Case Reports in Clinical Medicine
Vol.3 No.7(2014), Article
ID:48044,6
pages
DOI:10.4236/crcm.2014.37097
Parotid Lipoma: A Case Report
Massimo Mesolella, Filippo Ricciardiello, Flavia Oliva, Teresa Abate, Antonella Miriam Di Lullo, Anna Marino
ENT Department, University “Federico II”, Naples, Italy
Email: filipporicciardiello@virgilio.it
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 28 May 2014; revised 27 June 2014; accepted 17 July 2014
ABSTRACT
Lipoma is a common benign tumor affecting the soft tissues arising in every location where fat is normally present. About 15% of lipomas occur in head and neck region. The lipoma of parotid gland is a rare entity, comprising 0.6% - 4.4% of all parotid tumors. The etiology remains unclear. The case described a lipoma of the superficial lobe of the parotid gland in a 46-year-old male.
Keywords:Lipoma, Parotid Gland, Parotidectomy

1. Introduction
Lipoma is one of the most common benign tumors of mesenchymal origin, thinly encapsulated found anywhere on the body where fat is normally present [1] . In the head and neck, this tumor is not common [2] . Less than 15% (about 13% - 25%) of all lipomas occur in the head and neck [1] [3] , where they account for 0.1% - 5% of all benign tumors [2] [4] . In the head and neck, it arises mainly in the posterior cervical triangle and forehead. On rare occasions, however, it may occur in the pharynx, larynx, especially oral cavity, parotid gland and parapharyngeal space [1] [3] [5] -[7] . They can also be localized in the periparotid area and submandibular region [8] - [10] . They may be single or multiple [10] . The lipoma of parotid gland is a rare entity, comprising 0.6% - 4.4% of all parotid tumors in the literature, with most series reporting an incidence of 1% - 2% of all parotid tumors and 2.6% of benign tumors [1] [3] [10] . Lipoma is mostly a painless, asymptomatic and slow growing swelling [4] . Lipomas of parotid generally occur in sixth decade (ranging from 34 to 80 years) [10] . Those in deep lobe have been reported to be highest in fourth decade [4] [11] . Histologically, these tumors contain fat cells, although subtypes such as angiolipoma, angiomyolipoma, leiomyolipoma, osteolipoma and chondrolipoma containing other mesenchymal tissues can be present [12] . Recently, improved preoperative evaluation techniques, including the use of computed tomography (CT), magnetic resonance imaging (MRI), and fine-needle aspiration (FNA), have enabled a more accurate assessment of these tumors and a rational approach to their management [13] . Symptoms are few and uncharacteristic, hence preoperative diagnosis is difficult [2] .
Because of the relative rarity of lipomas in the parotid region, we present a case of parotid lipoma.
2. Case Report
A 46-year-old Italian male consulted our department complaining a painless swelling on the left side of the upper neck and face of 2 years duration. The swelling was progressively increasing in size since then. Physical examination revealed a mass of the left parotid region which was elastic, soft, mobile, regular, non-tender, nonfluctuant, non-pulsatile and non-transilluminant intraglandular mass.
The overlying skin was found to be normal. There was no other mass palpable in head and neck region. Function of facial nerve was intact. Rest of the otolaryngological examination was normal.
A high frequency ultrasonography visualized a nodular mass in left retro-angolo-mandibular region with high definition of margins and heterogeneity for presence of fibrous bundles that showed a striate echogenic tumour. The nodular mass was 28.4 × 20.6 × 20.2 mm with average of 23 mm (Figure 1). After one year the patient made onother ultrasonography that revealed a solid nodular mass with regular margins of 35 × 21 mm. Subsequently a TC with and without contrast showed a low density homogeneous capsulated mass with sharp margins in the superficial lobe of the left parotid gland of 21 × 34 mm (Figure 2). The contrast enhanced high resolution CT scan showed a homogenous lobulated low density mass (−100 Hounsfield units) in the superficial
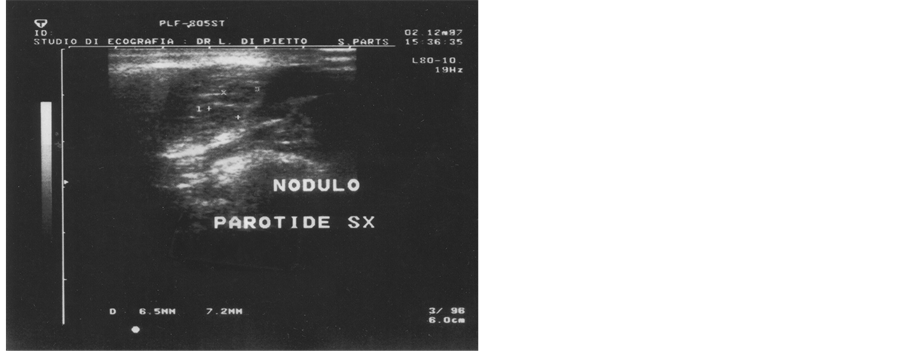
Figure 1. Ultrasound image visualized a nodular mass in left retro-angolo-mandibular region with high definition of margins and heterogeneity for presence of fibrous bundles that showed a striate echogenic tumour. The nodular mass was 28.4 × 20.6 × 20.2 mm with average of 23 mm.
