Paper Menu >>
Journal Menu >>
 Vol.1, No.2, 313-319 (2009) doi:10.4236/health.2009.14051 SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/ Health Which stressors are responsible for the worsening in the clinical symptomatology of lupus? M. I. Peralta-Ramírez1, J. Jiménez-Alonso2, M. Pérez-García1 1Department of Clinical Psychology, School of Psychology, University of Granada, Spain 2Systemic Autoimmune Disease Unit, University Hospital “Virgen de las Nieves”, Granada, Spain; mperalta@ugr.es Received 26 October 2009; revised 9 November 2009; accepted 12 November 2009. ABSTRACT Objective: The purpose of this study was to test which stressors worsen the symptoms perceived by patients with lupus, thus broadening and corroborating results obtained in a previous study published in Psychosomatic Medicine. Methods: In order to examine this question, we selected 43 patients with lupus whose symp- toms worsened due to the effects of daily stress. These patients were divided into two groups: patients whose increase in clinical lupus symp- tomatology was predicted by an increase in daily stressors on the same day (G1) and pa- tients whose increase in clinical lupus symp- tomatology was predicted by an increase in daily stressors the day before and the same day (G2). Later, three factorial analyses were con- ducted with the items related to stressors and the items related to lupic symptoms. Results: The results showed that in G1 there were three factors that made up a total of 35.08% of the explained variance. The stressors associated with certain symptoms of the illness in this group are feeling ill or being worried about their physical appearance, with the main stressor being the illness itself. However, in G2, two factors were found that made up a total of 40.37% of the explained variance for lag=0 and 38.67% for lag=1. The stressors associated with the majority of the lupus symptoms are of an interpersonal and work-related nature. This as- sociation was maintained when we carried out the factorial analyses with the items of the symptoms from the following day. Conclusions: The interpersonal and work-related stressors are related to a worsening in the majority of the lupic symptoms in the patients whose sympto- matology worsens as a result of daily stress experienced the day before. Keywords: Daily Stress; Interpersonal Stressor; Work-Related Stressors; Systemic Lupus Erythe- matosus 1. INTRODUCTION Various studies have shown the devastating effect psy- chological stress has on certain rheumatic diseases [1]. Specifically, diverse studies have shown that stress is one of the environmental factors that can cause a wors- ening in lupus [2-8]. Although the role of stress in this illness appears clear, at first, there was certain contro- versy about the nature of the stressors, as some authors supported the theory that daily stress (not organizing time well, problems in social relationships...etc.) was mainly responsible for the worsening in lupus [2-4,6-8], while other authors defended a greater effect of the Ex- traordinary Stressful Life Events (death of a family member, car accident, etc.) on the lupus [5]. Although there is currently a lot of evidence that daily stress is primarily responsible for the worsening of this illness, few studies have shown which specific stressors are most related to this worsening. Specifically, three main studies were carried out with this objective. The first was conducted by Schubert et al. [4]. The authors studied a woman suffering from SLE during a 63-day period. In this patient, the concentration of neopterin (immunological parameter closely related to lupic activity in patients with SLE) in urine was measured daily, and her daily stressors were evaluated weekly. The findings