Open Journal of Pediatrics
Vol. 2 No. 2 (2012) , Article ID: 19876 , 5 pages DOI:10.4236/ojped.2012.22028
Paediatric amitriptyline overdose
![]()
1Tamworth Rural Referral Hospital, Tamworth, Australia
2Waikato Hospital, Hamilton, New Zealand
Email: *Steven.Doherty@hnehealth.nsw.gov.au, grantcave@gmail.com, harveym@waikatodhb.govt.nz
Received 20 March 2012; revised 8 May 2012; accepted 19 May 2012
Keywords: Tricyclic Anti-Depressants; Toxicity; Overdose
ABSTRACT
We report a near fatal case of paediatric amitriptyline overdose including a series of ECGs demonstrating the effects of sodium bicarbonate therapy on cardio-toxicity. We briefly discuss the role of sodium to counteract the sodium channel blockade of tricyclic antidepressants and discuss the possible utility of lipid emulsion therapy in such cases.
1. INTRODUCTION
We describe a case of near fatal amitriptyline overdose in a 9 year old boy. Tricyclic antidepressants (TCAs) cause anticholinergic effects, alpha adrenergic blockade and have fast sodium-channel blocking effects. The case highlights the serious neurological and cardiotoxic effects of TCA overdose and contains a series of instructive ECGs that demonstrate the benefits of bicarbonate therapy. Although not used in this case, the possible efficacy of lipid emulsion therapy for this overdose is discussed.
2. CASE REPORT
A 9 year old male with a history of behaviour disorder was brought in by ambulance following an intentional overdose of 500 mg Amitriptyline. He had witnessed convulsive movements in the ambulance. During transport he had a BP of 95/50, was afebrile, a pulse of 150 and a BSL of 6.5 mmol/L. He was known to weigh 35 kg.
On arrival he was unconscious with a GCS of 7 (E1V2M4), had mid-range pupils, was tolerating an oropharyngeal airway and had small amounts of vomitus in his mouth. Soon after arrival in the ED he had a generalised tonic-clonic seizure that was brief and self terminating. Cardiac monitoring demonstrated a rate of 160 with wide and bizarre ECG complexes. On the basis of his initial monitoring he was given 35 mmol (1 mmol/kg) of sodium bicarbonate and also received 2 mg diazepam intravenoulsy. He underwent rapid sequence induction with thiopentone and suxamethonium and was intubated and ventilated.
There were no other significant health issues. His usual Amitryiptyline dose was 10 mg twice daily. He was on no other medications.
An ECG (ECG 1), after 35 mls of 8.4% sodium bicarbonate, revealed a tachycardia of 157, prolonged QRS and prolonged QT intervals. Further doses of sodium bicarbonate were administered in response to serial ECGs and these subsequent doses reduced the tachycardia to 132/min and QRS duration 132 ms (ECG 2) and then to 100/min and 126 ms (ECG 3) and resulted in a more normal appearance to the ECG complexes.
A midazolam infusion was commenced for the dual purpose of sedation and to prevent further seizure activity. He was transferred to Intensive Care where a magnesium infusion was commenced due to concerns about the QT interval. He was hyperventilated to keep his ETCO2 between 30 - 35.
Blood tests including a full blood count, urea, electrolytes, creatinine, calcium and magnesium were all within normal limits.
He remained intubated and ventilated for over 24 hours before being extubated uneventfully. His ECG returned to normal (ECG 4) and there was no further seizure activity. Whilst still in hospital he had further psychiatric review.
3. DISCUSSION
This case highlights the lethality of tricyclic antidepressants (TCAs) in overdose with unconsciousness, seizures and QRS prolongation and the series of ECGs highlights the benefits of sodium bicarbonate as a treatment.
Tricyclic anti-depressants have been in use for over 50 years and their toxicity partly relates to their narrow therapeutic index. Their use as antidepressants has reduced with the emergence of newer agents, but they are still used for other indications and in the paediatric population this can include for conditions such as obsessive-compulsive disorder and attention deficit hyperactivity disorder [1].