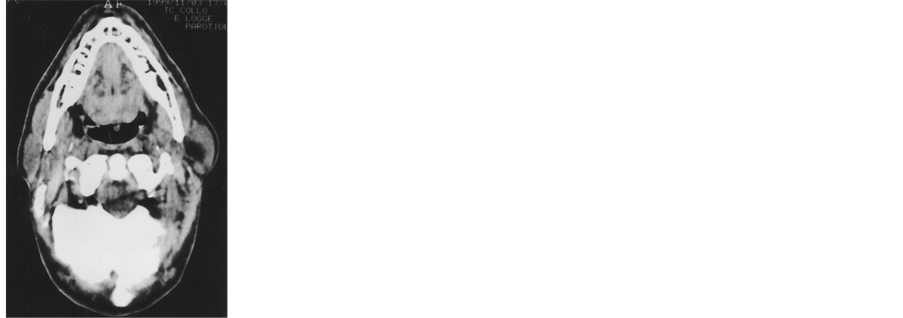
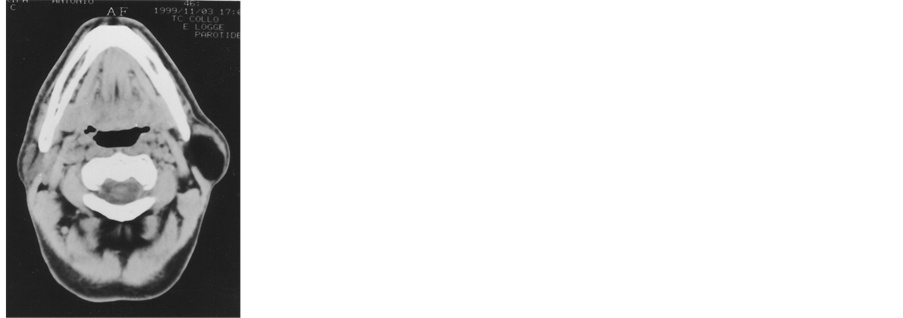
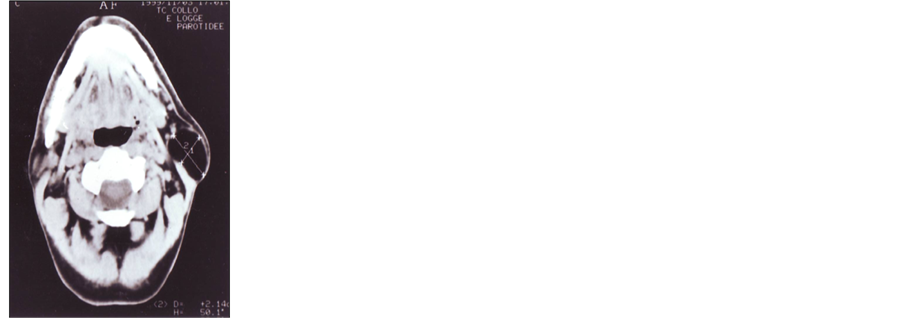
Figure 2. CT scans showed a low density homogeneous capsulated mass with sharp margins in the superficial lobe of the left parotid gland of 21 × 34 mm.
left parotid gland. The mass was the same density as fatty tissue.
MRI showed, on T1- and T2-weighted images, a well-defined bright lesion in the superficial lobe of the left parotid gland. A fine needle aspiration cytology (FNAC) was conclusive for the presence of “homogeneous proliferation of mature adipocytes”, compatible with lipoma. We performed tumor excision via a superficial parotidectomy with facial nerve preservation, under general anesthesia, using a classic Blair’s incision (Figure 3). Intraoperatively, a large mass was located in the left parotid space. The tumor comprised a well circumscribed, soft, yellow, fatty mass covered with a thin fibrous capsule (Figure 4). It was easily removed without injury of any major neurovascular structures. Histological diagnosis was lipoma characterized by sharply demarcated with thin fibrous connective tissue and comprised of homogeneous proliferation of mature adipocytes lobulated with a fine fibrous septa (Figure 5). The patient was discharged after 3 days. He has been followed-up for 12 months without recurrence of disease.


