Health
Vol.6 No.5(2014), Article ID:43131,8 pages DOI:10.4236/health.2014.65052
Sexual function in women after delivery: Does episiotomy matter?
![]()
1Unidade de Investigação em Psicologia e Saúde (UIPES), Lisboa, Portugal; *Corresponding Author: ileal@ispa.pt
2ISPA, Instituto Universitário, Lisboa, Portugal
Copyright © 2014 Isabel Leal et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Isabel Leal et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 30 December 2013; revised 3 January 2014; accepted 9 February 2014
KEYWORDS
Episiotomy; Episiorrhaphy; Intact Perineum; Sexual Function; Post-Partum
ABSTRACT
Objective: Despite the fact that a restrictive use of episiotomy has proven to be beneficial, it continues to be widely used in vaginal births. Our aim was to compare women with episiotomy, to women with an intact perineum, 3 months after delivery, regarding several sexual variables, namely: sexual desire, arousal, orgasm, pain, sexual satisfaction and sexual function. Methods: An exploratory, descriptive and quantitative study using a non-probabilistic, convenience sample of 147 Portuguese women, of which 54 belonged to a control group, was performed. The groups were not significantly different regarding sociodemographic aspects. Three instruments were used: the Female Sexual Function Index, a Socio-demographic and Clinical Questionnaire and the Female Sexual Function Questionnaire. Results: Most women mentioned a moderate level of sexual interest. Women with episiotomy present higher pain intensity, less sexual satisfaction, greater changes regarding the orgasm’s duration and intensity, lower levels of sexual arousal and total sexual function, than women with intact perineum. Discussion: We found no significant differences between women with episiotomy and women with an intact perineum in most variables. However, women with episiotomy presented higher levels of pain and a lower sexual satisfaction, being these significant differences.
1. INTRODUCTION
Although episiotomy’s definition is not consensual, some authors suggest that it should include: the place where the incision begins, its direction, length and depth, and the exact moment; the incision was performed [1].
Despite the controversy regarding the validity of episiotomy’s routine use in obstetrics, this is still one of the most performed procedures worldwide [2-4].
The estimated rate of episiotomy is 62.5% in the USA and 30% in Europe [1]. The American College of Obstetricians and Gynecologists [5], the World Health Organization [6], among others [7-9], consider that its routine use is not advised and should be abandoned, recommending a more selective philosophy.
Some studies, which aimed at reducing unnecessary interventions and mother-baby morbidity/mortality, evaluated the routine practice of episiotomy during childbirth. A systematic review concluded that selective episiotomy was associated with a lower risk of posterior perineal trauma, a lower need for suturing and fewer healing complications [10], when compared with routine episiotomy, which causes a bigger blood loss and does not reduce the risk of stress urinary incontinence, dyspareunia and perineal pain [3]. Moreover, some authors mention that, when comparing the restrictive and the routine use of episiotomy, the restrictive policy has shown many benefits, especially regarding the reduction of injuries in the posterior perineum, as well as of the dyspareunia and perineal pain felt after childbirth, which would otherwise impact on the physical, mental and social wellbeing of the mother [7,11].
Impact on Sexual Life
Most studies that assessed the impact of childbirth on female sexual life, focused on the short term physical changes involved, but their results were divergent [12]. However, most authors agree that the couple’s sex life is influenced by the childbirth [13], as spouses have difficulties in harmonizing parental roles and sexual life [14], which leads to a reduction in the frequency, and in the sexual desire, during this transition [9,15,16].
Women justify this decrease/absence of sexual desire with lack of time, fatigue, vaginal lacerations and breastfeeding [14]. References to poor vaginal lubrication and a decrease in the orgasm’s intensity, due to a diminished vasocongestion are common; also, in some women episiotomy affects self-image and therefore the relationship with the partner [15,16].
Based on what we found in the literature, and to help fill the information gap in this area, the aim of this study is to compare women that had an episiotomy/episiorrhaphy with those that have an intact perineum, 3 months after delivery, regarding several variables, namely sexual
desire, arousal, orgasm, pain, sexual satisfaction and sexual function.
2. MATERIALS AND METHODS
2.1. Sample
This sample consisted of 147 Portuguese mothers, hospitalized in the Obstetrics and Gynecology Service of Setubal’s Hospital Center, of these 54 belonged to the control group.
The ages of women with episiotomy were between 21 and 42 years, and of women without episiotomy (control group) were aged between 25 and 43 years. The overall demographic and clinical data was similar, in both groups (Table 1).
