Open Journal of Obstetrics and Gynecology
Vol.3 No.9(2013), Article ID:40078,4 pages DOI:10.4236/ojog.2013.39127
Placenta previa and percreta with massive genital bleeding in the first trimester of pregnancy: A case report*
![]()
1Department of Obstetrics and Gynecology, Niigata University General Hospital of Medical and Dental Sciences, Niigata, Japan
2Department of Radiology, Niigata University General Hospital of Medical and Dental Sciences, Niigata, Japan
3General Center for Perinatal, Maternal and Neonatal Medicine, Niigata University General Hospital of Medical and Dental Sciences, Niigata, Japan
Email: #obgy@med.niigata-u.ac.jp
Copyright © 2013 Masayuki Yamaguchi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 30 October 2013; revised 19 November 2013; accepted 25 November 2013
Keywords: Placenta Percreta; Massive Bleeding in Early Pregnancy; Internal Iliac Artery Catheter Ballooning; Cesarean Hysterectomy
ABSTRACT
A 40-year-old woman with a history of cesarean section and 3 episodes of uterine curettage for spontaneous or induced abortion presented with massive genital hemorrhage in the ninth week of gestation; she was treated with red cell concentrate and fresh frozen plasma transfusion. She was admitted to our hospital at the 11th week of gestation for continuous genital hemorrhage and cervical shortening (20 mm). Ultrasonography revealed placenta previa totalis. A lowlying gestational sac in early pregnancy, vascular lacunae, and an obscured retroplacental sonolucent zone indicated placenta percreta; magnetic resonance imaging showed similar findings. Owing to placenta percreta, uterus preservation was considered impossible. Elective cesarean section followed by total hysterectomy was performed at the 37th week of gestation, with bilateral internal iliac artery balloon catheter occlusion for reducing blood loss. The perioperative blood loss was 2,835 mL, for which the patient received blood transfusion. The postoperative course was uncomplicated.
1. INTRODUCTION
The treatment of placenta percreta is one of the most difficult procedures in perinatal medicine because of the risk of intraoperative massive hemorrhage. Abnormal placental adherence occurs after defective decidual formation. In rare cases, the placenta remains unusually adherent to the implantation site, with scanty or absent deciduas, due to the fact that the physiological line of cleavage through the decidual spongy layer is lacking.
Here, we report our experience of cesarean hysterectomy using bilateral internal iliac artery balloon catheter occlusion in a patient with placenta previa percreta, avoiding catastrophic hemorrhage and leading to good clinical outcome.
2. CASE REPORT
A 40-year-old woman, gravid 4, para 1, was referred to Niigata University General Hospital of Medical and Dental Science for advanced prenatal care after massive genital bleeding in the ninth week of gestation. At 35 years of age, she had undergone cesarean section at the 37th week of gestation due to breech presentation; further, the patient underwent uterine curettage thrice due to spontaneous or artificial abortions.
For the present pregnancy, the patient was impregnated by frozen embryo transfer at an infertility and obstetrics clinic. Ultrasonographic examination showed a low-lying gestational sac at the fifth week of gestation, with slight genital bleeding. At the ninth week of gestation, abrupt, massive genital bleeding occurred. Transfusions of 6 units of red cell concentrate and fresh frozen plasma each were needed because of deterioration in the patient’s general condition. Subsequently, the genital bleeding gradually decreased, and her general condition improved.
The patient was referred to our hospital in the 11th week of gestation and was hospitalized. Pelvic examination revealed slight bloody discharge, and ultrasonographic examination demonstrated a heterogeneous appearance of the chorionic plate located at the internal cervical os, considered as intraplacental lacunae (Figure 1), along with cervical shortening (~20 mm).
Bed rest was advised to the patient, and her general condition continued to be normal. Repeated ultrasonographic examinations revealed normal fetal growth; however, the early findings indicating placenta previa were confirmed. Magnetic resonance imaging (MRI) performed at the 29th week of gestation revealed a bilobed appearance of the placenta invading the myometrium around the internal cervical os, with extreme thinning of the anterior uterine wall, suggestive of placenta increta or placenta percreta. Cystoscopy performed at the 30th week of gestation ruled out placental invasion into the mucosa of the urinary bladder.