Figure 3. Surgical approach: superficial parotidectomy with facial nerve preservation, under general anesthesia, using a classic Blair’s incision.
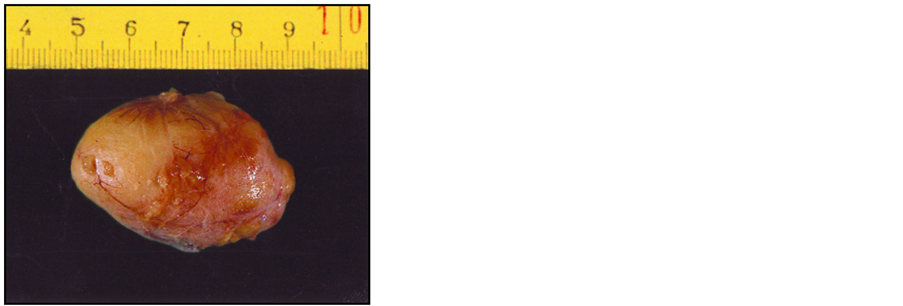
Figure 4. Specimen: the tumor comprised a large, well circumscribed, soft, yellow, fatty mass covered with a thin fibrous capsule.


Figure 5. Histological diagnosis was lipoma characterized by sharply demarcated with thin fibrous connective tissue and comprised of homogeneous proliferation of mature adipocytes lobulated with a fine fibrous septa.
3. Discussion
Lipoma of salivary glands is quite rare with the highest frequency reported in parotid gland that presents normally adipose tissue [4] [14] . In fact, lipomas histologically resemble normal mature adipose tissue, but the presence of a fibrous capsule helps to distinguish them from normal simple fat aggregation [1] [4] .
Lipomas are among the most common soft tissue tumors and approximately 15% of all lipomatous tumors arise in the head and neck, especially in the superficial and subcutaneous layers. Different causes of lipomas are mentioned in the literature: heredity, obesity, diabetes, radiation, endocrine disorders, insulin injection, corticosteroid therapy and trauma [3] . Trauma and lipoma are found to be most frequently correlated on clinical history. Trauma to soft tissue has been hypothesized to result in haematoma, with subsequent lymphatic effusion, fat necrosis and lipoma formation located in the subcutaneous plane [3] .
The highest reported incidence of lipoma in the parotid gland is 4.4%, with males most frequently affected with a sex ratio of 5:1 [3] [10] [15] . Moreover, the majority of patients had a single lesion without any predisposing factor. Usually intraparotid lipomas occur in the superficial lobe in 75% of cases, while in the deep lobe extending to the parapharyngeal space in 8.5% of cases and both in the deep and superficial lobe on the inferior part of the gland in 16.5% of cases [10] . They progress asymptomatially until reaching a large size. Clinically, the parotid lipoma appears as soft, slow growing, painless, well delineated asymptomatic mass [4] [16] . The clinical diagnosis is generally difficult, probably due to low index of clinical suspicion [4] .
Nowadays, the preoperative imaging has a crucial role to correctly diagnose the nature of lesions. Its main function is to eliminate extra-parotid subcutaneous lesions, and secondly to confirm the diagnosis of lipoma [10] . A correct clinical and instrumental evaluation of parotid gland masses, including both CT scan and MRI, can lead to a pre-operative diagnosis of lipoma. These two methods are a well-established imaging procedure and they can be helpful in giving information about pathological features of the tumors, to evaluate the location of the tumour and to programme the correct surgical approach [3] .
Ultrasound can give a clear and fast diagnosis of lipoma. It can be used as the initial study and shows a more o less homogeneous hypoechoic lesion that can be ovoid or lobulated [10] .
CT shows a hypodense and homogeneous mass with few septations and less than water density [3] . The normal parotid tissue reveals positive density, whereas lipomatous tissue will give negative attenuation (−50 to −150 Hounsfield units) [4] [17] . CT scan does not help much in differentiation of lipoma from surrounding adipose tissue. This information can be clearly gathered from MRI scan, which thus becomes the ideal radiological investigation for such tumors [4] . The normal parotid gland has a high fat content and is easily visualized on both CT and MRI, and therefore both techniques can demonstrate whether a mass in that region is intraglandular or extraglandular [1] [18] .
