Journal of Diabetes Mellitus
Vol.05 No.04(2015), Article ID:60911,6 pages
10.4236/jdm.2015.54035
Effect of Carbon Dioxide Therapy on Diabetic Foot Ulcer
Naeem Shalan, Abdulrahman Al-Bazzaz, Israa Al-Ani*, Fadi Najem, Mohammad Al-Masri
Faculty of Pharmacy and Medical Sciences, Al-Ahliyya Amman University, Amman, Jordan

Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).


Received 25 September 2015; accepted 2 November 2015; published 5 November 2015

ABSTRACT
Ulceration of diabetic foot represents one of the most concerning complications associated with uncontrolled blood sugar in diabetes mellitus. The aim of this study is to evaluate the condition of twenty-two diabetic patients with different degrees of ulceration in their feet after daily secessions of carbon dioxide therapy. Blood flow to the affected foot was measured by Doppler; also the size, color, degree of ulceration and sensation of the ulcerative area were all evaluated. Results showed improvement of blood flow to the affected foot as well as improvement in the sensation and color of the ulcerative area. It was concluded that carbon dioxide therapy of diabetic foot was promising and needed thorough investigation to be brought widely into application.
Keywords:
Diabetic Foot Ulcer, Carbon Dioxide Therapy

1. Introduction
Diabetes mellitus (DM) is a metabolic disorder resulting from a defect in insulin secretion, insulin action, or both. Insulin deficiency leads to chronic hyperglycaemia with disturbances of carbohydrate, fat and protein metabolism [1] - [4] . As the disease progresses, tissue or vascular damage ensues leading to severe diabetic complications such as retinopathy [5] [6] , neuropathy [7] [8] , nephropathy [9] [10] and cardiovascular complications [11] [12] . All these might end up with and foot ulceration which could be a serious problem that needs foot amputation [13] [14] .
Foot infection is a common problem with diabetes mellitus. It is a complex problem that is associated with admission of patient to hospitals [14] . Acute foot infection is usually caused by gram positive bacteria like Staphylococcus aureus and streptococci [15] . However, chronic infection is associated with anaerobic bacteria specially Pseudomonas aeruginosa and Clostridium bochili [16] [17] .
Previously, management of diabetic foot infection involved the restoration of fluid and electrolytes balance, blood sugar, acidosis and azotemia if occurred [18] . In addition an antibiotic might be prescribed. The selection of the antibiotic might be based on the culture result to cover the microorganisms involved. The treatment may start parenterally to ensure high concentration of drug especially at the beginning [19] . Penicillins, cephalosporines, floroquines and cardapenes are examples of antibiotics prescribed in management of diabetic foot infection [20] .
Hyperglycemia is associated with neuropathy, connective tissue changes, angiopathy involving macroangiopathy (atherosclerosis) and microangiopathy. Foot infection is one of serious complications associated with poor controlled diabetes mellitus [21] .
Carboxytherapy is the use of CO2-rich water bathing which was developed in France in 1930. It was found that CO2 helped in wound healing and fat accumulation in arteries [22] . The effect of CO2 enriched water lies primarily in the vasodilitation which is due to the increase in nitrous oxide formation by CO2 leading to vasodilatation and release of growth factor for angiogenesis which increases oxygen delivery to the area [23] .
The same principle is applied in the treatment of diabetic foot ulceration. Increase delivery of CO2 to the ulcerated area will generate nitrous oxide liberation that will mediate the sequence of events that end up with increase oxygen and blood flow to the ulcerated foot [24] . The improved angiogenesis and oxygenation will result in healing of the ulceration.
The objective of this work is to evaluate twenty-two diabetic patients in Jordan who have foot ulcers and take carbon dioxide therapy as daily sessions each for 30 minutes for two weeks in terms of ulcer area and blood flow to the foot.
2. Methodology
Artificial carbon dioxide containing water for foot bathing was generated using Carbothera® (Mitsubishi Rayon engineering com. Ltd.). The concentration of CO2 used was 1000 ppm and the water temperature was 37˚C. Volume of water in the chamber was 2 liters enough to immerse the patient’s foot.