Elective cesarean section and total hysterectomy with a multidisciplinary approach was planned for the 37th week of gestation. For reducing the perioperative blood loss and complications, we planned to use a temporary occlusive balloon in the internal iliac artery during the cesarean hysterectomy. Informed consent was obtained from the patient and her family after explaining the surgical and procedural risks involved. Preoperatively, both femoral arteries were punctured using the standard Seldinger technique, with placement of 5-Fr sheath introducers (Terumo Corporation, Tokyo, Japan). Using a 0.035- inch angled guidewire, a 4-Fr pigtail-shaped catheter (Terumo Clinical Supply, Gifu, Japan) was used to cannulate the contralateral internal iliac artery. This was exchanged for a 5.2-Fr occlusion balloon catheter (maximal occlusive diameter, 9 mm; Terumo Clinical Supply, Figure 2). The fluoroscopy time and dosimetry of fetal exposure were 9.3 min and 52 mGy, respectively. Subsequently, bilateral ureteral stent catheters were inserted by urologists under general anesthesia in the operation room.
Through a vertical abdominal incision, we observed that almost the entire anterior portion of the placenta bulged through the myometrium and uterine serosa, which was covered by obvious, tortuous cobweb-like vessels (Figure 3). Through a vertical incision at the uterine fundus, a male infant weighing 2,590 g was delivered. The Apgar scores of the infant were 2 and 3 at 1 and 5 min, respectively, due to the general anesthesia administered to the patient. The placenta and cord were left in utero, and the hysterotomy was rapidly closed with continuous sutures. At the beginning of the total hysterectomy, the bilateral round ligaments and ovarian proper ligaments were ligated and transected. Blunt dissection of the parametrial tissues and an incision on the peritoneum for vesicouterine excavation revealed neovasculature due to placenta percreta. As bleeding from the surface of the exposed placenta increased, the internal iliac artery balloon catheters were inflated, with an immediate reduction in blood loss that enabled the re-