The following inclusion criteria were considered: adult puerperal women; having given birth by eutocic delivery;
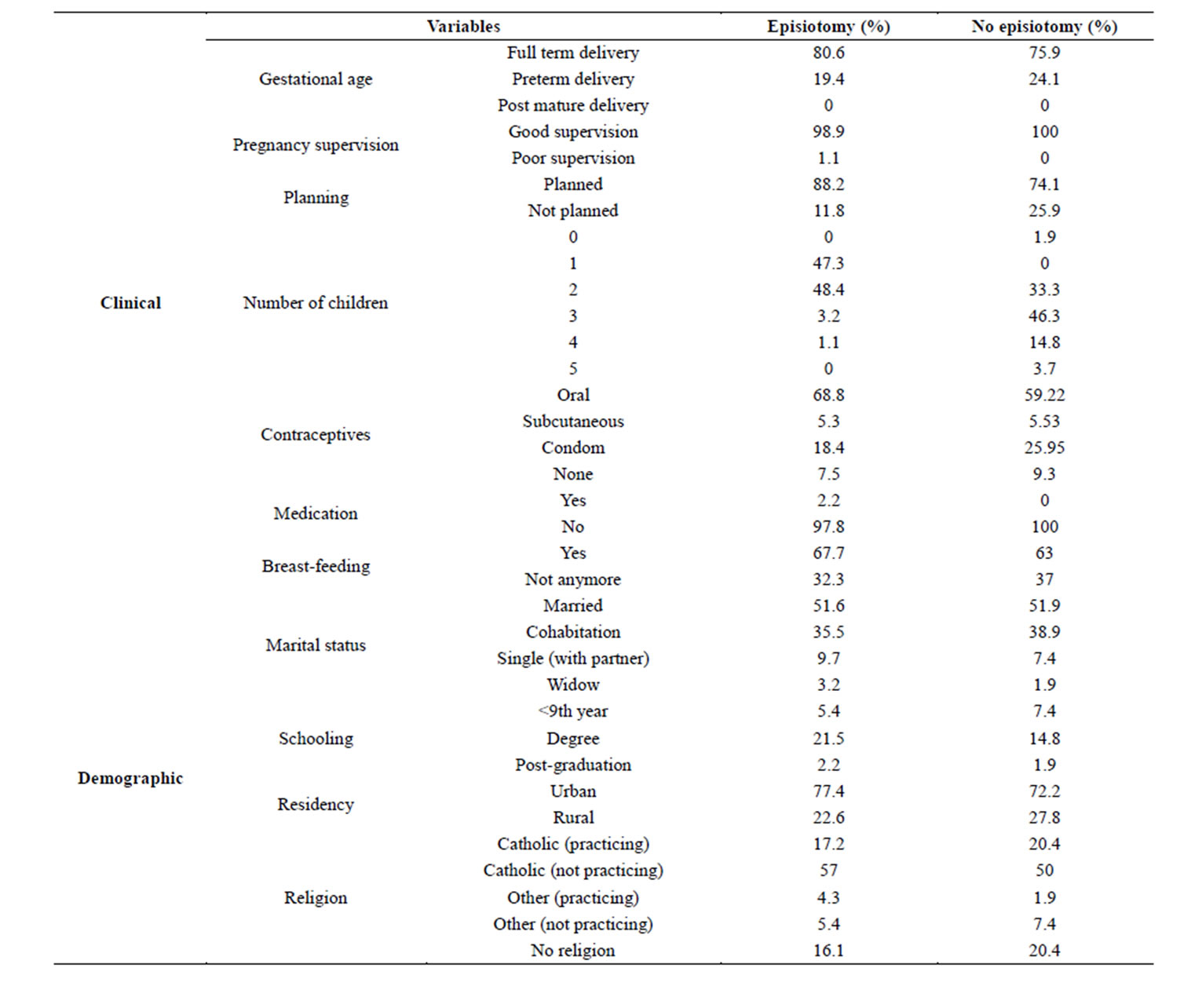
Table 1. Sociodemographic and clinical data.
having had a medio-lateral episiotomy/episiorrhaphy of the perineum; primiparous or multiparous women in the early puerperium; women without any pathological complications during the pregnancy; women without any obstetric complications during the pregnancy or childbirth; women who had a sexual partner during pregnancy and that still maintain the same partner.
The control group met all the inclusion criteria except for having an episiotomy/episiorrhaphy, thus, possessing an intact perineum, without any lacerations.
The aim was to compare both groups, and infer if the presence of episiotomy/episiorrhaphy interferes in the experience of female sexuality three months after childbirth.
2.2. Data Collection Procedures
Data was collected using the Female Sexual Function Index (FSFI), together with two other questionnaires, developed (in the absence of other instruments) for this study.
The FSFI is a 19-item, multidimensional self-report instrument [17], which assess 6 dimensions of the female sexual function: desire, arousal, lubrication, orgasm, satisfaction and pain (dyspareunia), and also provides a total score for the overall sexual function [17,18].
The Socio-demographic and Clinical Questionnaire was developed to gather specific. It has 8 socio-demographic questions, and 11 questions that enabled an obstetric and medical characterization of this sample.
The Female Sexual Function Questionnaire (FSFQ) developed by us [19], with the objective of collecting information regarding the female sexual function. It is a 25-question questionnaire focused on different aspects: sexual behavior, desire/arousal, orgasm, pain, impact of episiotomy on the sexual response and sexual satisfaction (see Table 2 for examples).
After getting the authorization from the Ethics Committee, of Setubal’s Hospital Center, to conduct the study, the questionnaires were distributed between January 20 and June 30, of 2010. All measuring instruments were pre-tested in a group of 19 mothers at the time of discharge from the Obstetrics and Gynecology unit.
120 women with episiotomy and 70 women with an intact perineum were then contacted after childbirth, while hospitalized in the Obstetrics and Gynecology Service of Setubal’s Hospital Center, in order to participate in this study. Thus, 3 months after birth the questionnaires were sent via mail with a pre-paid reply envelope. Of the 170 questionnaires sent out (108 to women with episiotomy, 62 to women with an intact perineum), only 147 (93 of the experimental group, 54 of the control group) were used, as the remaining were not returned or were incomplete.
