Health
Vol.5 No.7(2013), Article ID:35111,8 pages DOI:10.4236/health.2013.57156
Internalized symptoms in adolescence as predictors of mental health in adulthood in the Northern Swedish cohort*
![]()
1School of Psychology, University of Adelaide, Adelaide, Australia;
2Department of Public Health and Clinical Medicine, Division of Family Medicine, Umeå University, Umeå, Sweden; #Corresponding Author: karina.nygren@fammed.umu.se
3Department of Clinical Sciences, Division of Child and Adolescent Psychiatry, Umeå University, Umeå, Sweden
Copyright © 2013 Helen R. Winefield et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 25 April 2013; revised 26 May 2013; accepted 21 June 2013
Keywords: Mental Health; Internalizing Symptoms; Adolescence; Middle Adulthood
ABSTRACT
Although mental health symptoms in children and adolescents are shown to predict young adult mental health outcomes, long-term prospective studies of childhood cohorts are few. The aim of the present study was to analyze the prospective importance of internalized mental health symptoms in adolescence for internalized symptoms in adulthood. Methods: A communitybased prospective longitudinal cohort provided information by questionnaire about psychological status at age 16 and 43 (n = 1010, representing 94.3% of those still alive). Socio-demographic variables which were indicative of possible childhood adversity (parental class, absence, illness, unemployment, relationship, crowding, number of moves) were treated as confounders and controlled for in ordinal regression. Results: For both women and men, internalizing mental health symptoms reported at 16 significantly predicted the same outcome at 43 years, after controlling for previous adverse environmental conditions (OR = 1.2 for women, 1.3 for men). Conclusion: In this representative cohort studied over 27 years with excellent retention rates, the occurrence of self-reported worry, panic and sadness in mid-adolescence significantly increased the likelihood of similar states in middle adulthood.
1. INTRODUCTION
Adolescent depression and anxiety can predict mental health problems in early adulthood [1]. However, there is overall a lack of long-term cohort studies within the field. In addition, the available studies have methodological shortages which need to be addressed such as variations in mental health definitions, relatively short periods of follow-up, lack of analyses of important confounders, various criteria for sample selection and most importantly high attrition rates [1]. Most longitudinal studies covering the span from childhood to adulthood face representativeness problems as attrition rates are often between 30% - 70% [2]. A high response rate is crucial as those with poor mental health are notoriously difficult to reach and study in both epidemiological and clinical studies.
Categorical classification of depression and anxiety in adolescents by use of ICD/DSM diagnostic systems, whether in clinical or population based samples, shows a rather strong prediction of adult psychopathology [3,4]. Interestingly, even sub-threshold depression predicted adult depression in these studies. Confining studies to cases of psychiatric disorders which have been diagnosed by experts raises the risk of under-detection in epidemiological community studies. But valuable information can be gained from self-reports of mental health problems. These measures often have a dimensional approach such as internalizing symptoms (e.g. depressive, anxiety symptoms) and externalizing symptoms (acting-out behavior), especially in studies of mental health in young populations [5]. Non-clinical levels of distress are responsible for significant reductions in quality of life and interference with the developmental tasks of adolescence such as peer relationships and academic progress [3]. In a Dutch study [6], where 2400 children from the general population aged 4 - 16 years were followed in seven waves in a 24 year follow-up (1983-2007), internalizing and externalizing symptoms were measured by use of the ASEBA [7,8] questionnaires. The internalized symptom dimension predicted internalized symptoms (OR = 1.8) and externalized symptoms predicted externalized symptoms (OR = 1.6). The response rate at the seventh data collection was 67%. An additional pitfall (other than high non-response rates) in longitudinal studies is difficulty in using identical assessment methods in all ages through the course of the study. In the above mentioned ZuidHolland study, parental reports were used at ages before 19 years, while self-reports were used in adults. A third methodological challenge in longitudinal research is to consider relevant confounders. Socio-economic and environmental influences on both early and adult mental health are necessary to control for as possible confounders. Such confounders include parental socioeconomic position [9], parental divorce, parental sickness, severe childhood trauma as well as housing tenure and crowded living conditions [10,11].