showed that the moderately stressful incidents that led to a high level of emotional irritation and had stressful interper- sonal implications increased the concentration of neop- terin approximately one day later, that is, with a lag=1. Therefore, these stressors play a greater role in the in- crease in neopterin than other stressors. One problem of this study is that the sample studied is very small (only one SLE patient was evaluated), so that it is impossible to draw generalizable conclusions. Later, these authors performed a new study [6] where they evaluated daily (every 12 hours) the levels of stress, cortisol and neop- terin in another lupus patient during a 56-day period.  M. I. Peralta-Ramírez et al. / HEALTH 1 (2009) 313-319 SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/ 314 They found that when the patient anticipated a moderate stressor (which in this case was the infidelity of her partner), her cortisol increased 24 hours before the inci- dent and lessened 12 hours after it had occurred. How- ever, if the patient did not anticipate the incident, her cortisol increased 24 hours after the incident and de- creased 36 hours after it. With regard to the neopterin, these authors found that after exposure to the stressor there was a reduction in the amount of neopterin in the following 36 hours, producing a new increase in the next 60 hours. In this way, the authors again showed the modulation of the immune system due to stressful events involving interpersonal relationships, and due to the an- ticipation of these stressors, in the following 24-36 hours. The latest study carried out with the objective of defin- ing the type of stressor that can affect the worsening of lupus is the one by Pawlak et al. [7]. These authors studied the stressors in 41 women with lupus during a six-month period and their physiological correlates (complement activity, anti-dsDNA and ECLAM-European Consensus Lupus Activity Measurement). The results showed that the patients who had a larger number of social obligations presented more outbreaks (92%) than the patients who had fewer social obligations (39%). Furthermore, these authors found an increase in the in- terpersonal relationship conflicts in the month prior to the lupic outbreak in the patients who experienced a wors- ening in the disease. As we can see, all of these studies seem to clearly agree that the stressors most related to the worsening of the disease are not only of a daily nature, but they also have a clear component related to interpersonal relation- ships. However, in addition to the different stressors common to the general population, there have been no studies on the effects that the perception itself of the worsening of the disease (another stressor) has on this worsening. Likewise, no studies been carried out to test whether experiencing different stressors acts on some target organ of the disease, thus produces its worsening (joints, skin, etc.), or whether, on the contrary, it acts on a general level by activating all the systems. Therefore, the purposes of the present study were, on one hand, to test what types of stressors are responsible for the worsening in the clinical symptomatology of lupus and, on the other, to find out what physical symptoms are involved in this worsening. These were tested in a group of patients that had already been evaluated and classified according to the effect that the stress had on their perception of the worsening of the disease [8]. 