2.3. Data Analysis Procedures
The differences between both groups were evaluated with t-tests. Data normality was assessed with the Kolmogorov-Smirnov test with Lilliefors correction. We also assumed the robustness of these parametric tests to mild violation of data distribution assumptions for large samples, rather than using non-parametric alternatives. When the variances were heterocedastic, we used the Welch’s correction to the t-test. Statistical significance was assumed for p < 0.05. All statistical analyses were performed with PASW Statistics (v.18, SPSS Inc., Chicago, IL).
3. RESULTS
The FSFI main results showed that, women with episiotomy had identical mean levels of Sexual Desire when compared to women with intact perineum (episiotomy: M = 2.74, SEM = 0.76/intact perineum: M = 2.71, SEM = 0.98) (t(88) = −0.171; p = 0.864) (Table 3).
Regarding Sexual Arousal, women with episiotomy are less sexually aroused, when compared to women with an intact perineum. Despite this, the mean levels remain similar (women with episiotomy: M = 4.48, SEM = 0.11/intact perineum: M = 4.28, SEM = 0.11). The tStudent test revealed no statistically significant differences (t(126) = −1.28, p = 0.20) (Table 3).
Women with episiotomy presented a lower mean level of Vaginal Lubrication than women without episiotomy (episiotomy: M = 3.34; SEM = 0.04/intact perineum: M = 3.42; SEM = 0.04). These differences were not statistically significant (t(129) = 1.47; p = 0.14) (Table 3).
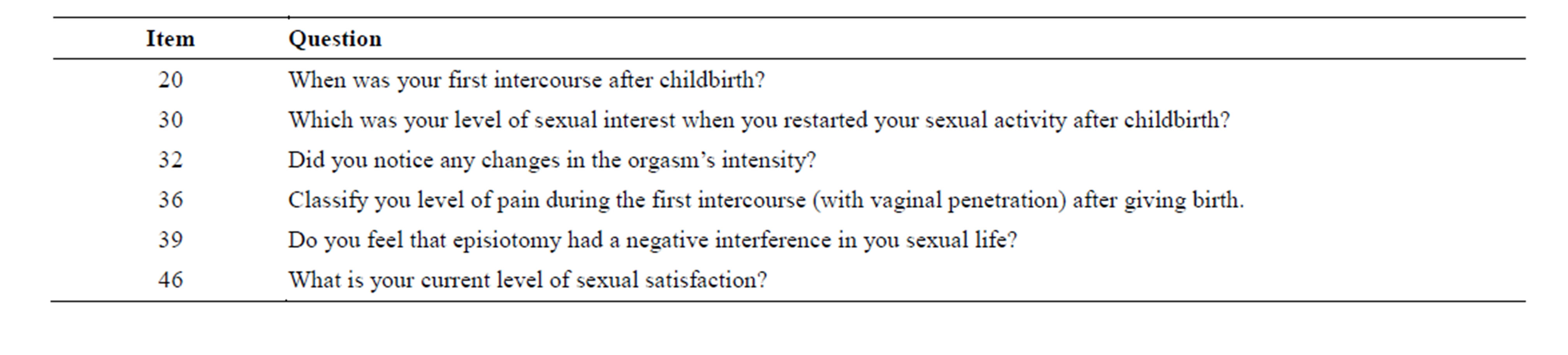
Table 2. Examples of items from the FSFQ.
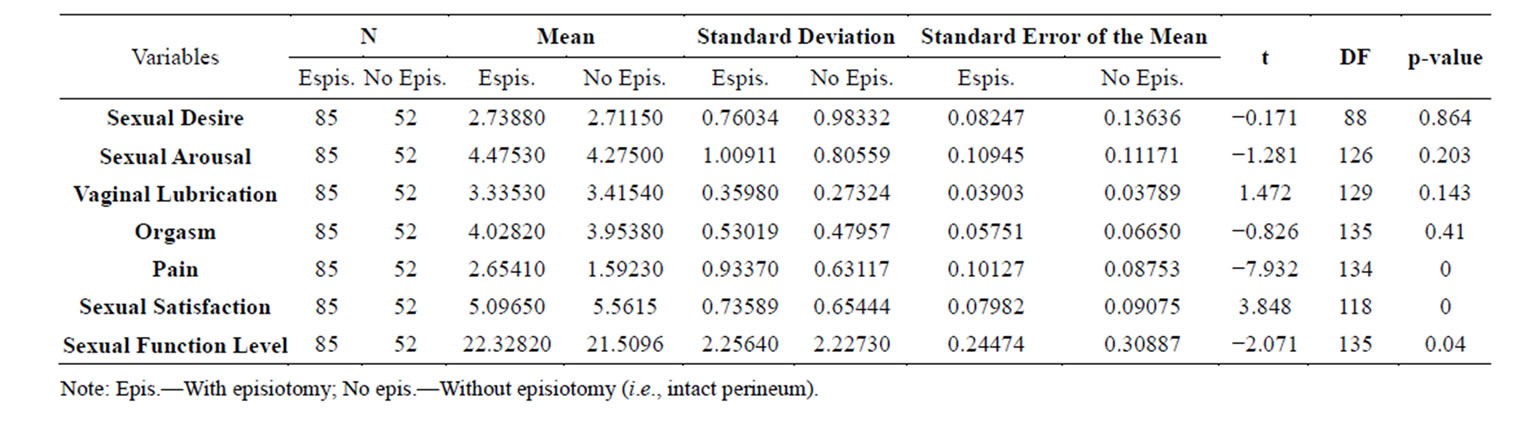
Table 3. Comparison between the group with episiotomy and the group without episiotomy regarding the study’s variables.