Twenty?two diabetic patients (14 males and 8 females, age 45 - 65 years) suffered from ulceration in their feet participated in this study. Different methods including prescribing antibiotics had failed to treat their infected ulcerative feet. Their ulcerative feet were examined and evaluated before and after CO2 therapy.
The patients immersed their feet in a disposable bag containing carbon dioxide (1000 ppm) dissolved in water at 37˚C for 30 minutes each session. Then the plate of the device was cleaned by disinfectant to be ready for other patient. After the bath the foot was dried by clean dry tissue. These sessions were repeated daily for 15 days.
Four parameters were evaluated pre and post the treatment, Blood flow to the foot by Doppler flowmeter (Greyline-PDFM 5.1), size of the ulcerative area, color and sensation of the foot.
The ulcer size was measured by metered ribbon, while the color was evaluated by the following scale: (1 = normal skin, 2 = pink with no necrotic areas, 3 = blue minor necrosis, 4 = yellow, medium necrosis and 5 = black, deep necrosis).
The sensation of the area was evaluated by pressure pin performed by a dermatologist and the scale was: (1 = normal sensation, 2 = fair, 3 = slight sensation, 4 = poor sensation, and 5 = no sensation)
3. Rustles and Discussion
The improved circulation induced by carboxy therapy is due to improved tissue oxygenation. The hypercarpnia results in increase oxygen exchange between blood hemoglobin and myoglobuline of the peripheral tissues. It also decreases resistance of the arteries in the skin and muscles which dilate on account of the decline in pH. Carbonic acid is rapidly dissociated to bicarbonate and H+ as shown in the following equations:
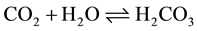
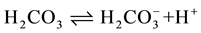
This differential pH change favors the unloading of oxygen in the tissues making hemoglobin more efficient transporter for oxygen [25] . It also permits the release of growth factor for angiogenesis [24] .
Some studies showed that vasodilation is mediated by nitric oxide which induces angiogenesis and suppresses vasoconstriction in response to cold by keeping the patients’ feet warm [26] .
Results shown in Table 1 and Figure 1 showed improvement in the blood flow expressed by mean Doppler pressure pre and post treatment significantly (p > 0.5). This improvement would be reflected on better oxygenation of the area which would improve angiogenesis and render the area unsuitable for anaerobic bacteria.
The improved circulation was also expressed by changing of the colour of the ulcerative area from yellow which represents medium necrosis to blue which represents minor necrosis.
This indicates an improvement in the healing of these ulcerative areas as shown in Figure 2.
The sensation of the patients ulcerative feet were also improved from poor sensation to some sensation upon evaluation after complete sessions Figure 3. This improvement is due to improved blood circulation an angiogenesis as well as to optimization of blood sugar that might be associated with CO2 therapy.
Results also showed that there was no significant change in the area of the ulceration (p < 0.5) after the specified time of therapy and this may be due to the fact that it needs more time than that of this study Figure 4.
Statistical analysis of the same parameters between males and females proved that there were no significant differences in the evaluated parameters in males and females and p < 0.5 for all parameters.
The overall outcome of these sessions resulted in obvious improvement in the condition of each patient’s ulcerative foot, but more time is needed to get the benefit of this result.
Figure 1. Mean blood flow rate pre and post CO2 treatment.
Figure 2. Mean colour changes pre and post CO2 treatment.
Figure 3. Mean sensation changes pre and post CO2 treatment.
Figure 4. Mean ulceration size in square centimeters pre and post CO2 treatment.
Table 1. Results of the measured parameters pre and post treatment as an average and standard deviation and standard error if the mean.
4. Conclusion
Carbone dioxide therapy is beneficial in improvement of diabetic foot ulceration and it has increased blood flow to the affected foot, improved the sensation, and decreased the necrosis. Further work is needed for longer time treatment to ensure better results in complete healing.
