiro-Mendoza, C.K., Davidoff, M.J. and Petrini, J.R. (2007) Differences in Mortality between Late-Preterm and Term Singleton Infants in the United States, 1995-2002. The Journal of Pediatrics, 151, 450-456.
- Mazhar, S.B., Peerzada, A. and Mahmud, G. (2002) Maternal and Perinatal Complications in Multiple versus Singleton Pregnancies: A Prospective Two Years Study. Journal of Pakistan Medical Association, 52, 143-147.
- Pinborg, A., Loft, A. and Andersen, A.N. (2004) Neonatal Outcome in a Danish National Cohort of 8602 Children Born after in Vitro Fertilization or Intracytoplasmic Sperm Injection: The Role of Twin Pregnancy. Acta Obstetricia et Gynecologica Scandinavica, 83, 1071-1078. http://dx.doi.org/10.1111/j.0001-6349.2004.00476.x
- ACOG (2006) ACOG Committee Opinion, No. 333: The Apgar Score. Obstetrics & Gynecology, 107, 1209-1212.
- Ehrenstein, V. (2009) Association of Apgar Scores with Death and Neurologic Disability. Journal of Clinical Epidemiology, 1, 45-53. http://dx.doi.org/10.2147/CLEP.S4782
- Eskes, T.K. (1993) Uterine Contractions and Their Possible Influence on Fetal Oxygenation. Gynakologe, 26, 39-45.
- Georgieva, A., Moulden, M. and Redman, C.W. (2013) Umbilical Cord Gases in Relation to the Neonatal Condition: The EveREst Plot. European Journal of Obstetrics & Gynecology and Reproductive Biology, 168, 155-160.
- Prins, R.P. (1994) The Second-Born Twin: Can We Improve Outcomes? American Journal of Obstetrics and Gynecology, 170, 1649-1657. http://dx.doi.org/10.1016/S0002-9378(94)70336-1
- Stein, W., Misselwitz, B. and Schmidt, S. (2008) Twin-to-Twin Delivery Time Interval: Influencing Factors and Effect on Short-Term Outcome of the Second Twin. Acta Obstetricia et Gynecologica Scandinavica, 87, 346-353. http://dx.doi.org/10.1080/00016340801934276
NOTES

*Corresponding author.