The Orgasm was slightly more affected in women with episiotomy than in women without episiotomy (episiotomy: M = 4.02, SEM = 0.06/intact perineum: M = 3.95, SEM = 0.06). However, these differences were not statistically significant (t(135) = −0.83, p = 0.41) (Table 3).
Three months after delivery, women with episiotomy present a higher Pain Intensity (associated to sexual intercourse) than women without episiotomy (episiotomy: M = 2.65, SEM = 0.1/intact perineum: M = 1.59, SEM = 0.09). However, the these differences were not statistically significant (t(134) = −7.93; p < 0.001) (Table 3).
Women with episiotomy have less Sexual Satisfaction than women with intact perineum (episiotomy M = 5.1/intact perineum M = 5.56). These results are significantly different (t(117.6) = 3.85, p < 0.001).
Women with episiotomy had a, only slightly, lower Overall Level of Sexual Function, when compared with women with intact perineum (episiotomy: M = 22.33, SEM = 0.24/intact perineum: M = 21.51, SEM = 0.31), with statistically significant differences between the groups (t(135) = −2.07, p = 0.04) (Table 3).
Regarding FSFQ, the results for Sexual Interest after delivery, most women mentioned a moderate level of interest (episiotomy = 40%/intact perineum = 36.5%). Women without episiotomy had slightly higher percentages in items related to a “high”, “low” or “no” sexual interest, when compared with women with episiotomy (high: 23.1% vs. 20%, low: 30.8% vs. 27.1%, none: 3.8% vs. 2.4%). In contrast, women with episiotomy had a higher percentage regarding “very high” interest in sexual activity (episiotomy = 10.6%/intact perineum = 5.8%).
The results between groups were similar regarding the topics having sexual fantasies “sometimes” (episiotomy = 40.9%/intact perineum = 46.3%) and “few times” (episiotomy = 43%/intact perineum = 37%).
After delivery, most women described no change in the Orgasm’s Intensity (with episiotomy = 60%; without episiotomy = 63%); but the ones that reported changes, mostly described the orgasm as more intense (episiotomy = 82.9%/intact perineum = 75%).
Furthermore, more than half the women from both groups reported feeling no changes in the Duration of the Orgasm (episiotomy = 58.8%/intact perineum = 67.3%). Regarding those that reported changes, most referred that it was “shorter” (episiotomy = 62.9%/intact perineum = 64.7%), although some did mention it was “longer” (episiotomy = 20%/intact perineum = 29.4%). Also, it is interesting to notice that only women from the episiotomy group referred that the orgasm was “much longer” (11.4%).
These results are enhanced when considering the first sexual intercourse after childbirth. Thus, women with episiotomy have more Pain than women with an intact perineum; 25% of women without episiotomy mentioned having “no pain” in this first sexual intercourse, while only 8.2% of the women with episiotomy reported the same. Also 21.2% of the women with episiotomy, and 36.5% of the group without episiotomy, mentioned having a “low intensity” of pain. Furthermore, women with episiotomy present higher percentages in “moderate” pain (41.2%) when compared with women with an intact perineum (30,8%), and also regarding “high” levels of pain (episiotomy = 27.1%/intact perineum = 7.7%). The women with episiotomy were also, the only ones to refer “unbearable” pain (2.4%) (Figure 1). The location of this pain also varies between the groups of women with episiotomy (42.3% stitches and cut) and of women with an intact perineum (42% in the abdomen) (Figure 2).
There are also significant differences in the way Pain interferes with sexual intercourse, for women in both groups. The majority of women with an intact perineum refer that pain “never” (61.5%) “few times” (36.5%) interferes with the sexual intercourse, which is very different from the women with episiotomy, who refer that it interferes “few times” (40%) or “sometimes” (32.9%). Also some women with episiotomy refer that it interferes “often” (5.9%) or “always” (1.2%) (Figure 3).