2. PATIENTS AND METHODS 2.1. Study Population 64 patients originally participated in this study, of which 6 were later rejected because they had mixed connective tissue disease rather than lupus. Therefore, 58 lupus pa- tients participated in the study, of which 50 were women and 8 men. 45 met at least 4 American College of Rheu- matology (ACR) [9] criteria for classification as suffer- ing from Systemic Lupus Erythematosus (SLE), and 12 were suffering from Chronic Lupus Discoid (CLD), di- agnosed by their clinical history and an anatomopa- thological study. The mean age was 39.37 years (SD=9.72), and the mean educational level was 10.7 years (SD=3.44), which is equivalent to a bachelor’s degree. The mean duration of the illness was 9.1 years (SD=6.38), the mean index of organ damage was 0.9 (SD=1.06), and the mean on the index of lupus activity was 1.73 (SD=3.2). All of the participants were patients at the Systemic Autoimmune Disease Unit at the University Hospital “Virgen de las Nieves” in Granada, Spain. They all had at least a minimum cultural background (they could at least read and write), and none of them presented any associated mental illness at the time of the study, al- though there were two patients with psychiatric histories. All of these patients gave their signed informed consent to participate in this study. Of these 58 patients, we only included the 43 patients for whom stress predicted a worsening in the clinical symptomatology of lupus. These subjects were classified into two groups: G1 with 31 pa- tients whose increase in the clinical symptomatology of the lupus was predicted by an increase in daily stressors on the same day; and G2 with 12 patients whose increase in the clinical symptomatology was predicted by an in- crease in daily stressors the day before and the same day. 2.2. Information Collected 2.2.1. Daily Stress Inventory (DSI) The translation and adaptation to the Spanish population of the Brantley, Waggoner and Jones Daily Stress Inven- tory (DSI) was carried out by Peralta-Ramírez [10]. For this adaptation, they used the responses to a complete version of the DSI given by a broad sample. They then created a 20 item version comprised of some items that remain identical (e.g., “I forgot something”), others that are worded in a different way (e.g., “gave up an undesir- able habit: eating too much, smoking, etc” for “gave up a habit that was not good for him”), and others that grouped various items from the DSI with related criteria (“Had problems in his relationship with other people: was criti- cized, ignored, interrupted when speaking…”). This in- strument measures stressful daily events and the degree of stress produced by each of them in the last 24 hours. It contains 20 items that are categorized from 0 to 6, de- pending on the degree of stress they have caused, keeping in mind that 0 is no stress experienced and 6 means the event caused panic. The instrument’s reliability coefficient is 0.82, the Cronbach alpha coefficient is 0.88, and its discriminated validity is 74.86% correct classification. Therefore, the instrument presents high validity for detecting change [10]. The items related to this instrument are included in Table 1.  M. I. Peralta-Ramírez et al. / HEALTH 1 (2009) 313-319 SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/ 315 Table 1. Items from the DSI and the SLI. ITEMS FROM THE DSI I1. Had problems at work, with a specific activity I2. Did not organize his or her time well I3. Had problems in his or her relationships with other people (was criticized, ignored, and interrupted when speaking...) I4. Has not slept soundly I5. Forgot something I6. Felt or feared being ill I7. Had some small accident I8. Thought about the future I9 Played a sport or game poorly I10. Did something he or she did not want to do I11. Lost something or couldn’t find something he or she was looking for I12. Bad weather affected him or her I13. Challenged someone in authority I14. Heard bad news I15. Something related to his or her personal appearance