The aim of our present study was to analyze the prospective importance of internalized mental health symptoms in adolescence on internalized symptoms in adulthood, in a large community-based cohort with excellent retention. The benefits of our study are the long follow-up time from mid-adolescence to early middle age, a representative sample, using the same self-report symptom questionnaire at baseline and follow up, and the exploration of the role of socio-demographic factors as confounders of the relationship between adolescent and adult symptoms. Thus, we supposed the study would add important knowledge in predicting adult outcome of mental health problems in adolescence.
2. STUDY POPULATION AND DESIGN
2.1. Population
The Northern Swedish Cohort consists of all pupils (n = 1083) who in 1981 attended the last year of compulsory school (age 16) in all nine schools in a middle-sized municipality in Northern Sweden. The cohort has proven to be representative for the country as a whole with regard to among other variables both socio-demographics and self-reported health status [12]. At the 27-year follow-up 94.3% (n = 1010, 522 men, 488 women) of those still alive of the original cohort continued to participate. Due to non-response in main variables, the effective sample size of the present study is n = 985 (92% response rate, n women = 476, n men = 509).
2.2. Follow-Up
The cohort has so far been followed up five times of which two (age 16 in 1981 and age 43 in 2008) will be used in this study. The main data source has been extensive questionnaires. Standardized scales covered the broad areas of somatic and mental health, externalizing behaviors, other health behaviors, exhaustion, time of puberty, school/work environment, labor market history and position, education, material and psychosocial life conditions [12].
2.3. Measures
2.3.1. Dependent Variable
The dependent variable is a measure of internalized mental health symptoms at age 43. Questions derived from validated measures [12] were used to form a composite index based on a clinical evaluation of the seriousness of both the single symptoms and also the combinations of symptoms.
Respondents were asked if they had experienced any nervous problems in the past 12 months. Two of these nervous problems were worry/anxiousness and anxiety/ panic. These were both binary variables coded as no = 0 and yes = 1. The respondents were also asked how often, in the past 12 months, that they had experienced sadness or feeling low. This was a 4-grade ordinal scale variable coded as never = 0, sometimes = 1, often = 2, always = 3. Based on these three variables, an ordinal scale index was created, ranging from 0 = not experiencing any symptoms to 8 = having worry/anxiousness, anxiety/ panic and often or always feeling sad and low (see Table 1).
2.3.2. Earlier Health Status
A measure of internalized mental health symptoms at age 16 was used as the main independent variable. It was created in an identical manner as the corresponding dependent measure at age 43 (as described above). For cross tabulations, the variables internalized mental health symptoms at both age 16 and 43 were assigned to categories as follows: 0 = low level, 1 = 1 (medium level), 2 = 2 or more (high level).
2.3.3. Confounders at Age 16
All confounders were retrieved from the 1981 questionnaire when the participants were 16 years old. These reflect socio-demographic and family relationship factors potentially affecting internalizing symptoms at both age 16 and 43.
Parental class. Answers to two questions regarding father’s and mother’s occupation at 16 years of age were combined into a new variable coded as 0 = no workingclass parent, 1 = one working-class parent and 2 = two working-class parents, according to a Swedish classification system of socio-economic status [13].