Hence MRI remains the best diagnostic technique that can accurately diagnose lipomas preoperatively by comparing the signal intensity on T1- and T2-weighted images [1] : in fact MRI presents the typical signal intensity patterns with high signal intensity on T1- and T2-weighted images without contrast media enhancement and with a weak signal on fat-suppressed images. MRI can also clearly define the limits of lipoma from normal adipose tissue (subcutaneous tissue) with a “black-rim” around the mass, a distinction that cannot be made from CT [1] [3] [10] . Moreover, MRI is sufficiently accurate to distinguish between lipomas and liposarcomas. The homogeneous nature of the lesion on MRI points towards lipoma, while in cases of liposarcoma the tumor is more heterogeneous and it is enhanced following injection of contrast medium [10] . In the literature, correct categorization of benign vs. malignant parotid gland tumour has been reported to be 87% after CT/MRI examination [19] , lipoma can be distinguished from well-differentiated liposarcoma by the presence of thick septa, the presence of nodular/globular or non-adipose mass-like areas [19] . Many Authors believe that a CT or MRI can correctly diagnose a lipoma preoperatively in all cases, thereby allowing better treatment planning [10] . Fine-needle aspiration biopsy (FNAB), commonly performed in the diagnostic work-up for parotid mass, does not provide sufficient data for diagnosis [3] [4] [14] .
During surgery, the facial nerve is identified and followed up to its peripheral branches, as far as necessary for tumour dissection and to evoid the neural block, created by increased intra-neural pressure so the nerve cannot conduct an impulse across the site of compression. If the compression is relieved, return of facial movement may begin immediately or within 3 weeks [3] . In every surgical resection, pre-operative planning is crucial. Nowadays surgical therapy rap presents the only treatment of choice for these tumors. There are different types of surgical approaches according to topography, size of tumor, pathology and its relationship to surrounding regions. The surgical procedure reported in English literature consisted of superficial parotidectomy, partial excision of the inferior part of the parotid gland, extrcapsular dissection, near total parotidectomy in the case with parapharyngeal extension [10] . In 83% of cases, surgery was performed for esthetic and/or functional discomfort caused by increased tumor volume. The average time between the discovery of lipoma and surgical excision is about 1 - 3 years in literature such as in our case. During operation most surgeons recommend superficial parotidectomy with dissection of the facial nerve before removal of lesions in the deep lobe [1] . Debnath, S.C., et al. exposed all the branches from the main trunk of the facial nerve by meticulous dissection and superficial parotidectomy [1] .
Lipomas that involve the deep parotid lobe are extremely rare, and their management is challenging; it should include meticulous dissection of the branches of the facial nerve. The postoperative aesthetic and functional results should be the major concerns [1] . In these cases, surgical management is total parotidectomy with the preservation of facial nerve. The lipoma resembles in appearance to the surrounding adipose and salivary tissue and it may be difficult to distinguish [4] . Therefore high incidence of facial nerve dysfunction has been reported after total conservative parotidectomy done for deep lobe parotid lipoma [5] .
Analysis of previous series reveals that around 50% of the reported cases have developed transient or permanent facial weakness postoperatively [4] . The meticulous dissection in the form of full exposure of nerve and use of facial nerve monitor helps in protecting facial nerve function.
4. Conclusion
Lipoma of the parotid gland is rare and can be clinically misleading about 30% of patients. Preoperative images, CT and MRI, have a crucial role because they locate the tumor on the parotid gland and facilitate the diagnosis of lipoma. The surgical excision can be delayed and finally surgical decision is made for esthetic and/or functional considerations in more than 80% of cases [10] . Usually there aren’t problems in terms of dissection and NIM can be used in cases of recurrence or large tumor surgery.
References
- Debnath, S.C. and Saikia, A. (2010) Lipoma of the Parotid Gland Extending from the Superficial to the Deep Lobe: A Rarity. British Journal of Oral and Maxillofacial Surgery, 48, 203-204. http://dx.doi.org/10.1016/j.bjoms.2009.07.028
- Khorsandi Ashtiani, M.T., Yazdani, N., Saeedi, M. and Amali, A. (2010) Large Lipoma of the Larynx: A Case Report. Acta Medica Iranica, 48, 353-356.