Both groups reported mostly moderate levels of Sexual Satisfaction, presenting similar results (episiotomy = 41.8%/intact perineum = 46.3%). However, regarding the high and low levels of satisfaction, the differences
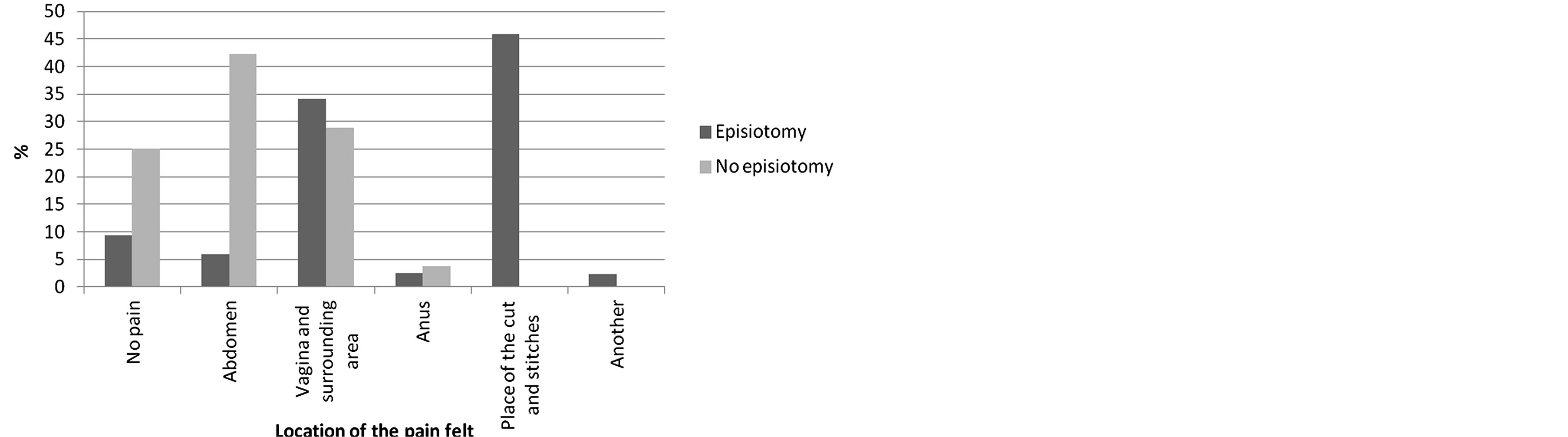
Figure 1. Location of the pain felt in the first postpartum sexual intercourse.
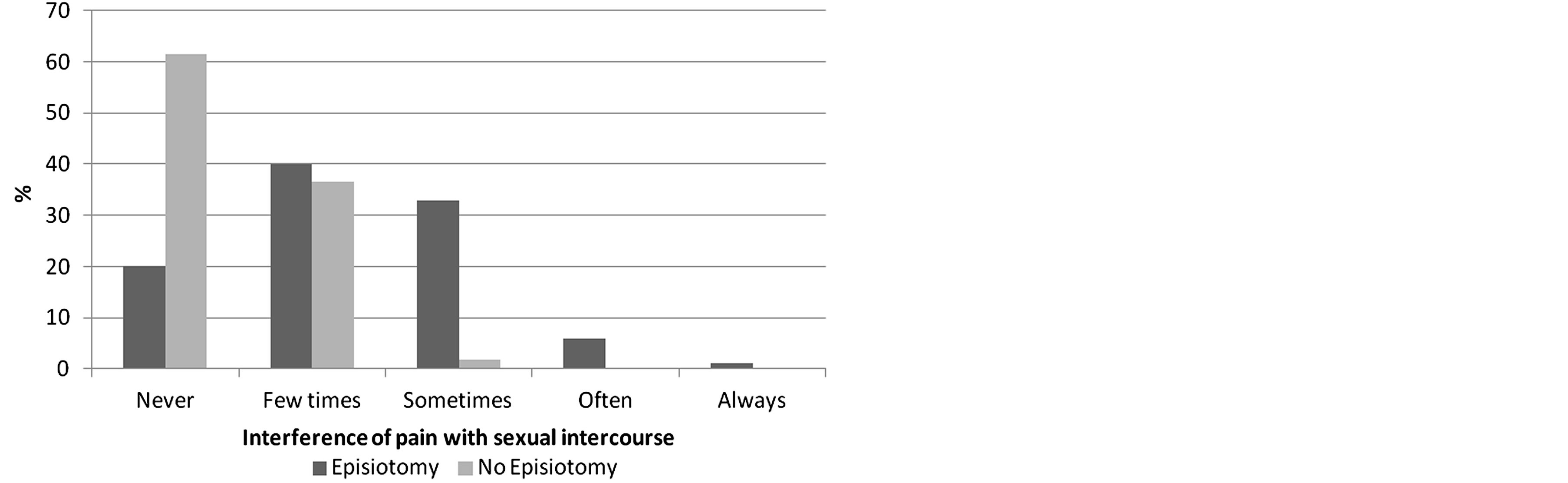
Figure 2. Interference of pain with sexual intercourse.
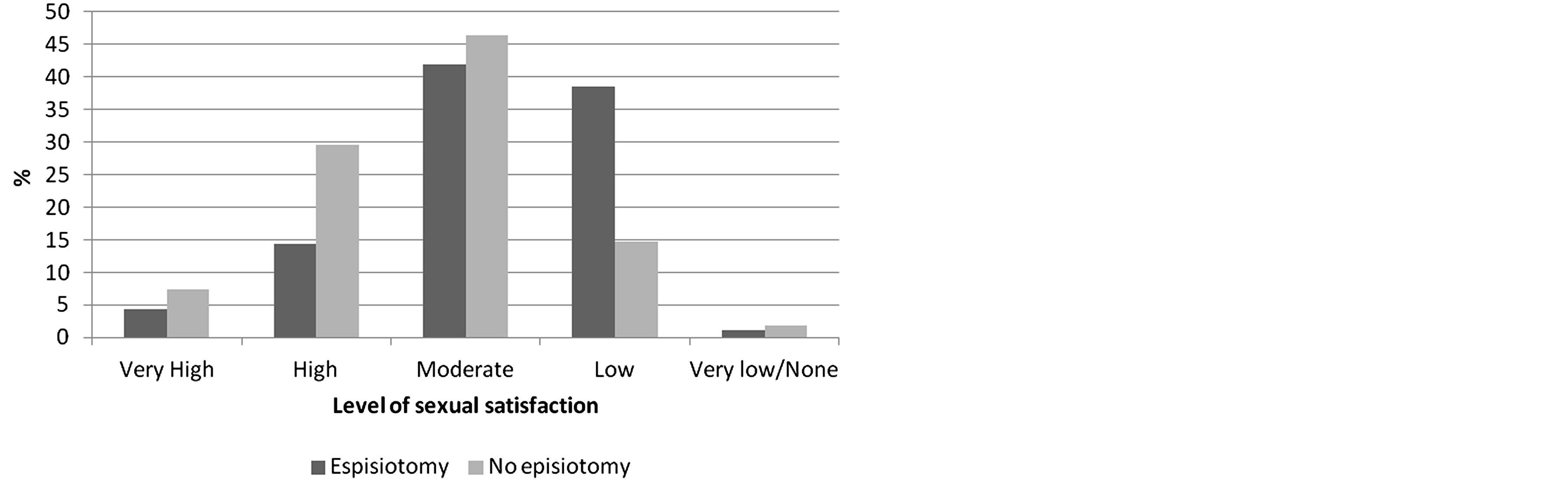
Figure 3. Level of sexual satisfaction.