Cite this paper
NaeemShalan,AbdulrahmanAl-Bazzaz,IsraaAl-Ani,FadiNajem,MohammadAl-Masri, (2015) Effect of Carbon Dioxide Therapy on Diabetic Foot Ulcer. Journal of Diabetes Mellitus,05,284-289. doi: 10.4236/jdm.2015.54035
References
- 1. Kumar, P.J. and Clark, M. (2002) Textbook of Clinical Medicine. 8th Edition, Saunders, London.
- 2. American Diabetes Association (2009) Diagnosis and Classification of Diabetes Mellitus. Diabetes Care, 32, 62-67.
http://dx.doi.org/10.2337/dc09-S062 - 3. Beverley, B. and Eschwège, E. (2003) The Diagnosis and Classification of Diabetes and Impaired Glucose Tolerance. In: Pickup, J.C. and Williams, G., Eds., Textbook of Diabetes, 3rd Edition, Blackwell Publishing, UK, 2.1-2.11.
- 4. Lindberg, G., Lindblad, U. and Melander, A. (2004) Sulfonylureas for Treating Type 2 Diabetes Mellitus. Cochrane Database of Systematic Reviews, 3, 151-155.
- 5. Bearse, M.A., Han, T., Schneck, M.E., et al. (2004) Local Multifocal Oscillatory Potential Abnormalities in Diabetes and Early Diabetic Retinopathy. Investigative Ophthalmology & Visual Science, 45, 3259-3265.
http://dx.doi.org/10.1167/iovs.04-0308 - 6. Hove, M.N., Kristensen, J.K., Lauritzen, T. and Bek, T. (2004) The Prevalence of Retinopathy in an Unselected Population of Type 2 Diabetes Patients from Arhus County, Denmark. Acta Ophthalmologica Scandinavica, 82, 443-448.
http://dx.doi.org/10.1111/j.1600-0420.2004.00270.x - 7. Seki, M., Tanaka, T., Nawa, H., et al. (2004) Involvement of Brain-derived Neurotrophic Factor in Early Retinal Neuropathy of Streptozotocin-Induced Diabetes in Rats: Therapeutic Potential of Brain-Derived Neurotrophic Factors for Dopaminergic Amacrine Cells. Diabetes, 53, 2412-2419.
http://dx.doi.org/10.2337/diabetes.53.9.2412 - 8. Moran, A., Palmas, W., Field, L., et al. (2004) Cardiovascular Autonomic Neuropathy Is Associated with Microalbuminuria in Older Patients with Type 2 Diabetes. Diabetes Care, 27, 972-977.
http://dx.doi.org/10.2337/diacare.27.4.972 - 9. Huang, C., Kim, Y., Caramori, M.L., et al. (2002) Cellular Basis of Diabetic Nephropathy: II. The Transforming Growth Factor-Beta System and Diabetic Nephropathy Lesions in Type 1 diabetes. Diabetes, 51, 3577-3581.
http://dx.doi.org/10.2337/diabetes.51.12.3577 - 10. Shukla, N., Angelini, G.D., Jeremy, J.Y., et al. (2003) Homocysteine as a Risk Factor for Nephropathy and Retinopathy in Type II Diabetes. Diabetologia, 46, 766-772.
http://dx.doi.org/10.1007/s00125-003-1104-x - 11. Svensson, M., Eriksson, J.W. and Dahlquist, G. (2004) Early Glycemic Control, Age at Onset, and Development of Microvascular Complications in Childhood-Onset Type 1 Diabetes: A Population-Based Study in Northern Sweden. Diabetes Care, 27, 955-962.
http://dx.doi.org/10.2337/diacare.27.4.955 - 12. Saely, C.H., Aczel, S., Marte, T., et al. (2004) Cardiovascular Complications in Type 2 Diabetes Mellitus Depend on the Coronary Angiographic State Rather than on the Diabetes State. Diabetologia, 47, 145-146.
http://dx.doi.org/10.1007/s00125-003-1274-6 - 13. Wallace, C., Reiber, G.E., LeMaster, J., et al. (2002) Incidence of Falls, Risk Factors for Falls, and Fall-Related Factures in Individuals with Diabetes and a Prior Foot Ulcer. Diabetes Care, 25, 1983-1986.
http://dx.doi.org/10.2337/diacare.25.11.1983 - 14. Lipsky, B.A. (2004) A Report from the International Consensus on Diagnosing and Treating the Infected Diabetic Foot. Diabetes/Metabolism Research and Reviews, 20, 68-77.
http://dx.doi.org/10.1002/dmrr.453 - 15. Lipsky, B.A., Picoreto, R.E. and Wheat, L.J. (1990) The Diabetic Foot: Soft Tissue and Bone Infection. Infectious Disease Clinics of North America, 4, 409-432.