- Dispenza, F., De Stefano, A., Romano, G. and Mazzoni, A. (2008) Post-Traumatic Lipoma of the Parotid Gland: Case Report. Acta Otorhinolaryngologica Italic, 28, 87-88.
- Chakravarti, A., Dhawan, R., Shashidhar, T.B., Shakuntala and Sahni, J.K. (2008) Lipoma of the Deep Lobe of Parotid Gland—A Case Report and Review of Literature. Indian Journal of Otolaryngology and Head Neck Surgery, 60, 194-196.
- Kimura, Y., Ishikawa, N., Goutsu, K., Kitamura, K. and Kischimoto, S. (2002) Lipoma in the Deep Lobe of the Parotid Gland: A Case Report. Auris Nasus Larynx, 29, 391-393. http://dx.doi.org/10.1016/S0385-8146(02)00018-4
- RK, A., PN, N., S, Y., VK, A. and KK, D. (2013) Intraoral Lipoma: A Rare Case Report and Review of Literature. Journal of Clinical and Diagnostic Research, 7, 3090-3091.
- Nader, S., Nikakhlagh, S., Rahim, F. and Fatehizade, P. (2012) Endolaryngeal Lipoma: Case Report and Literature Review. Ear, Nose Throat Journal, 91, E18-E21.
- Janecka, I.P., Conley, J., Perzin, K.H. and Pitman, G. (1977) Lipomas Presenting as Parotid Tumors. Laryngoscope, 87, 1007-1010. http://dx.doi.org/10.1288/00005537-197706000-00018
- Furlong, M.A., Fanburg-Smith, J.C. and Childers, E.L. (2004) Lipoma of the Oral and Maxillofacial Region: Site and Subclassification of 125 Cases. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 98, 441-450. http://dx.doi.org/10.1016/j.tripleo.2004.02.071
- Fakhry, N., Justin, M., Varoquaux, A., Antonini, F., Santini, L., Lagier, A., Turner, F., Patrick, D. and Giovanni, A. (2012) Is Surgical Excision of Lipomas Arising from the Parotid Gland Systematically Required? European Archives of Oto-Rhino-Laryngology, 269, 1839-1844. http://dx.doi.org/10.1007/s00405-011-1843-0
- Ulku, C.H., Uyar, Y. and Unald, D. (2005) Management of Lipomas Arising from Deep Lobe of the Parotif Gland. Auris Nasus Larynx, 32, 49-53.
- Ohno, Y., Muraoka, M., et al. (1998) Osteolipoma of the Parapharyngeal Space. European Archives of Oto-Rhino-Laryngology, 255, 315-317. http://dx.doi.org/10.1007/s004050050067
- Ulku, C.U. and Uyar, Y. (2004) Parapharyngeal Lipoma Extending to Skull Base: A Case Report and Review of the Literature. Skull Base, 14, 121-125. http://dx.doi.org/10.1055/s-2004-828708
- Layfield, L.J., Glasgow, B.J. and Lufkin, R. (1991) Lipomatous Lesions of the Parotid Gland: Potential Pitfalls in Fine Needle Aspiration Biopsy Diagnosis. Acta Cytologica, 35, 553-556.
- El Monem, M.H., Gaafar, A.H. and Magdy, E.A. (2006) Lipomas of the Head and Neck: Presentation Variability and Diagnostic Workup. The Journal of Laryngology Otology, 120, 47-55. http://dx.doi.org/10.1017/S0022215105004597
- Srinivasan, V., Ganesan, S. and Premachandra, J. (1996) Lipoma of the Parotid Gland Presenting with Facial Palsy. The Journal of Laryngology Otology, 110, 93-95.http://dx.doi.org/10.1017/S0022215100132827
- Korentager, R., Noyek, A.M., Chapnik, J.S., et al. (1988) Lipoma and Liposarcoma of the Parotid Gland: High Resolution Preoperative Imaging Diagnosis. Laringoscope, 98, 967-971.http://dx.doi.org/10.1288/00005537-198809000-00011
- Cummings, C.W. (2005) Cummings Otolaryngology: Head & Neck Surgery. Vol. 2, Chapter 60: Benign Neoplasms of the Salivary Glands. 4th Edition, Elsevier Mosby.
- Kransdorf, M.J., Bancroft, L.W., Peterson, J.J., Murphey, M.D., Foster, W.C. and Temple, H.T. (2002) Imaging of Fatty Tumor: Distinction of Lipoma and Well-Differentiated Liposarcoma. Radiology, 224, 99-104.http://dx.doi.org/10.1148/radiol.2241011113