are clear: women with intact perineum have a higher percentage of “high” satisfaction (with episiotomy = 14.3%/intact perineum = 29.6%), while women with episiotomy refer having a “low” level of satisfaction (episiotomy = 38.5%/intact perineum = 14.8%) (Figure 3).
The sexual life, has a “moderate” importance for most women (episiotomy = 50.5%/intact perineum = 44.4%), presenting no significant differences between both groups. Also, there are no significant differences between sexual life as “very important” (30.8%/31.5%) or “fundamental” (3.3%/3.7%), nor between “of little importance” (12.1%/ 14.8%) or “not important” (3.3%/5.6%).
Furthermore, regarding the importance of sex, the results were very similar, most women attribute to sex a
“moderate importance” (episiotomy = 60.4%/intact perineum = 57.4%). However some differences between groups were found in the “very important” point, being that women with an intact perineum presented higher results (episiotomy = 19.8%/intact perineum = 33.3%), and “of little importance”, where women with episiotomy had higher results (episiotomy = 12.1%/intact perineum = 5.6%). Only a very low percentage from both groups considered sex as fundamental (7.7%/3.7%).
4. DISCUSSION
Regarding Sexual Desire and Sexual Arousal, there were no significant differences between women with and without episiotomy. These results go against previous studies on the subject [15,20].
Also concerning Sexual Interest, the results show no major differences between the two groups, with the exception of the item “very high” interest in sexual activity that is mostly mentioned by women with intact perineum. The existing literature mentions that sexual desire after delivery is adversely affected [15,21]. However, most studies do not compare groups of women with and without episiotomy; only studies that make a comparison between groups of primiparous women with mediolateral episiotomy and women had a cesarean [22].
About the fantasies/erotic dreams, the data seem to show that women, with an intact perineum have erotic dreams or fantasies more often than women with episiotomy, in this sample. There are, however, no studies to prove or counteract these results.
Postpartum Orgasm was not significantly affected by episiotomy. This evidence is in accordance with the results from several studies [23], which mentioned that the ability to reach orgasm is rapidly acquired after delivery. In this sense these authors reported that, six weeks after delivery, most women recover their ability to have orgasms. Moreover, the difficulty in having orgasms is most marked in the three months following childbirth [20]. Von Sydow [24] mentions that during the first intercourse after delivery, only 20% of women can reach an orgasm, while 3 - 6 months after childbirth 75% of women regain pre-pregnancy levels.
Regarding the orgasm, the data show that most women reported feeling no changes to the intensity or duration of orgasm. But, among women who reported changes, the majority mention that it was “shorter”. These findings go against a previous study [25] which reported that, after delivery, the duration of the orgasm diminishes.
The theme of pain/dyspareunia, related to sexual intercourse after delivery, has been widely studied, although the findings are contradictory. This study’s results reveal that, women with episiotomy present pain intensity significantly higher than those without episiotomy. These findings go in the same direction as those of Buhling et al. [26], who concluded that, women with dyspareunia 6 months after childbirth, were more likely to have undergone an episiotomy or vaginal dystocia. In another study it was found that women with intact perineum had less pain than the others [27]. Hartman et al. [8] argue that the pain during intercourse was more frequent in women with episiotomy than those with cesarean, or an intact perineum. Also, Andrews et al. [28] compared women with episiotomy and with perineal lacerations, and concluded that, perineal lacerations cause significantly less pain than episiotomy, being that most women reported perineal pain up to 3 months after childbirth [28].
In contrast, other studies suggest that perineal pain is not influenced by episiotomy; in this sense, Hartman et al. [8] and Botros et al. [12], suggest that episiotomy does not increase the risk of dyspareunia.
Women with episiotomy report higher levels of pain during the first postpartum intercourse with vaginal penetration. This suggests that episiotomy may have a negative influence in terms of the pain experienced by women which does not converge with results from other studies [29] that refer that the levels of pain among women with and without episiotomy, during the first sexual intercourse after childbirth, are very similar.