- 16. Gerding, D.N. (1995) Foot Infections in Diabetic Patients: The Role of Anaerobes. Clinical Infectious Diseases, 20, 83-88.
http://dx.doi.org/10.1093/clinids/20.Supplement_2.S283 - 17. Sapico, F.I., Witte, J.L., Canawati, H.N., Montogomerie, J.Z. and Bessman, A.N. (1984) The Infected Foot of the Diabetic Patient: Quantitative Microbiology and Analysis of Clinical Features. Reviews of Infectious Diseases, 6, 171-176.
http://dx.doi.org/10.1093/clinids/6.Supplement_1.S171 - 18. Caputo, G.M., Gavanagh, P.R., Ulbrech, J.S., Gibbones, G.W. and Karchmer, A.W. (1994) Assessment and Management of Foot Diseases in Patients with Diabetes. The New England Journal of Medicine, 331, 853-860.
http://dx.doi.org/10.1056/NEJM199409293311307 - 19. Joshi, N., Caputo, G., Weitekamp, M. and Karchmer, A. (1999) Infections in Patients with Diabetes Mellitus. The New England Journal of Medicine, 341, 1906-1912.
http://dx.doi.org/10.1056/NEJM199912163412507 - 20. Alavil, S.M., Khosravi, A.D., Sarami, A., Dashtebozorg, D. and Montazeri, E.A. (2007) Bacteriologic Study of Diabetic Foot Ulcers. Pakistan Journal of Medical Sciences, 23, 681-684.
- 21. Alnaeb, M.E., Crabtree, V.P., Boutin, A., Mikhailidis, D.P., Seifalian, A.M. and Hamilton, G. (2007) Prospective Assessment of Lower-Extremity Peripheral Arterial Disease in Diabetic Patients Using a Novel Automated Optical Device. Angiology, 58, 579-585.
http://dx.doi.org/10.1177/0003319707305685 - 22. Zenker, B. (2012) Carboxytherapy: Carbon Dioxide Injections in Aesthetic Medicine.
http://www.plastikoperationer.net/wp-content/uploads/2013/02/Carboxy-therapy-report.pdf - 23. Hayashi, M.S., Yamada, S., Kumada, Y., Matsuo, H., Toriyama, T. and Kawahara, H. (2008) Immersing Feet in Carbon Dioxide-Enriched Water Prevents Expansion and Formation of Ischemic Ulcers after Surgical Revascularization in Diabetic Patients with Critical Limb Ischemia. Annals of Vascular Diseases, 1, 111-117.
http://dx.doi.org/10.3400/avd.AVDoa08001 - 24. Pamela, C. and Richard, A. (2005) Lippincott’s Illustrated Review: Biochemistry. 3rd Edition, Lippincott Williams & Wilkins, New York.
- 25. Ziche, M., Morbidelli, L., Masini, E., Amerini, S., Granger, H.J., Maggi, C.A., Geppetti, P. and Ledda, F. (1994) Nitric oxide Mediates Angiogenesis in Vivo and Endothelial Cell Growth and Migration in Vitro Promoted by Substance P. Journal of Clinical Investigation, 94, 2036-2044.
http://dx.doi.org/10.1172/JCI117557 - 26. Penhavel, M.V., Nascimento, V.H., Duraes, E.F., Carneiro, F.P. and Sousa, J.B. (2013) Effects of Carbon Dioxide Therapy on the Healing of Acute Skin Wounds Induced on the Back of Rats. Acta Cirurgica Brasileira, 28, 334-339.
NOTES
*Corresponding author.