affected him or her I16. Was faced with a feared situation or object I17. Worried about other people’s problems I18. Barely escaped something dangerous I19. Gave up a habit that was not good for him or her I20. Had economic problems ITEMS FROM THE SLI S1. Loss of appetite S2. Joint pain S3. General malaise S4. Fatigue S5. Skin rash S6. Abdominal symptoms S7. Difficulty breathing 2.2.2. SLE Symptoms Inventory (LSI) This inventory was elaborated by the group of medical specialists in the Systemic Autoimmune Disease Unit of the Internal Medicine Service at the University Hospital “Virgen de las Nieves” in Granada [11]. It refers to 8 symptoms suggestive of SLE activity, namely loss of appe- tite, joint pain, general malaise, fever, tiredness or fatigue, skin rash, difficulty breathing and abdominal symptoms. These items are categorized from 1 to 10 according to the degree of intensity of these symptoms on that day. This inventory was designed to evaluate the subjective symp- toms of large groups of SLE patients in clinical studies. We tested its internal consistency, as well as its concor- dance with physician reports and serological indicators 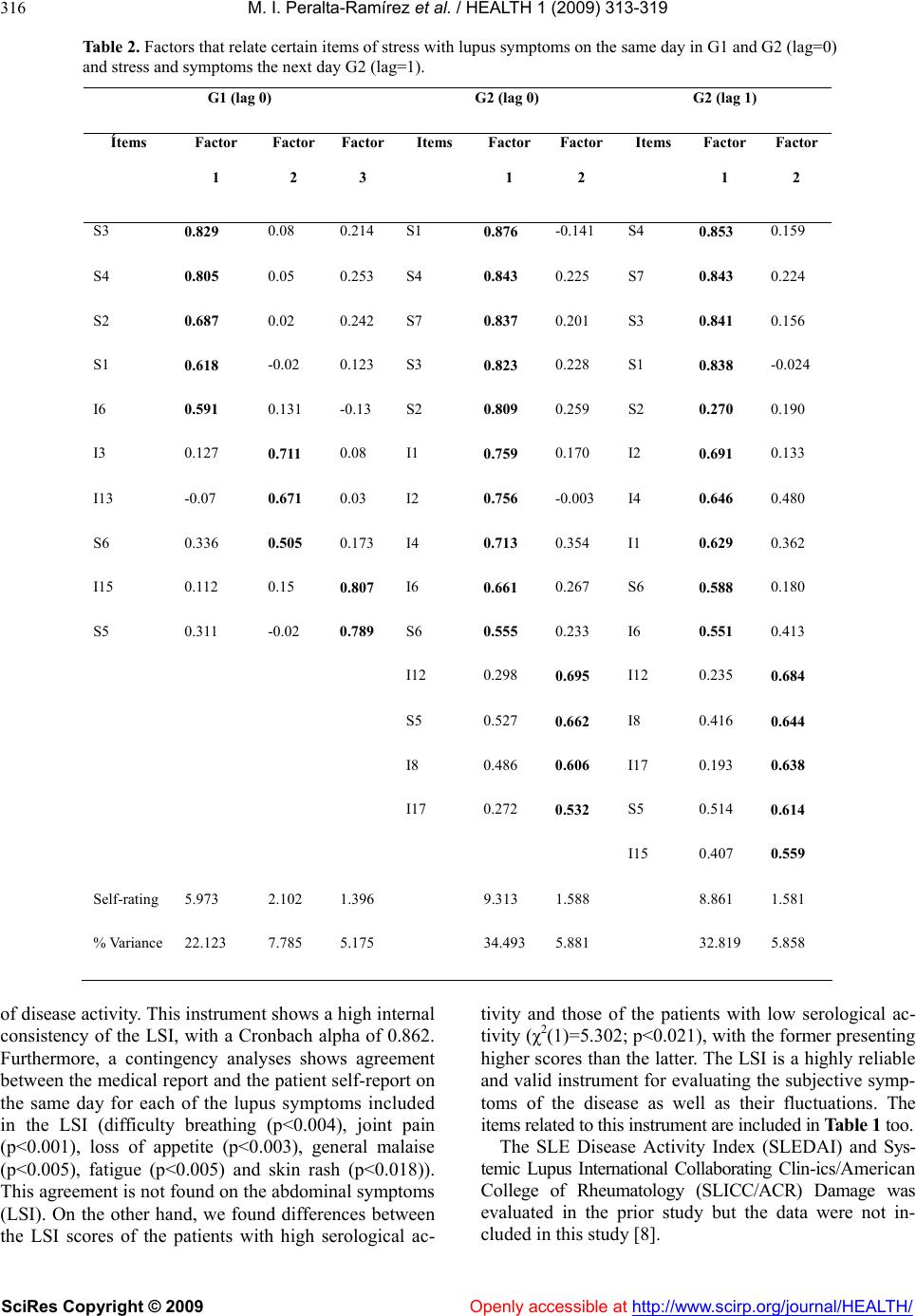 M. I. Peralta-Ramírez et al. / HEALTH 1 (2009) 313-319 SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/ 316 Table 2. Factors that relate certain items of stress with lupus symptoms on the same day in G1 and G2 (lag=0) and stress and symptoms the next day G2 (lag=1). G1 (lag 0) G2 (lag 0) G2 (lag 1) Ítems Factor 1 Factor 2 Factor 3 Items Factor 1 Factor 2 Items Factor 1 Factor 2 S3 0.829 0.08 0.214 S1 0.876 -0.141 S4 0.853 0.159 S4 0.805 0.05 0.253 S4 0.843 0.225 S7 0.843 0.224 S2 0.687 0.02 0.242 S7 0.837 0.201 S3 0.841 0.156 S1 0.618 -0.02 0.123 S3 0.823 0.228 S1 0.838 -0.024 I6 0.591 0.131 -0.13 S2 0.809 0.259 S2 0.270 0.190 I3 0.127 0.711 0.08 I1 0.759 0.170 I2 0.691 0.133 I13 -0.07 0.671 0.03 I2 0.756 -0.003 I4 0.646 0.480 S6 0.336 0.505 0.173 I4 0.713 0.354 I1 0.629 0.362 I15 0.112 0.15 0.807 I6 0.661 0.267 S6 0.588 0.180 S5 0.311 -0.02 0.789 S6 0.555 0.233 I6 0.551 0.413 I12 0.298 0.695 I12 0.235 0.684 S5 0.527 0.662 I8 0.416 0.644 I8 0.486 0.606 I17 0.193 0.638 I17 0.272 0.532 S5 0.514 0.614 I15 0.407 0.559 Self-rating 5.973 2.102 1.396 9.313 1.588 8.861 1.581 % Variance 22.123 7.785 5.175 34.493 5.881 32.819 5.858 of disease activity. This instrument shows a high internal consistency of the LSI, with a Cronbach alpha of 0.862. Furthermore, a contingency analyses shows agreement between the medical report and the patient self-report on the same day for each of the lupus symptoms included in the LSI (difficulty breathing (p<0.004), joint pain (p<0.001), loss of appetite (p<0.003), general malaise (p<0.005), fatigue (p<0.005) and skin rash (p<0.018)). This agreement is not found on the abdominal symptoms (LSI). On the other hand, we found differences between the LSI scores of the patients with high serological ac- tivity and those of the patients with low serological ac- tivity (χ2(1)=5.302; p<0.021), with the former presenting higher scores than the latter. The LSI is a highly reliable and valid instrument for evaluating the subjective symp- toms of the disease as well as their fluctuations. The items related to this instrument are included in Table 1 too. The SLE Disease Activity Index (SLEDAI) and Sys- temic Lupus International Collaborating Clin-ics/American College of Rheumatology (SLICC/ACR) Damage was evaluated in the prior study but the data were not in- cluded in this study [8].  M. I. Peralta-Ramírez et al. / HEALTH 1 (2009) 313-319 SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/ 317 Table 3. Summary of the relationship between the different stressors and lupus symptom. 