Figure 1. Ultrasonogram at the 11th week of gestation, showing intraplacental lacunae (arrowheads).
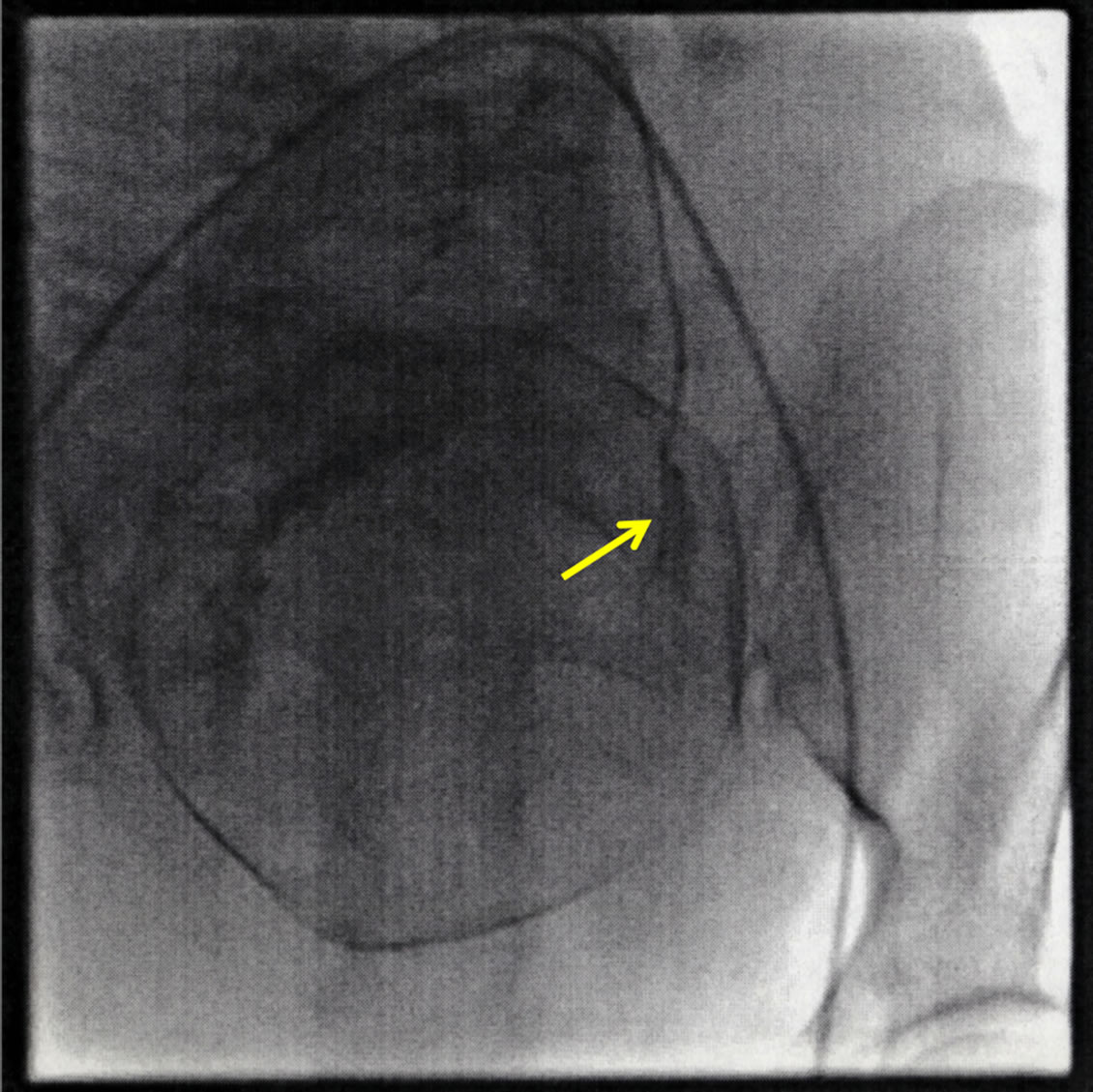
Figure 2. Fluoroscopic findings, confirming the placement of the occlusion balloon catheters in both internal iliac arteries (arrow: contrast material injected into the left internal iliac artery).
maining procedure to be performed in a relatively bloodless field. The bladder was carefully mobilized beneath the uterus and found to be intact. Total hysterectomy was performed, and the internal iliac artery balloon catheters were deflated before closure of the abdominal peritoneum to ensure adequate hemostasis. However, after this deflation, considerable oozing occurred on the surface of the urinary bladder and the parametrial region, requiring intensive hemostasis by fine ligation of blood vessels and fixation of fibrin sealants. Perioperatively, occlusion of the balloon catheters was sustained for 60 min, with the
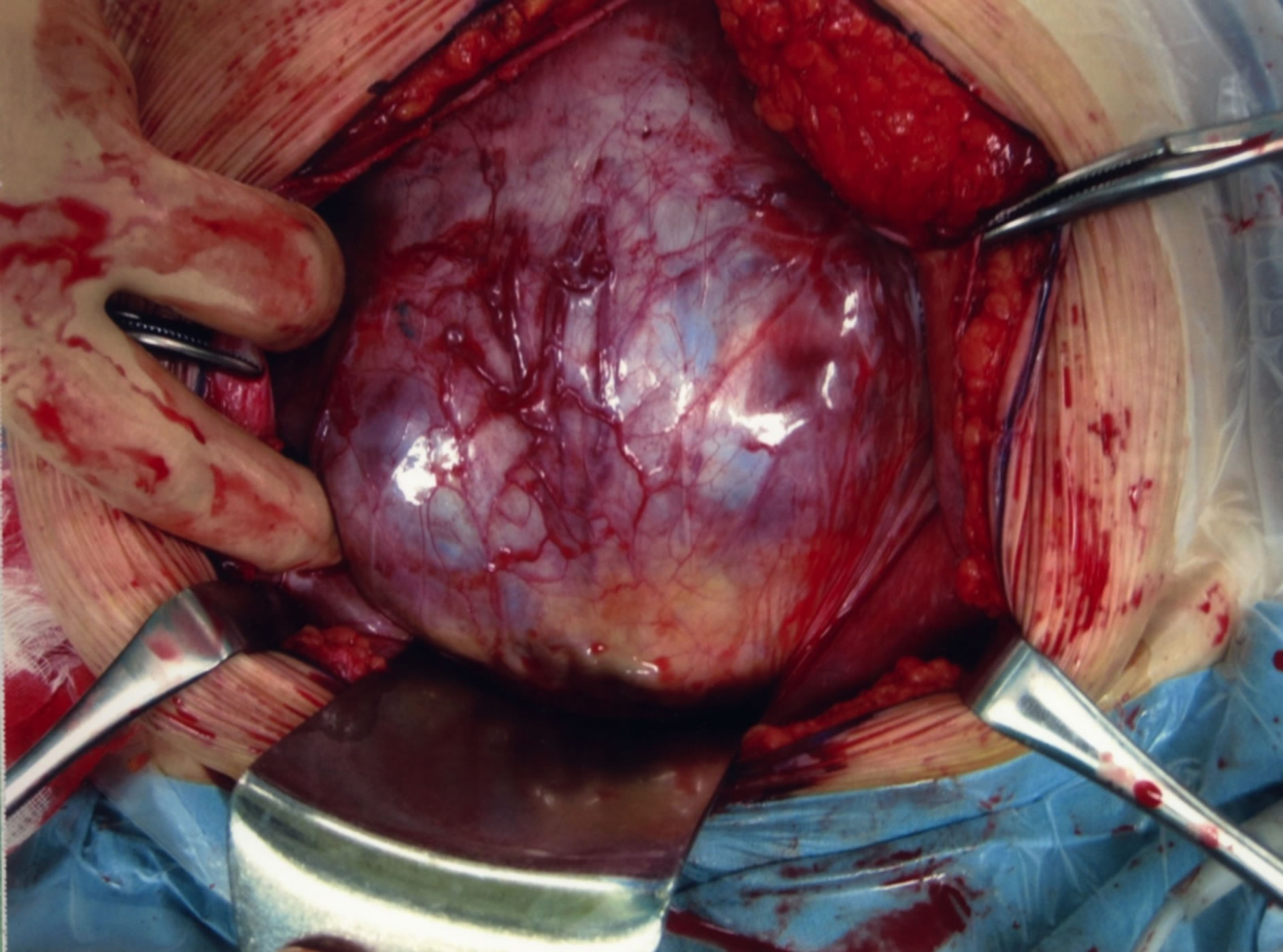
Figure 3. Intraoperative view showing the uterine serosa on the anterior side covered by obvious, tortuous cobweb-like vessels, indicating the presence of placenta previa percreta.
estimated total blood loss being 2,800 mL including amniotic fluid. The patient was transfused with 1,200 mL autologous total blood as well as 2 units of red cell concentrate and 6 units of fresh frozen plasma.
The patient tolerated the operation well, followed by a relatively uneventful postoperative course. The infant was hospitalized in the neonatal intensive care unit, and intubation with respiratory support was performed owing to the low Apgar scores. The respiratory support was stopped on day 2 after birth, and the infant discharged from the NICU along with the mother with no complications. Histological examination of the resected uterus showed that the chorionic villi had penetrated the entire myometrium without intervening deciduas, confirming the diagnosis of placenta percreta. At 1 month postoperatively, the mother and infant remained in good condition.