Parental illness. Answer to two questions regarding
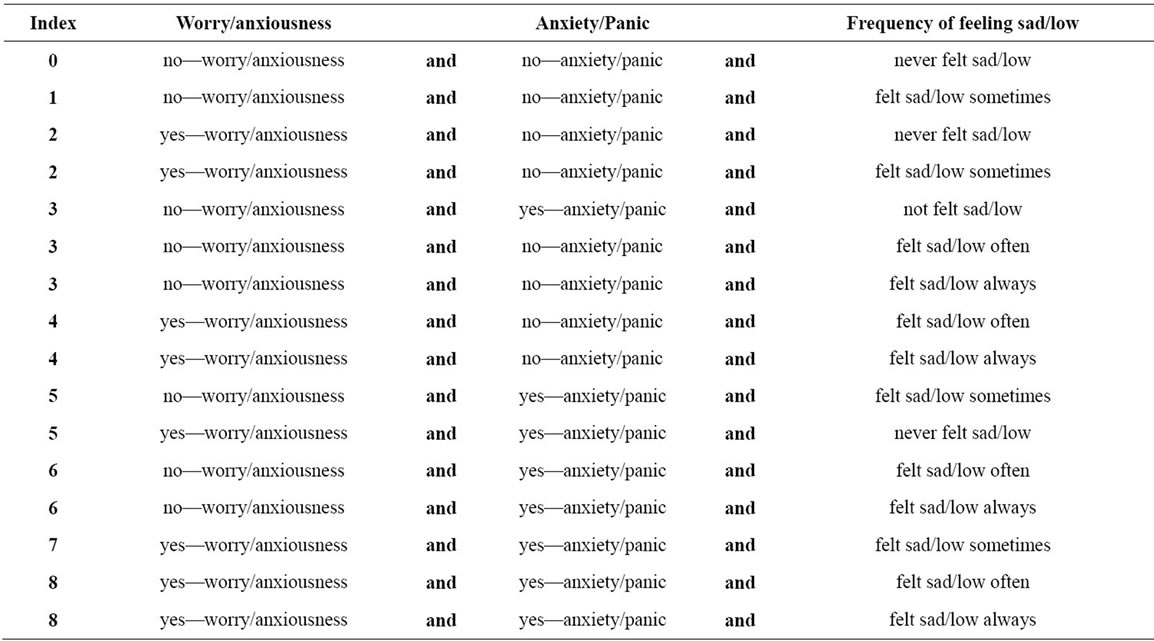
Table 1. Internalized mental health symptoms index (range 0 - 8). Detailed description of where each combination of the three variables included in the index have been placed within this index.
father’s and mother’s health status at age 16 were dichotomized into the parent having/not having a physical or mental illness, then summarized into a combined variable coded as 0 = neither mother nor father had illness, 1 = mother or father had illness and 2 = both parents had illness.
Parental divorce/death. Participants reported on their parents’ marital status and possible death. These variables were combined in a dichotomous variable, coded as 0 = parents married and 1 = parents divorced or one/both parents had passed away.
Relationship with parent. The adolescents were asked to report on how they experienced their relationship with their mother and father, respectively. These were 5-point Likert scale questions ranging from 1 = very good to 5 = very poor. Both variables were dichotomized as 0 = having a very good relationship and 1 = having a good, neither good nor poor, poor or very poor relationship. The two variables were combined into a composite measure, coded as 0 = good relationship with both parents, 1 = poor relationship with one parent and 2 = poor relationship with both parents.
Crowded living situation. At age 16, the participants were asked how many rooms their home had and how many people were living in their home. From these, a measure of crowded living space was created.
Unemployment in the family. Unemployment in the family was measured with a single variable, a question in which the adolescents were to report if any family member had been unemployed within the previous 12 months. This variable was coded as 0 = no and 1 = yes.
Number of moves. The variable is based on a question concerning how many times, during the participant’s lifetime, that the family had moved (so far that he/she had to seek new friends). This was a 5-point Likert scale variable ranging from 0 = has never moved to 4 = has moved more than 10 times.
2.4. Statistical Methods
We tested the following possible confounders: parental socio-economic status, parents born abroad, crowded living conditions, unemployed parents, poor contact with parents, parental sickness, parental divorce and number of moves. The following variables were significantly related to both internalized mental health symptoms at both age 16 and at age 43 and were therefore included as confounders in the regression analyses: crowded living conditions, unemployed parents, poor relationship with parents, parental sickness, parental divorce, number of moves. The correlation between the confounders was <0.3.