2.3. Procedure During the first week, the patients were recruited by the internist at the outpatient clinic for autoimmune diseases. At the routine check-up, the patient was given informa- tion about this study on the effects of stress and lupus and invited to participate (90% agreed). If the patient agreed, he or she was given an appointment for the first session. In the first session, the study was explained in detail, and subjects were asked to sign the consent form (99% accepted). The subjects who accepted underwent the following: 1) a clinical interview was carried out to find out basic data like age, educational level and diverse emotional problems occurring in his or her life; 2) the SLEDAI and SLICC/ACR were evaluated; 3) they were given 30 copies of the DSI and 30 copies of the LSI. Furthermore, every 15 days they were contacted by tele- phone in order to resolve any doubts about completing the questionnaires, and they were encouraged to con- tinue to fill them out. They were informed that they would have to complete the DSI and LSI at the end of the day every day for six months (This was done by all the patients, except three who left the evaluation early). Each month, they were provided with 31 IEC question- naires and 31 LSI questionnaires, personally if they lived in Granada or by mail if they lived outside of Granada. Furthermore, every 15 days they were telephoned in order to resolve any doubts about completing the questionnaires, and they were encouraged to continue to fill them out. 2.4. Statistical Analyses In a previous study published in the Journal Psychosomatic Medicine [8], 3 groups were used: G1: patients whose increase in the clinical symptomatology of the lupus was predicted by an increase in daily stressors on the same day (lag=0); G2: patients whose increase in the clinical symptomatology was predicted by an increase in daily stressors the day before and the same day (lag=0,1); G3: patients for whom daily stress did not predict any increase in the self-reported clinical symptomatology of the lupus. In the present study, data from two of the groups (G1, G2) were used for statistical analyses. Secondly, with the objective of testing what types of G1 G2 Factors that relate certain items of stress with lupus symptoms on the same day and self-rating. Factors that relate certain items of stress with lupus symptoms on the same day and self-rating. Factors that relate certain items of stress with lupus symptoms the next day and self-rating. Factor 1: 5.973 *Felt or feared being ill General malaise Fatigue Joint pain Loss of appetite Factor 2: 2.102 *Had problems in his/her relationships with other people. *Challenged someone in authority Abdominal symptoms Factor 3: 1.396 *Something related to his/her personal appearance affected him/her. Skin rash Factor 1: 9.313 *Did not organize his/her time well *Has not slept soundly *Had problems at work *Felt or feared being ill Loss of appetite Fatigue Difficulty breathing General malaise Joint pain Abdominal symptoms Factor 2: 1.588 *Bad weather affected him/her *Thought about the future *Worried about other people’s prob- lems. Skin rash Factor 1: 8.61 * Did not organize his/her time well * Has not slept soundly * Had problems at work * Felt or feared being ill Fatigue Difficulty breathing General malaise Loss of appetite Joint pain Abdominal symptoms Factor 2: 1.581 * Bad weather affected him/her * Thought about the future * Worried about other people’s problems * Something related to his/her personal appearance affected him/her.. Skin rash 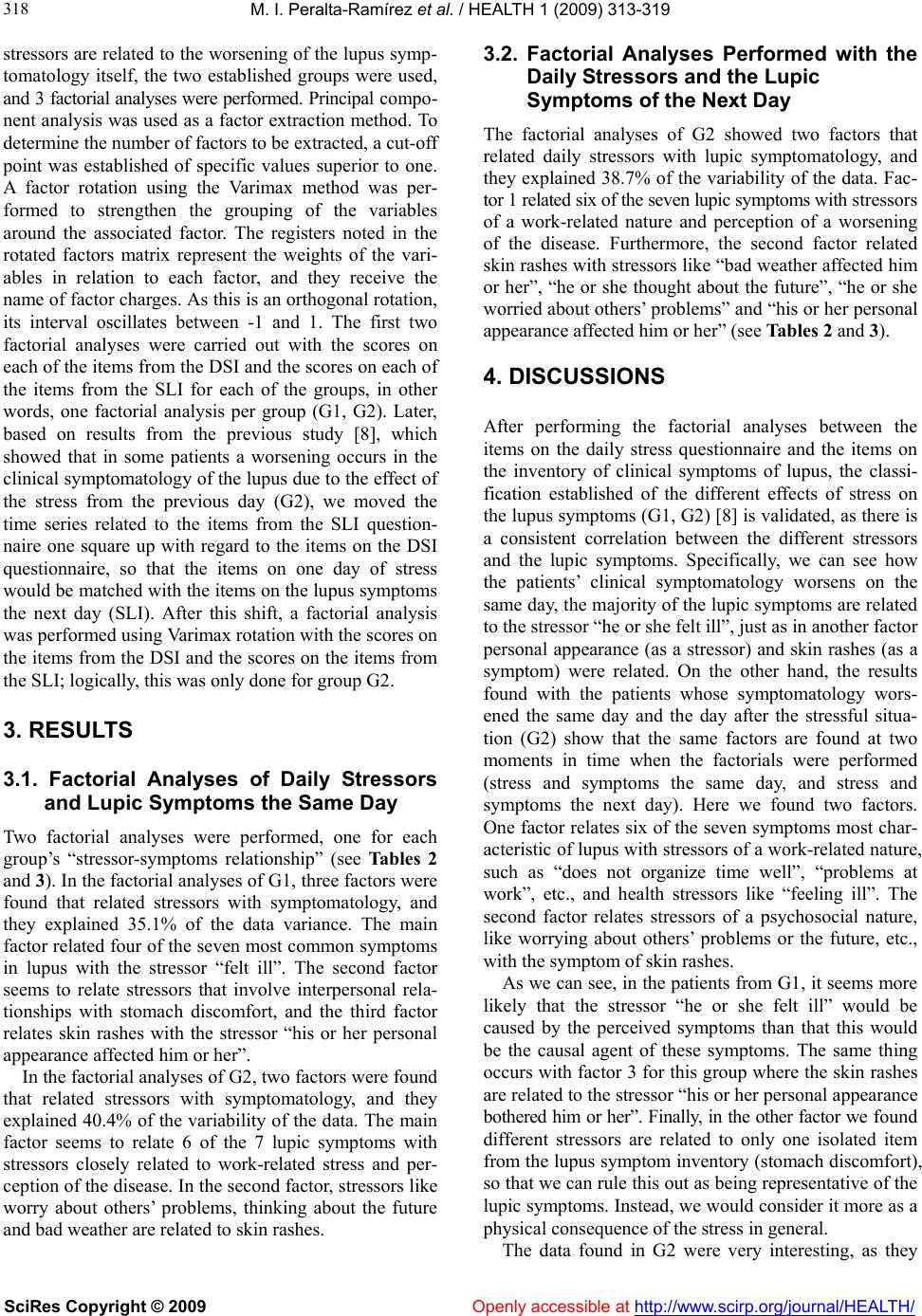 M. I. Peralta-Ramírez et al. / HEALTH 1 (2009) 313-319 SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/ 318 stressors are related to the worsening of the lupus symp- tomatology itself, the two