3. DISCUSSION
Placenta accreta occurs due to abnormal placental implantation. In most instances, the placenta separates spontaneously from its implantation site during the first few minutes after delivery of the infant. In rare cases, the placenta remains unusually adherent to the implantation site, with scanty or absent deciduas and an absent physiological line of cleavage through the decidual spongy layer [1]. Placenta accreta, increta, and percreta represent an important cause of peripartum hemorrhage and maternal morbidity in modern obstetrics, accounting for approximately 50% of emergency hysterectomies [2].
Etiological factors for placenta accreta, increta, and percreta include the occurrence of placenta previa, previous delivery by cesarean section, previous curettage(s), and multigravidity [3]. All of these factors were positive in this patient, with multigravida status, previous delivery by cesarean section, 3 instances of uterine curettage, and placenta previa in the present pregnancy. Moreover, the prenatal clinical course of the patient indicated the mechanism of occurrence of placenta percreta, i.e., the chorionic plate invaded the wound of the previous cesarean section, with the embryo being implanted in the lower uterine cavity around the isthmus uteri, which was noted on ultrasonography in early pregnancy. The invading chorionic plate possibly damaged the previous wound, leading to massive bleeding at the ninth week of gestation. Moreover, the macroscopic appearance of the resected uterus demonstrated placental invasion in the lower segment of the anterior uterine wall (around the previous incision for cesarean section), completely replacing the myometrium in the lower segment.