For the statistical analyses, the proportional odds model was used. Ordinal regression was chosen as the method for the statistical analyses as the dependent variable had an ordinal scale. The analyses were first performed separately for the main independent variable, after which all confounders were added in the multi-variate analysis. A significance level of <0.05 was chosen and all analyses were performed separately for men and women. The estimates (log odds) were transformed into odds ratios.
3. RESULTS
Table 2 shows the distribution of all included variables. Scores measuring internalized mental health symptoms at ages 16 and 43 range from 0 - 8. For both men and women, the distribution of both variables is skewed: the majority of respondents experienced either no symptoms or only occasional sadness/feeling low. Internalized mental health symptoms were significantly more frequent for women than men, both at age 16 and 43. Also, there was an increase in symptoms from age 16 to age 43 among both men and women.
Parental class was evenly distributed. About one third of the pupils reported illness in at least one parent. About one fourth had experienced parental divorce/death. Two thirds had very good relations with both parents. Very few had crowded living conditions. About one fifth of the pupils had unemployed family members.
Figures 1(a) and (b) show the distribution of internalized symptoms at age 16 as compared to age 43 among men and women. There was a shift in symptoms duringthe 27-year follow-up among both men and women, with higher frequencies of both zeros and values above 1.
Table 3 illustrates how those with no, one and more than one symptom of internalized psychological symptoms at age 16 are distributed 27 years later (in row per cent). Among men, those 16 years old with no symptoms had the most stable situation, 69% still had low level at age 43, while 19% had more than one symptom. Of those with most symptoms in adolescence, 44% still had high levels 27 years later, while 37% had low levels. The most unstable group was those with one symptom. A similar trend was found among women but fewer (55%) of those with no symptoms at age 16 continued to have low levels at age 43 while 21% had moved to the highest level group. A poorer prognosis than among the men resulting in a more stable situation was found among women with highest levels of symptoms in adolescence: 51% still had highest levels, while 31% had no symptoms.
Table 4 shows the results of the ordinal regression analyses. The univariate analysis showed that experienc-
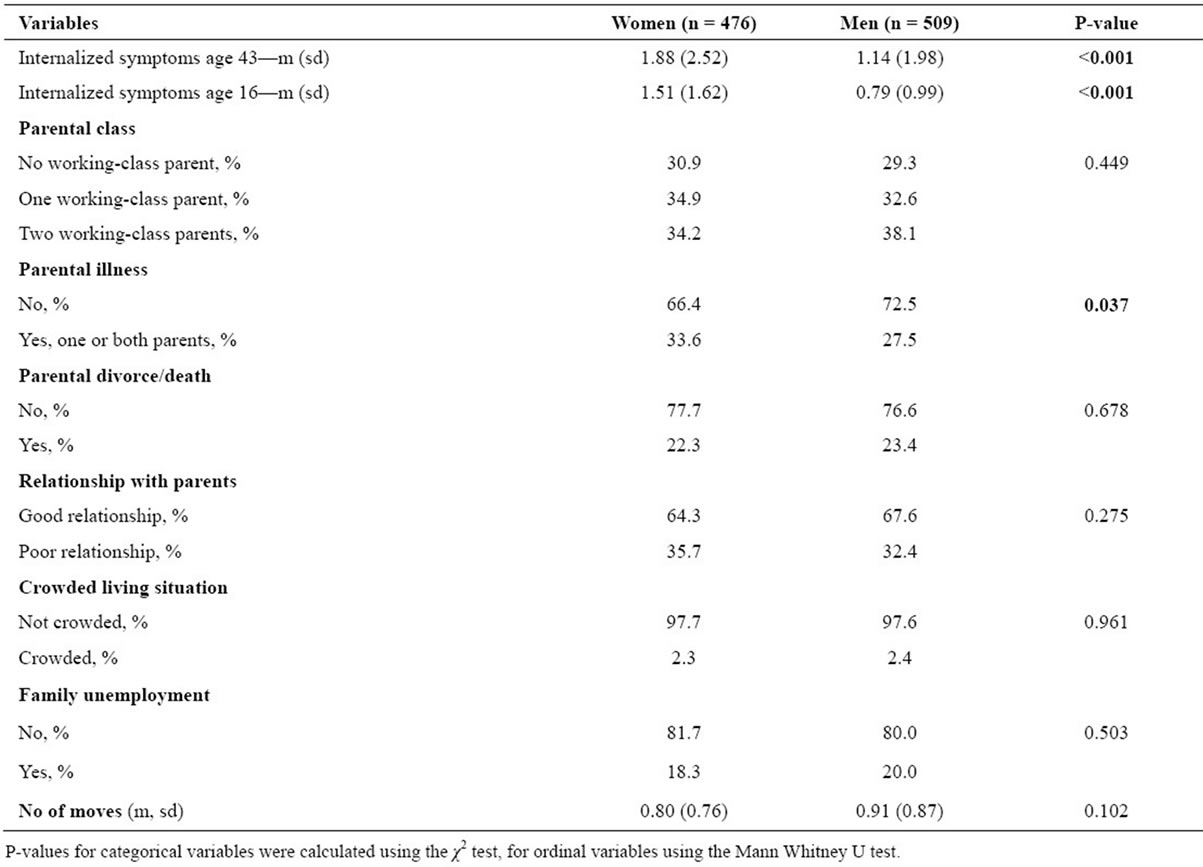
Table 2. Distribution of dependent and independent variables among women and men. Significance level at 0.05.
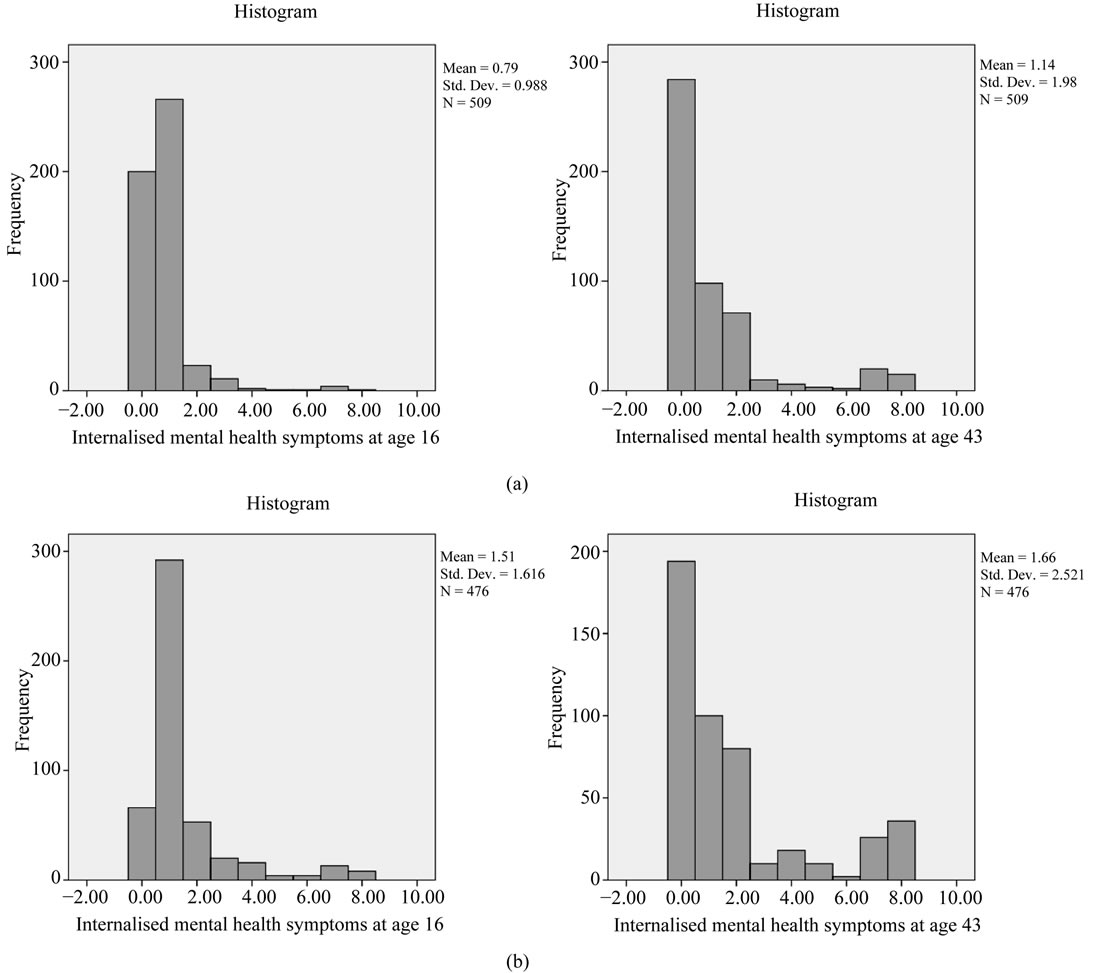
Figure 1. (a) Histogram of distribution of internalized psychological symptoms at age 16 as compared to age 43 among men; (b) Histogram of distribution of internalized psychological symptoms at age 16 as compared to age 43 among women.