established groups were used, and 3 factorial analyses were performed. Principal compo- nent analysis was used as a factor extraction method. To determine the number of factors to be extracted, a cut-off point was established of specific values superior to one. A factor rotation using the Varimax method was per- formed to strengthen the grouping of the variables around the associated factor. The registers noted in the rotated factors matrix represent the weights of the vari- ables in relation to each factor, and they receive the name of factor charges. As this is an orthogonal rotation, its interval oscillates between -1 and 1. The first two factorial analyses were carried out with the scores on each of the items from the DSI and the scores on each of the items from the SLI for each of the groups, in other words, one factorial analysis per group (G1, G2). Later, based on results from the previous study [8], which showed that in some patients a worsening occurs in the clinical symptomatology of the lupus due to the effect of the stress from the previous day (G2), we moved the time series related to the items from the SLI question- naire one square up with regard to the items on the DSI questionnaire, so that the items on one day of stress would be matched with the items on the lupus symptoms the next day (SLI). After this shift, a factorial analysis was performed using Varimax rotation with the scores on the items from the DSI and the scores on the items from the SLI; logically, this was only done for group G2. 3. RESULTS 3.1. Factorial Analyses of Daily Stressors and Lupic Symptoms the Same Day Two factorial analyses were performed, one for each group’s “stressor-symptoms relationship” (see Tables 2 and 3). In the factorial analyses of G1, three factors were found that related stressors with symptomatology, and they explained 35.1% of the data variance. The main factor related four of the seven most common symptoms in lupus with the stressor “felt ill”. The second factor seems to relate stressors that involve interpersonal rela- tionships with stomach discomfort, and the third factor relates skin rashes with the stressor “his or her personal appearance affected him or her”. In the factorial analyses of G2, two factors were found that related stressors with symptomatology, and they explained 40.4% of the variability of the data. The main factor seems to relate 6 of the 7 lupic symptoms with stressors closely related to work-related stress and per- ception of the disease. In the second factor, stressors like worry about others’ problems, thinking about the future and bad weather are related to skin rashes. 3.2. Factorial Analyses Performed with the Daily Stressors and the Lupic Symptoms of the Next Day The factorial analyses of G2 showed two factors that related daily stressors with lupic symptomatology, and they explained 38.7% of the variability of the data. Fac- tor 1 related six of the seven lupic symptoms with stressors of a work-related nature and perception of a worsening of the disease. Furthermore, the second factor related skin rashes with stressors like “bad weather affected him or her”, “he or she thought about the future”, “he or she worried about others’ problems” and “his or her personal appearance affected him or her” (see Tables 2 and 3). 