For the successful management of placenta percreta, additional hemostatic techniques are usually necessary during cesarean hysterectomy, such as bilateral internal iliac artery ligation, preoperative embolization of the internal iliac artery, and preoperative placement of occlusive balloon catheters in the internal iliac artery. However, the failure rate of iliac artery ligation is reportedly as high as 60% [4], with its efficacy being limited by the rapid recruitment of an extensive collateral system in the pelvis [5]. With arterial embolization, complications such as pelvic pain, sexual dysfunction, or urological involvement have been reported [4,6].
At present, preoperative arterial balloon catheter occlusion is considered to be a promising technique. Although aortic balloon occlusion is an easier procedure than internal iliac artery balloon occlusion, the former is associated with potential risks such as aortic rupture, plaque dislodgement and embolization to a distal vessel, inability to deflate the balloon, and inability to withdraw the balloon through the sheath [4]. Further, common iliac arterial balloon occlusion is associated with reperfusion injury, thrombosis, and/or embolism of the lower extremities [7]. Despite the existence of anastomoses between the external iliac artery and arteries perfusing the uterus, the effectiveness of internal iliac artery balloon catheter occlusion in reducing blood loss has been demonstrated previously [8,9]. Keeping in mind these considerations, bilateral internal iliac artery balloon occlusion was adopted in this case, and a marked reduction in blood loss was noted immediately after the inflation of the balloon catheter.
4. CONCLUSION
Although predicting the occurrence of placenta percreta is not easy, a low-lying gestational sac and massive bleeding in early pregnancy, especially in cases with previous cesarean section and/or multiple instances of uterine curettage, are considered as alarm signals for placenta percreta. Further evaluation and comparisons are essential for validating the efficacy of the various types of arterial balloon catheter occlusion in cesarean hysterectomy for placenta percreta.
REFERENCES
- Cunningham, F.G., Leveno, K. J., Bloom, S.L., et al. (2010) William’s obstetrics. 23rd Edition, McGraw-Hill Medical, New York, 776-780.
- Daskalakis, G., Anastasakis, E., Papantoniou, N., Mesogitis, S., Theodora, M. and Antsaklis, A. (2007) Emergency obstetric hysterectomy, Acta Obstetricia et Gynecologica Scandinavica, 86, 223-227.
- Gielchinsky, Y., Rojansky, N., Fasouliotis and S.J. and Ezra, Y. (2001) Placenta accreta—Summary of 10 years: A survey of 310 cases. Placenta, 23, 210-214. http://dx.doi.org/10.1053/plac.2001.0764
- Masamoto, H., Uehara, H., Gibo, M., Okubo, E., Sakumoto K. and Aoki, Y. (2009) Elective use of aortic balloon occlusion in cesarean hysterectomy for placenta previa percreta. Gynecologic and Obstetric Investigation, 67, 92-95. http://dx.doi.org/10.1159/000164685
- Chait, A., Moltz, A. and Nelson Jr., J.H. (1968) The collateral arterial circulation in the pelvis. An angiographic study. The American Journal of Roentgenology, Radium Therapy and Nuclear Medicine, 102, 392-400. http://dx.doi.org/10.2214/ajr.102.2.392
- Diop, A.N., Bros, S., Chabrot, P., Gallot D. and Boyer, L. (2009) Placenta percreta: Urologic complication after successful conservative management by uterine arterial embolization: A case report. American Journal of Obstetrics & Gynecology, 201, e7-8. http://dx.doi.org/10.1016/j.ajog.2009.08.040
- Shin, J.C., Liu, K.L. and Shyu, M.K. (2005) Temporary balloon occlusion of the common iliac artery: New approach to bleeding control during cesarean hysterectomy for placenta percreta. American Journal of Obstetrics & Gynecology, 193, 1756-1758. http://dx.doi.org/10.1016/j.ajog.2005.08.033
- Tan, C.H., Tay, K.H., Sheah, K., Kwek, K., Wong, K., Tan, H. K. and Tan, B.S. (2007) Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accrete. American Journal of Roentgenology, 189, 1158-1163. http://dx.doi.org/10.2214/AJR.07.2417
- Carnevale, F. C., Kondo, M. M., de Oliveira Sousa, W. Jr., et al. (2011) Perioperative temporary occlusion of the internal iliac arteries as prophylaxis in cesarean section at risk of hemorrhage in placenta accrete. Cardio Vascular and Interventional Radiology, 34, 758-764. http://dx.doi.org/10.1007/s00270-011-0166-2
NOTES
*Disclosure: The authors have no conflicts of interest.
#Corresponding author.