In 2004 nearly 3000 children were poisoned with tricyclics in the US and half of these were in children aged 6 - 19 years. Adolescents tended to present with intentional overdose. [1] In children doses of 5 mg/kg are potentially toxic and severe toxicity is likely at doses of 20 mg/kg [1,2].
TCAs block sodium channels and this partly explains the central nervous system and pro-arrhythmic effects in overdose. Sodium bicarbonate is the mainstay of therapy in TCA overdose [1,2]. Alkalinisation increases the protein binding of the drug and also presents a sodium load which may partly overcome sodium channel blockade [2]. There is animal evidence [3] that sodium loading is more effective than alkalinisation, with hypertonic saline having a greater effect on reducing QRS duration than sodium bicarbonate therapy. There is also case-report evidence that hypertonic saline can further reduce QRS duration when standard therapy with sodium bicarbonate has been ineffective [4]. The value of hyperventilation alone is not established [3].
Whilst not used in this case, intravenous lipid emulsion (ILE) is a recommended treatment for the sodium channel toxidrome in local anaesthetic toxicity [5] and has been advocated in the treatment of intractable tricyclic antidepressant toxicity [6]. Evidence from animal studies show haemodynamic, and survival benefits from the use of lipid emulsion in tricyclic toxicity [7-9]. There is evidence for a plausible mechanism, sequestration of toxin in a newly created intravascular lipid phase, with increased blood carriage of toxin seen in lipid treated animals [9]. The safety of Intralipid use in children has been established with regards to total parenteral nutrition but there is little experience of its use as a rescue therapy in overdose in the paediatric population.
There is a small amount of human evidence in this area. Two cases have been reported as conference abstracts. One case involved a 52 year old female who continued to be unstable on maximal therapy after an overdose of 6 grams of imipramine. Haemodynamic stability was achieved 30 minutes after bolus ILE followed by infusion [10]. In the second case an 80 year old male intoxicated with 1.5 grams of doxepin remained unstable post sodium bicarbonate and vasopressor infusions. ILE was used, with haemodynamic stability and weaning of bicarbonate and vasopressors in 150 minutes [11]. Three additional cases involving amitriptyline toxicity were reported briefly as part of a case series with two of the patients surviving [12]. While attributing improvement to ILE is not possible, these cases support the view that use of ILE in the setting of the critically ill patient refractory to standard therapy is justified.
There is a single human study in which subjects were given pharmacologic dose amitriptyline to steady state followed by lipid infusion. A nonsignificant rise in amitriptyline concentration was seen [13], supporting the concept of sequestration of the drug in the intravascular lipid phase.
4. SUMMARY
This case highlights some of the classic features of TCA toxicity and the ECGs provide an illustrative example of the effects of sodium bicarbonate on cardiac toxicity.
The concept of binding toxicological drugs is the basis of the emerging interest in therapies such as ILE. The ability of ILE to bind TCAs and maintain them in the circulation, thus preventing uptake into cells, may reduce toxicity. Whilst it is not a standard therapy for TCA overdose at this point ILE should be considered in severe toxicity.
REFERENCES
- Soghoian, S., Doty, C.I., Maffei, F.A. and Connolly, H. Toxicity, tricyclic antidepressant. eMedicine Paediatrics. www.emedicine.medscape.com/article/1010089
- Emergency Medicine Expert Group (2008) Therapeutic guidelines: Toxicology and wilderness. Version 1. Therapeutic Guidelines Limited, Melbourne.
- McCabe, J.L., Cobaugh, D.J., Menegazzi, J.J. and Fata, J. (1998) Experimental tricyclic antidepressant toxicity: A randomized, controlled comparison of hypertonic saline solution, sodium bicarbonate, and hyperventilation. Annals of Emergency Medicine, 32, 329-333. doi:10.1016/S0196-0644(98)70009-5
- McKinney, P.E. and Rasmussen, R. (2003) Reversal of severe tricyclic antidepressant-induced cardiotxicity with intravenous hypertonic saline. Annals of Emergency Medicine, 42, 20-24. doi:10.1067/mem.2003.233
- Harrop, G.W., Picard, J., Meek, T., et al. (2010) AAGBI safety guideline, management of severe local anaesthetic toxicity. http://www.aagbi.org/publications/guidelines/docs/la_toxicity_2010.pdf
- Toxbase Database Information (2010) Amitryptiline. UK National Poisons Information Centre.