Table 3. Various levels of internalized psychological symptoms (no symptom, one symptom, two or more symptoms) at age 16 in relation to the same levels at age 43. Row percent. Separate analysis for men and women. P-value men: <0.001, P-value women: 0.002.
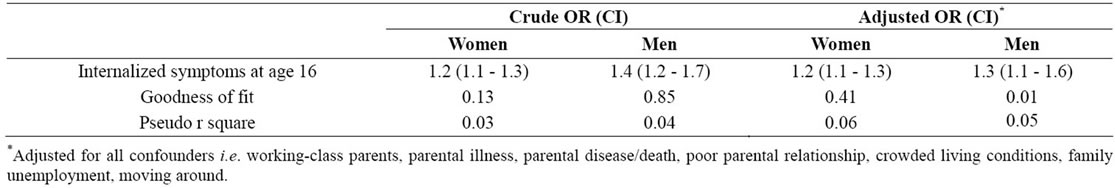
Table 4. Ordinal regression analysis. Crude and adjusted odds ratios (OR) and 95% confidence intervals (CI) for internalized symptoms (women and men) at age 43.
ing internalized symptoms at age 16 was significantly related to experiencing the same symptoms 27 years later. In the multivariate analysis, this correlation was still significant although several confounders were controlled for. Experiencing internalized mental health symptoms at age 16 significantly increased the odds ratio of experiencing the same symptoms at age 43, for women by 1.2 times and for men by 1.3 times. Statistically controlling for adverse adolescent environment did not affect the odds ratio for women, and decreased it somewhat for men.
In the adjusted model, only one confounder was significantly related to the outcome. For women, parental illness/death at age 16 increased the odds ratio of internalized symptoms at age 43 with 1.5 times. The high goodness of fit in the crude analyses among men was weakened after control for confounders. Overall, the goodness of fit was acceptable in all other analyses. Pseudo R squares (Nagelkerke) indicate that between 3 and 6 percent of the variance was explained by our model.
4. DISCUSSION
The Northern Swedish Cohort is a representative community-based sample and there has been excellent retention of participants over the study’s long duration. Our results showed that the odds of moving one step in internalized symptoms at age 43 increases by 30% among men and 20% among women when moving one step higher on the symptom scale at age 16. Controlling for a range of adverse socio-demographic confounders in adolescence did not affect the odds ratio for women but slightly decreased it for men. In spite of these consistent results we also found another picture with quite high degree of participants moving from various symptom loads. Thus, there is a need for further research on movements between trajectories of mental health development from adolescence until adult age.