4. DISCUSSIONS After performing the factorial analyses between the items on the daily stress questionnaire and the items on the inventory of clinical symptoms of lupus, the classi- fication established of the different effects of stress on the lupus symptoms (G1, G2) [8] is validated, as there is a consistent correlation between the different stressors and the lupic symptoms. Specifically, we can see how the patients’ clinical symptomatology worsens on the same day, the majority of the lupic symptoms are related to the stressor “he or she felt ill”, just as in another factor personal appearance (as a stressor) and skin rashes (as a symptom) were related. On the other hand, the results found with the patients whose symptomatology wors- ened the same day and the day after the stressful situa- tion (G2) show that the same factors are found at two moments in time when the factorials were performed (stress and symptoms the same day, and stress and symptoms the next day). Here we found two factors. One factor relates six of the seven symptoms most char- acteristic of lupus with stressors of a work-related nature, such as “does not organize time well”, “problems at work”, etc., and health stressors like “feeling ill”. The second factor relates stressors of a psychosocial nature, like worrying about others’ problems or the future, etc., with the symptom of skin rashes. As we can see, in the patients from G1, it seems more likely that the stressor “he or she felt ill” would be caused by the perceived symptoms than that this would be the causal agent of these symptoms. The same thing occurs with factor 3 for this group where the skin rashes are related to the stressor “his or her personal appearance bothered him or her”. Finally, in the other factor we found different stressors are related to only one isolated item from the lupus symptom inventory (stomach discomfort), so that we can rule this out as being representative of the lupic symptoms. Instead, we would consider it more as a physical consequence of the stress in general. The data found in G2 were very interesting, as they  M. I. Peralta-Ramírez et al. / HEALTH 1 (2009) 313-319 SciRes Copyright © 2009 http://www.scirp.org/journal/HEALTH/ 319 319 [2] Adams, S.J., Dammers, P.M., Saia, T.L., et al. (1994) Stress, depression and anxiety predict average symptom severity and daily symptom fluctuation in systemic lupus erythematosus. J Behav. Med., 17, 459-477. show a clear relationship between the different work and health stressors and six of the seven symptoms associ- ated with lupus. Likewise, the skin rashes are not related, as they were in the former group, with personal appear- ance, but rather with stressors regarding interpersonal relationships and worry about the future. It is noteworthy that in the group in which the worsening of the symp- toms of the disease is predicted by the stress the day before, when we performed the factorial analyses with the stress data and the symptoms of the following day, the same factors remained and with similar self-ratings. These data do make it possible to state that certain stressors of a work and interpersonal nature produce worsening in the lupic symptomatology perceived the same day and the day after experiencing the stress. [3] Wekking, E.M., Vingerhoets, A.J., Van Dam, A.P., et al. (1991) Daily stressors and systemic lupus erythematosus: A longitudinal analyses-first findings. Psychother Psy- chosom, 55,108-113. [4] Schubert, C., Lampe, A., Rumpold, G., et al. (1999) Daily psychosocial stressors interfere with the dynamics of urine neopterin in a patient with systemic lupus erythe- matosus: An integrative single-case study. Pychosom Med, 61, 876-882. [5] Da costa, D., Dobkin, P., Pinard, L., et al. (1999) The role of stress in functional disability among women with sys- temic lupus erythematosus: A prospective study. Arthritis Care and Research, 12, 112-119. The results found coincide, on one hand, with those obtained by other researchers [4,6,7], where the psycho- social stressors were related to the worsening in lupus activity. However, we were able to relate different types of stressors with certain specific symptoms of lupus, finding a great effect of the stressors