- Harvey, M. and Cave, G. (2007) Intralipid outperforms sodium bicarbonate in a rabbit model of clomipramine toxicity. Annals of Emergency Medicine, 49, 173-185. doi:10.1016/j.annemergmed.2006.07.016
- Bania, T.C. and Chu, K. (2006) Hemodynamic effect of intralipid on amitryptilline toxicity. Annals of Emergency Medicine, 13, S177. doi:10.1197/j.aem.2006.03.448
- Harvey, M., Cave, G. and Hoggett, K. (2009) Correlation of plasma and peritoneal diasylate clomipramine concentration with hemodynamic recovery after intralipid infusion in rabbits. Academic Emergency Medicine, 16, 151-156. doi:10.1111/j.1553-2712.2008.00313.x
- Carr, D., Boone, A., Hoffman, R.S., Martin, K. and Ahluwalia, N. (2009) Successful resuscitation of a doxepin overdose using intravenous fat emulsion (IFE). Clinical Toxicology, 47, 710.
- Al-Duaij, N., George, M., O’Donnell, K., et al. (2009) Lipid emulsion therapy in massive imipramine overdose. Clinical Toxicology, 47, 460.
- Geib, A.J., Manini, A. and Liebelt, E. (2009) Case series of intravenous lipid emulsion rescue for drug cardiotoxicity. Clinical Toxicology, 47, 704.
- Minton, N., Goode, A. and Henry, J. (1987) The effect of a lipid suspension on amitryptiline disposition. Archives of Toxicology, 60, 467-469. doi:10.1007/BF00302392
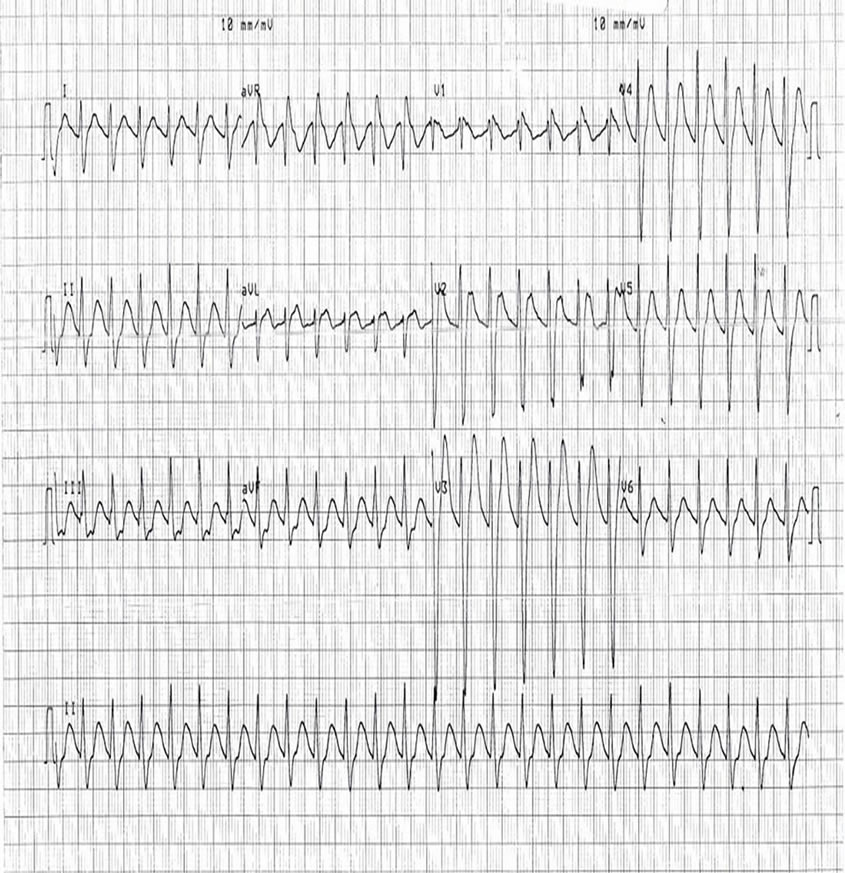 ECG 1
ECG 1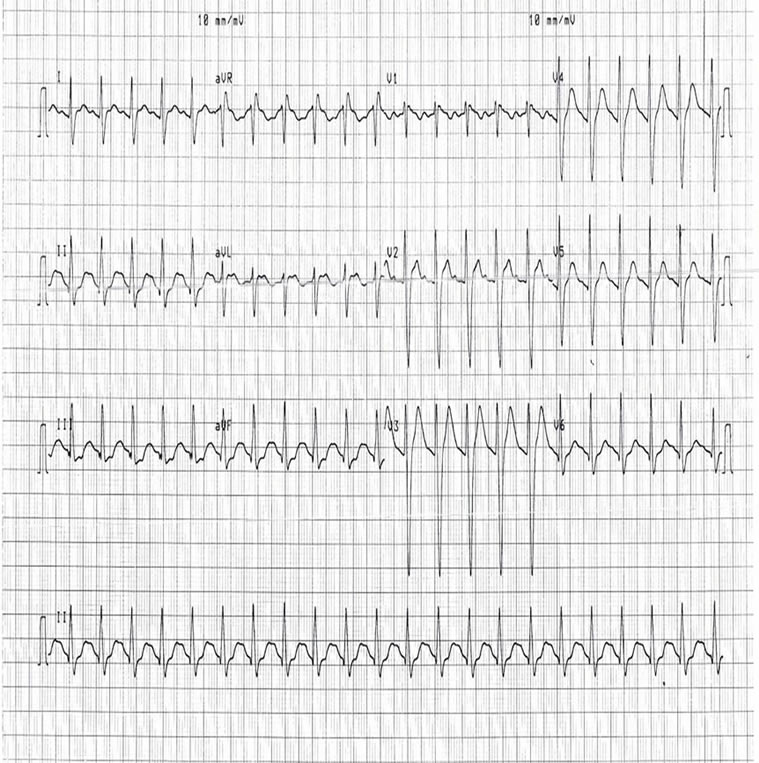 ECG 2
ECG 2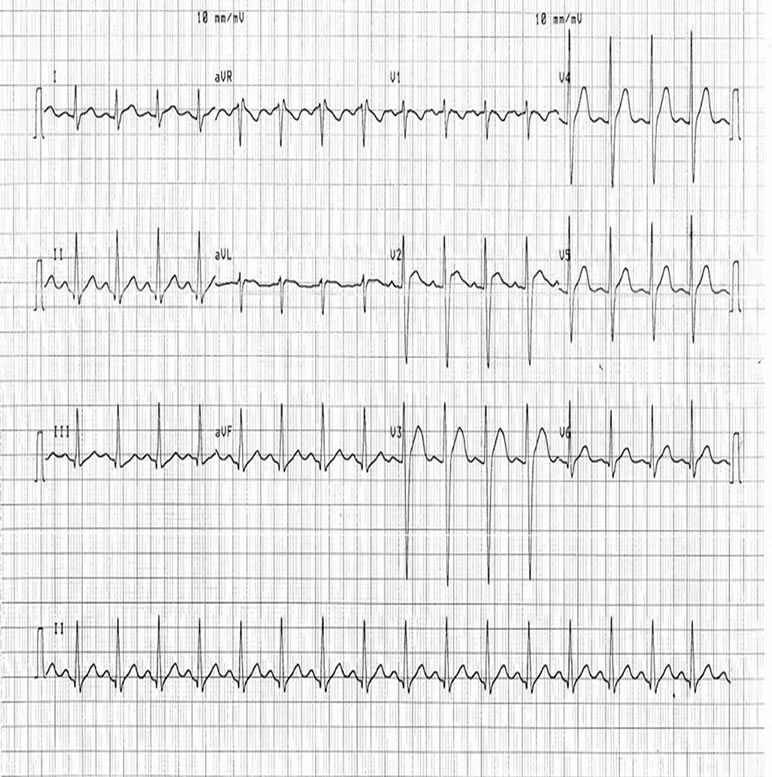 ECG 3
ECG 3 ECG 4
ECG 4
NOTES
*Corresponding author.