The predictive power of internalizing disorders in mid-adolescence for similar disorders in middle adulthood is congruent with other prospective longitudinal research reports, few of which however have followed their adult cohorts past their 30’s. The odds ratios found in our study were similar to those found in other studies on self-reported symptoms [6] but lower compared to studies in which structured diagnostic interviews are performed at baseline [4]. One study with an exceptionally long follow-up is the 45-year follow-up of the British Birth Cohort [14], which found similarly that persistent internalizing problems in late adolescence and early adulthood are predictive of mid-life disorders. Further, they found as we did that men showed a stronger relationship between malaise in early adulthood and mid-life diagnoses than did women. The interesting gender-related finding needs to be further analyzed in future research posing the question about mechanisms and other explanations to why mental disorders seem to have less continuity among women.
The implication of our main findings for service delivery is that self-reported worry and sadness during adolescence is a marker for similar forms of psychological distress in middle age. This bolsters arguments for efforts at early detection and treatment of the adolescent with internalizing problems, who may not as readily come to the attention of teachers and parents compared with the individual showing externalizing (conduct and acting-out) problems [15].
The finding that socio-demographic factors indicative of adverse environment reduce rather than increase the predictiveness of adolescent problems for men, is an intriguing one and calls for further analyses. Other studies exploring adversity in youth have found the strongest effects for abuse and neglect [10,11,16], severe and relatively rare circumstances which were not measured here. In addition, it may be relevant to look more widely at adulthood mental health outcomes, beyond the internalizing symptoms only. There is a need for more analyses of the predictive power of internalizing early symptoms on a wide range of mental health symptoms.
4.1. Strengths and Limitations
The main strength of our study is the exceptionally high response rate over a long period of time in the Northern Swedish Cohort. Several socio-demographic factors were tested but only those which turned out to be confounders were included in the final analyses.
The measure of internalized symptoms needs to be discussed. Depression is one of the best-studied predictors of later mental health conditions, but the high comorbidity of depressive with anxiety disorders makes it attractive to aggregate these internalizing conditions. According to the “tripartite” model depression and anxiety are closely related which is a further argument for using them in the same dimension which is also the case in the internationally well-known ASEBA scales [5,17]. Our measure is based on a clinical judgment of both occurrence and severity of the symptoms. Often less noticeable to teachers and parents than are conduct disorders, adolescent internalizing symptoms in the form of experiences of worry, panic and sadness are important as precursors to adult distress as well as in their own right. As compared to medical diagnoses, self-reported mental illness may represent less precise but more common conditions.
It is likely that by maintaining a focus on internalizing disorders, our findings under-represent the prevalence of the complete range of disorders in adulthood which are predicted by internalizing disorders at 16. Likewise, the prediction of internalizing disorders at age 43 might be strengthened by widening the scope of symptoms at age 16 that are explored as predictors. Kim-Cohen et al. (2003) found by following back 26-year-old adults diagnosed with mental disorders, in a longitudinal cohort with 96% retention, that adult disorders were generally preceded by their juvenile counterparts, but also by different disorders [18]. Similarly to the findings of Copeland et al. (2009), childhood conduct or oppositional defiant disorder was part of the developmental history of every adult disorder [18,19].
4.2. Conclusion
In conclusion, these results, being free from methodological weaknesses of unrepresentative samples, different assessment methods, short follow-ups and poor retention, demonstrate the prediction of adult internalizing disorders from those reported in adolescence. In doing so, the results emphasize the potential preventive health benefits of having procedures in place to notice and offer interventions to adolescents distressed by anxiety and depression. Social position and family environment seem to have limited confounding effects on the relation between adolescent and adult internalizing symptoms. Thus, health promotion could preferably use the school as an arena in preventive work.