related to work overload and to the perception of the illness itself. Fur- thermore, we went one step further in which we can de- fine what types of stressors are related to a certain sym- ptomatology. One piece of data which stands out is that skin rashes are not associated with other lupic symptoms in their relationship with the stressors. Instead, they are related to interpersonal relationship stressors. [6] Schubert, C., Lampe, A., Geser, W., et al. (2003) Daily psychosocial stressors and cyclic response patterns in urine cortisol and neopterin in a patient with systemic lupus erythematosus. Psyc ho neuroendocrinolog y , 28, 459-473. [7] Pawlak, C., Witte, T., Heiken, H., et al. (2003) Flares in patients with systemic lupus erythematosus is associated with daily psychological stress. Psychother Psychosom, 72, 159-165. [8] Peralta-Ramirez, M.I., Jimenez-Alonso, J., Godoy-Garcia, J.F., and Perez-Garcia, M. (2004) The effects of daily stress and stressful life events on the clinical symptoma- tology of patients with lupus erythematosus. Psychosom Med., 66, 788-94. In conclusion, this study highlights the importance of certain stressors in approaching stress in patients with lupus. Knowing which stressors are most related to the worsening of the symptoms provides us with guidelines for action and intervention in the diverse psychological therapies that are being conducted with the objective of providing lupus patients with psychological strategies for controlling stress and other related emotional vari- ables [12-14]. Furthermore, the results obtained are an important tool for the medical specialist who works with these patients, as he or she can provide information of a preventative nature to patients, emphasizing the impor- tance of avoiding work overload and controlling any possible interpersonal conflicts. Finally, the results found in this study corroborate the results found in the previous study published in Psychosomatic Medicine [8]. [9] Tan, E.M., Cohen, A.S., Fries, J.F., Masi, A.T., McShane, D.J., Rothfield, N.F., Schaller, J.G., Talal, N., and Win- chester, R.J. (1982) The revised criteria for the classifica- tion of systemic lupus erythematosus. Arthritis Rheum, 25, 1271-7. [10] Peralta, M.I., López, F., Godoy, J.F., Godoy, D., Sánchez, M.B., and Pérez, M. (2002) Validación de la detección de cambio del inventario de estrés cotidiano. Psicología Conductual, 10, 343-354. [11] Peralta-Ramírez, M.I., Verdejo García, A., Muñoz, M.A., Sabio Sánchez, J.M., Jiménez-Alonso, J., and Pérez García, M. (2007) Lupus symptoms inventory (LSI): Develop- ment and validation of a self-evaluation inventory of the subjective symptoms of systemic lupus erythematosus. Journal of Clinical Psychology in Medical Settings, 344-350. [12] Greco, C.M., Rudy, T.E., and Manzi, S. (2004) Effects of a stress-reduction program on psychological function, pain, and physical function of systemic lupus erythema- tosus patients: A randomized controlled trial. Arthritis Rheum, 15, 625-34. 5. ACKNOWLEDGMENTS [13] Haupt, M., Millen, S., Janner, M., et al. (2005) Improve- ment of coping abilities in patients with systemic lupus erythematosus: A prospective study. Ann Rheum Dis., 64, 1618-1623. To the patients with lupus who participated in this study. Financial support is gratefully acknowledged from the National Spanish ‘‘I+D’’ Projects SEJ2007-61857. [14] Peralta-Ramírez, M.I., Robles-Ortega, H., Navarrete- Navarrete, N., and Jiménez-Alonso, J.F. (2009) Aplicación de la terapia de afrontamiento del estrés en dos poblaciones con alto estrés: Pacientes crónicos y personas sanas. REFERENCES [1] Herrmann, M., Scholmerich, J., and Straub, R.H. (2000) Stress and rheumatic diseases. Rheum Dis. Clin. North Am., 26, 737-63. Openly accessible at |