Considering the location of this pain, the results show that most women with episiotomy refer to having pain on the incision (episiotomy/episiorrhaphy), on the stitches, and in the vagina and surrounding area. In contrast, most women with intact perineum mention pain mainly in the abdomen. Thus, we can conclude that, in this sample, the presence of episiotomy conditioned the location of the pain. Although there is extensive literature that focuses on pain during intercourse in the postpartum, the studies that actually assess the location of that pain are scarce and unspecific, such as the one by Paterson et al. [21], who mentioned that almost all women included in their sample reported genital pain in postpartum period. Of these, 62.5% reported pain in the perineal region and the same percentage of women reported pain in the vagina.
There are significant differences on how pain interferes with sexual intercourse for women with and without episiotomy. Thus, women with episiotomy report that, the pain often interferes with their sexual relations. Based on this, we can conclude that, in this sample, three months after delivery, episiotomy appears to continue having a negative interference on the pain felt during sexual intercourse. The existence of pain in the postpartum period may negatively affect sexual functioning, as is described in a study by Paterson et al. [21], who mention that the pain experienced by women, in this period had a negative (medium to moderate) impact on their sexual function.
Most women (from both groups) reported that their level of sexual satisfaction was “moderate”. Moreover, 1/3 of women without episiotomy reported a “high” level of sexual satisfaction, which is significantly higher than in women with episiotomy. This tendency is opposed to the one observed regarding low levels of sexual satisfaction, where women with episiotomy present the highest rates.
These results suggest that episiotomy interferes negatively in terms of sexual satisfaction, which corroborates the data obtained by Klein et al. [30]. These authors mentioned that three months after delivery sexual satisfaction levels seem to be higher in women with an intact perineum and lower in women with episiotomy. Also, another investigation [27] showed that women with an intact perineum also had higher levels of sexual satisfaction, despite this, the difference in sexual satisfaction, between women with episiotomy and women with perineal lacerations, was not proven.
Some limitations must be considered. The sample size and convenience sampling may limit the generalization of the conclusions to the general population. Also, the use of a non-validated instrument may limit the reliability and validity of the data gathered. However, this was not the only possibility, given the absence of specific instruments validated for this target population.
This study shows that, in general more than half the women, from both groups, believe that sex is of moderate importance in their lives. However, it appears that a greater number of women without episiotomy believe that sex plays a very important role in their lives.
Moreover, it contributes to the further development of knowledge about the actual impact that the episiotomy technique can have in female sexuality. Despite the fact that we did not find significant differences between women with and without episiotomy, in most of the studied variables, we did observe that, women with episiotomy presented higher levels regarding the pain felt (intensity, location) and a lower sexual satisfaction.
REFERENCES
- Kalis, V., Stepan, J.J., Horak, M., Roztocil, A., Kralickova, M. and Rokyta, Z. (2008) Definitions of mediolateral episiotomy in Europe. International Journal of Gynaecology and Obstetrics, 100, 188-189. http://dx.doi.org/10.1016/j.ijgo.2007.07.022
- Löwenstein, L., Drugan, A., Gonen, R., Itskovitz-Eldor, J., Bardicef, M. and Jakobi, P. (2005) Episiotomy: Beliefs, practice and the impact of educational intervention. European Journal of Obstetrics & Gynecology and Reproductive Biology, 123, 179-182. http://dx.doi.org/10.1016/j.ejogrb.2005.04.006
- Mattar, R., Aquino, M.M.A. and Mesquita, M.R.D.S. (2007) A prática da episiotomia no Brasil. Revista Brasileira de Ginecologia e Obstetricia, 29, 1-2. http://dx.doi.org/10.1590/S0100-72032007000100001
- Tomasso, G., Althabe, F., Cafferata, M.L., Aleman, A. and Sosa, C. (2006) The need to avoid the routine use of episiotomy. Current Women’s Health Reviews, 2, 99-102. http://dx.doi.org/10.2174/157340406776931034
- American College of Obstetricians and Gynecologists (2006) ACOG Practise Bulletin nº 71—Episiotomy: Clinical management guidelines for obstetrician-gynecologists. Obstetrics and Gynecology, 107, 957-962.
- Department of Reproductive Health and Research WHO. (2000) Integrated Management of Pregnancy and Childbirth: Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. World Health Organization, Geneva.
- Carroli, G. and Mignini, L. (2009) Episiotomy for vaginal birth. Cochrane Database of Systematic Reviews, 1. http://dx.doi.org/10.1002/14651858.CD000081.pub2
- Hartmann, K., Viswanathan, M., Palmieri, R., Gartlehner, G., Thorp, J. and Lohr, K.N. (2005) Outcomes of routine episiotomy: A systematic review. JAMA: Journal of the American Medical Association, 293, 2141-2148. http://dx.doi.org/10.1001/jama.293.17.2141
- Rathfisch, G., Dikencik, B.K., Kizilkaya Beji, N., Comert, N., Tekirdag, A.I. and Kadioglu, A. (2010) Effects of perineal trauma on postpartum sexual function. Journal of Advanced Nursing, 66, 2640-2649. http://dx.doi.org/10.1111/j.1365-2648.2010.05428.x
- Carroli, G. and Belizan, J. (2007) Episiotomy for vaginal birth. Cochrane Database of Systematic Reviews, 4. http://dx.doi.org/10.1002/14651858.CD000081
- Chang, S.-R., Chen, K.-H., Lin, H.-H., Chao, Y.-M.Y. and Lai, Y.-H. (2011) Comparison of the effects of episiotomy and no episiotomy on pain, urinary incontinence, and sexual function 3 months postpartum: A prospective follow-up study. International Journal of Nursing Studies, 48, 409-418. http://dx.doi.org/10.1016/j.ijnurstu.2010.07.017
- Botros, S.M., Abramov, Y., Miller, J.-J.R., Sand, P.K., Gandhi, S., Nickolov, A., et al. (2006) Effect of parity on sexual function: An identical twin study. Obstetrics & Gynecology, 107, 765-770. http://dx.doi.org/10.1097/01.AOG.0000207677.03235.76
- Lourenço, M.D.C. (2002) Conjugalidade e parentalidade: Continuar a díade na presença de um terceiro. Psychologica, 31, 25-42.