![]()
![]()
REFERENCES
- Fryers, T. and Brugha, T. (2013) Childhood determinants of adult psychiatric disorder. Clinical Practice and Epidemiolgy in Mental Health, 9, 1-50. doi:10.2174/1745017901309010001
- Gustavson, K., von Soest, T., Karevold, E. and Roysamb, E. (2012) Attrition and generalizability in longitudinal studies: Findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health, 12, 918. doi:10.1186/1471-2458-12-918
- Fergusson, D., Horwood, L., Ridder, E. and Beautrais, A. (2005) Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry, 62, 66-72. doi:10.1001/archpsyc.62.1.66
- Jonsson, U., Bohman, H., von Knorring, L., Olsson, G., Paaren, A. and von Knorring, A.L. (2011) Mental health outcome of long-term and episodic adolescent depression: 15-year follow-up of a community sample. Journal of Affective Disorders, 130, 395-404. doi:10.1016/j.jad.2010.10.046
- Achenbach, T.M., Rescorla, L.A. and Ivanova, M.Y. (2012) International epidemiology of child and adolescent psychopathology I: Diagnoses, dimensions, and conceptual issues. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 1261-1272. doi:10.1016/j.jaac.2012.09.010
- Reef, J., Diamantopoulou, S., van Meurs, I., Verhulst, F. and van der Ende, J. (2009) Child to adult continuities of psychopathology: A 24-year follow-up. Acta Psychiatry Scandinavica, 120, 230-238. doi:10.1111/j.1600-0447.2009.01422.x
- Achenbach, T.M. (1991) Manual for the child behavior checklist/4-18 and 1991 child profile. University of Vermont, Burlington.
- Achenbach, T.M. (2003) Manual for the ASEBA adult forms & profiles. University of Vermont, Research Center for Children, Youth & Families, Burlington.
- Stansfeld, S., Clark, C., Rodgers, B., Caldwell, T. and Power, C. (2011) Repeated exposure to socioeconomic disadvantage and health selection as life course pathways to mid-life depressive and anxiety disorders. Social Psychiatry and Psychiatric Epidemiology, 46, 549-558. doi:10.1007/s00127-010-0221-3
- Clark, C., Caldwell, T., Power, C. and Stansfeld, S. (2010) Does the influence of childhood adversity on psychopathology persist across the life course? A 45-year prospective epidemiologic study. Annals of Epidemiology, 20, 385-394. doi:10.1016/j.annepidem.2010.02.008
- Green, J.G., McLaughlin, K.A., Berglund, P.A., Gruber, M.J., Sampson, N.A., Zaslavsky, A.M., et al. (2010) Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication i: Associations with first onset of dsm-iv disorders. Archives of General Psychiatry, 67, 113-123. doi:10.1001/archgenpsychiatry.2009.186
- Hammarström, A. and Janlert, U. (2012) Cohort profile: The Northern Swedish cohort. International Journal of Epidemiology, 41, 1545-1552. doi:10.1093/ije/dyr118
- Statistics Sweden (1983) Swedish socio-economic classification (in Swedish). Stockholm.
- Clark, C., Rodgers, B., Caldwell, T., Power, C. and Stansfeld, S. (2007) Childhood and adulthood psychological ill health as predictors of midlife affective and anxiety disorder. Archives of General Psychiatry, 64, 668-678. doi:10.1001/archpsyc.64.6.668
- Papandrea, K. and Winefield, H. (2011) It’s not just the squeaky wheels that need the oil: Examining teachers’ views on the disparity between referral rates for students with internalizing versus externalizing problems. School Mental Health, 3, 222-235. doi:10.1007/s12310-011-9063-8
- Reinherz, H., Paradis, A., Giaconia, R., Stashwick, C. and Fitzmaurice, G. (2003) Childhood and adolescent predictors of major depression in the transition to adulthood. American Journal of Psychiatry, 160, 2141-2147. doi:10.1176/appi.ajp.160.12.2141
- Clark, L.A. and Watson, D. (1991) Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100, 316-336. doi:10.1037/0021-843X.100.3.316
- Kim-Cohen, J., Caspi, A., Moffitt, T.E., Harrington, H., Milne, B.J. and Poulton, R. (2003) Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry, 60, 709-717. doi:10.1001/archpsyc.60.7.709
- Copeland, W., Shanahan, L., Costelo, J. and Angold, A. (2009) Which childhood and adolescent psychiatric disorders predic which young adult disorders? Archives of General Psychiatry, 66, 764-772. doi:10.1001/archgenpsychiatry.2009.85
NOTES
*This study has been funded by Formas, dnr 259-2012-37.