- Colman, A. and Colman, L. (1994) Gravidez: A experiência psicológica. Lisboa Edições Colibri.
- Katz, A. (2010) Sexual changes during and after pregnancy. American Journal of Nursing, 110, 50-52. http://dx.doi.org/10.1097/01.NAJ.0000387693.78241.80
- Ryding, E.-L. (1984) Sexuality during and after pregnancy. Acta Obstetrica et Gynecologica Scandinava, 63, 679-682. http://dx.doi.org/10.3109/00016348409154662
- Rosen, R., Brown, C., Heiman, J., Leiblum, S., Meston, C., Shabsigh, R., et al. (2000) The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex & Marital Therapy, 26, 191-208. http://dx.doi.org/10.1080/009262300278597
- Hentschel, H., Alberton, D.L., Capp, E., Goldim, J.R. and Passos, E.P. (2007) Validação do Female Sexual Function Index (FSFI) para uso em Língua Portuguesa. Revista do Hospital de Clínicas de Porto Alegre, 27, 10-14.
- Lourenço, S., Leal, I. and Carvalheira, A. (2010) Estudo da resposta sexual feminina no período peri-gravídico em mulheres sujeitas a episiotomia episiorrafia. In: Leal, I., Pais-Ribeiro, J., Marques, M. and Pimenta, F., Eds., 8º Congresso Nacional de Psicologia da Saúde, ISPA, Lisboa, 849-858.
- Barret, G., Pendry, E., Peacock, J., Victor, C., Thacker, R. and Manyonda, I. (2000) Women’s sexual health after childbirth. British Journal of Obstetrics and Gynaecology, 107, 186-195. http://dx.doi.org/10.1111/j.1471-0528.2000.tb11689.x
- Paterson, L.Q.P., Davis, S.N.P., Khalifé, S., Amsel, R. and Binik, Y.M. (2009) Persistent genital and pelvic pain after childbirth. The Journal of Sexual Medicine, 6, 215-221. http://dx.doi.org/10.1111/j.1743-6109.2008.01063.x
- Baksu, B., Davas, I., Agar, E., Akyol, A. and Varolan, A. (2007) The effect of mode of delivery on postpartum sexual function in primiparous women. International Urogynecology Journal, 18, 401-406. http://dx.doi.org/10.1007/s00192-006-0280-x
- Connolly, A., Thorp, J. and Pahel, L. (2005) Effects of pregnancy and childbirth on postpartum sexual function: A longitudinal prospective study. International Urogynecology Journal, 16, 263-267. http://dx.doi.org/10.1007/s00192-005-1293-6
- Von Sydow, K. (1999) Sexuality during pregnancy and after childbirth: A metacontent analysis of 59 studies. Journal of Psychosomatic Research, 47, 27-49. http://dx.doi.org/10.1016/S0022-3999(98)00106-8
- Masters, W. and Jonhson, V. (1966) Human sexual response. Churchill, London.
- Buhling, K., Schmidt, S., Robinson, J., Klapp, C., Siebert, G. and Dudenhausen, J. (2006) Rate of dyspareunia after delivery in primiparae according do mode of delivery. European Journal of Obstetrics & Gynecology and Reproductive Biology, 124, 42-46.
- Signorello, L., Harlow, B., Chekos, A. and Repke, J. (2001) Postpartum sexual functioning and its relationship to períneal trauma: A retrospective cohort study of primiparous women. American Journal of Obstetrics and Gynecology, 184, 881-888. http://dx.doi.org/10.1067/mob.2001.113855
- Andrews, V., Thakar, R., Sultan, A.H. and Jones, P.W. (2007) Evaluation of postpartum períneal pain and dyspareunia—A prospective study. European Journal of Obstetrics & Gynecology and Reproductive Biology, 137, 152-156. http://dx.doi.org/10.1016/j.ejogrb.2007.06.005
- Sleep, J., Grant, A., Garcia, J., Elbourne, D., Spencer, J., Chalmers, I. (1984) West Berkshire perineal management trial. British Medical Journal, 289, 587-590. http://dx.doi.org/10.1136/bmj.289.6445.587
- Klein, M., Gauthier, R., Robbins, J., Kaczorowski, J., Jorgensen, S., Franco, E., et al. (1994) Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. American Journal of Obstetrics & Gynecology, 171, 591-598. http://dx.doi.org/10.1016/0002-9378(94)90070-1
LIST OF ABBREVIATIONS
FSFI—Female Sexual Function Index FSFQ—Female Sexual Function Questionnaire

