Health
Vol.5 No.5(2013), Article ID:31939,5 pages DOI:10.4236/health.2013.55118
Social capital and health literacy in Taiwan
![]()
1Department of Health Care Administration, Oriental Institute of Technology, New Taipei City, Taiwan; *Corresponding Author: FL008@mail.oit.edu.tw
2Center for General Education, National Defense Medical Center, Taipei, Taiwan
3Department of Industrial Technology Education, National Kaohsiung Normal University, Kaohsiung, Taiwan
4National Science and Technology Museum, Kaohsiung, Taiwan
Copyright © 2013 Hsieh-Hua Yang et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 18 March 2013; revised 20 April 2013; accepted 10 May 2013
Keywords: Social Capital; Health Literacy; Taiwan; Area Sampling
ABSTRACT
The argument of this study is that social capital is a key factor of health literacy. Data came from an island-wide sample. Position generator was adopted to measure social capital. A regression model is constructed to test the social capital which is known as a robust predictor of health literacy after controlling gender, age, education, income, and health communication ability. The results reveal that female, higher education, and better health communication ability are also correlated with health literacy. Implications for public health are discussed.
1. INTRODUCTION
Research during the past 15 years has shown that those with limited health literacy skills have higher health care costs [1], use health care services more frequently or improperly [2-4], have poor understanding of chronic disease [4,5], have barriers to fully understanding one’s health, illness and treatment [6], cannot adherent to medication regimens [7-9], affect health behaviors [10], tend to be less capable of properly caring for themselves [11, 12], and influence health status.
Lee et al. indicated that the current literature in which individuals are treated as isolated and passive actors, and low health literacy is considered simply as an individual trait independent of support and resources in an individual’s social environment [13]. They suggested that research needs to take into account social support that people can draw on when problems arise due to their health literacy limitations. Other researchers suggested that social networks and diffusion [14,15] played a key role in health knowledge, and social capital [16] dimensions also covariate with health literacy. And it is argued that social capital is a key factor of health literacy.
2. LITERATURE REVIEW
2.1. Health Literacy
Health literacy was defined as “degree to which individuals have the capacity to obtain, process, and understand basic health information and services to make appropriate health decisions” [17]. With chronic illnesses replacing infectious diseases as the leading causes of death, prevention of disease has taken the forefront in public health [18]. There was a shift in the emphasis on public health in response to the new risk factors, and health promotion initiatives for preventing people from adopting high-risk lifestyles came into fashion. The Ottawa charter for health promotion states that ‘health is created in the context of everyday life, where people live, love, work and play’ [19]. Health literacy has been redefined as the ability to make sound health decisions in the context of everyday life at home, in the community, at the workplace, in the healthcare system, the market place and the political arena [20]. And the assessment of health literacy was suggested to include health promotion, health protection, disease prevention, health-care maintenance, and system navigation [21].
The demographic characteristics are associated with health literacy. The 2003 assessment in the United States [22] revealed that women had higher average health literacy than men, adults who were ages 65 and older had lower average health literacy than adults in younger age groups, adults who had graduated from high school or obtained a GED, average health literacy increased with each higher level of educational attainment, and adults living below the poverty level had lower average health literacy than adults living above the poverty threshold. The assessment in Canada [21] confirms that average health literacy varies significantly by age and education.
2.2. Social Capital
The sources of social capital may trace to Pierre Bourdieu, James Coleman and Robert Putnam [23]. Portes suggests that social capital means the ability to secure benefits through membership in networks and other social structures [24]. Woolcock classified the nature of network relations and the levels at which social capital applies [25]. Lin’s theory [26] is grounded in the classic tradition of capital theories that explicate the nature of various types of capital and how each generates returns to an actor. It defines social capital as “resources embedded in a social structure which are accessed and/or mobilized in purposive actions” [26]. Thus, social capital contains three elements: resources embedded in a social structure; accessibility to such social resources by individuals; and use or mobilization of such social resources by individuals in purposive actions.
In Chinese society, individual ties that people build and maintain among themselves through various connections such as family, clan, clique, friends, classmate, and colleagues, are termed in Chinese as “Guanxi” [27]. Guanxi, or interpersonal connections is the social structure for fulfilling moral and ethical obligations to one’s family and pseudofamily. This kind of resources has been termed “face” (mian zi) [28]. Face giving from friends and neighbors is important when the men had to rely on popular support for carrying out their duties in public domains. Face giving of this sort was also important when the men tried to mobilize tangible resources from the friends and neighbors on behalf of their families or pseudo families. In this sense, having face means having quanxi capital, or the capacity to mobilize social resources from guanxi networks; and losing face means lacking guanxi capital, or the incapacity to mobilize resources through guanxi networks.
The social capital theory has specifically proposed that access to and use of social resources embedded in social networks can have two types of outcomes, instrumental and expressive returns. For instrumental action, there are three possible returns: economic, political, and social. For expressive action, social capital is a means to consolidate resources and to defend against possible resource losses. Three types of return may be specified: physical health, mental health, and life satisfaction.
There are two methodologies used to measure access to social capital, name generators and position generators. Position generator was proposed by Lin and associates [29]. This measurement samples positions in a hierarchical structure, rather than sampling ego-centered interpersonal ties. To the extent that social capital reflects embedded resources in the structure, then this approach should yield meaningful information regarding ego’s access to such structurally embedded resources. From the responses, it becomes possible to construct three indicators. Range is the distance between the highest and lowest accessed positions, and it represents the accessibility to different hierarchical positions in the society. Extensity is the number of positions accessed and it indicates the heterogeneity of accessibility to different positions. Upper reachability indicates the prestige or status of the highest position accessed.
There is a large literature about social capital and health, yet little research exists on social capital and health literacy.
3. MATERIALS AND METHODS
The sampling frame was island-wide and composed of a stratified (by administrative district) probability sample of over 15 years old persons including outlying islands and mountain townships of Taiwan. The over-all criterion that should be applied in choosing a sampling design is to so design the sample that it will yield the desired information with the reliability required at a minimum cost; or, conversely, that at a fixed cost it will yield estimates of the statistics desired with the maximum reliability possible [30]. Because a complete frame of reference was not available, area sampling method was adopted. An area sampling is a method in which the area to be sampled is subdivided into smaller blocks which are selected at random and then subsampled or fully surveyed. The entire 1100 sample came from 17 counties, 7 cities and 1 island. There were 2 respondents who did not complete the questionnaire.
The questionnaire for generating social capital was adopted from [31]. The respondents were asked “among your relatives, friends, or acquaintances, are there people who have the following jobs?”. Following the questions were fifteen “job” positions sampled from two structural dimensions: occupational prestige and class. Three indexes were constructed from the three position-generator items, extensity, upper reachability, and range. These three measures of position data were highly correlated, a composite variable was constructed. A factor score, as Table 1, was computed for both male and female respondents as a weighed sum of the three measures (0.02 extensity +0.50 range +0.51 upper reachability). Both range and upper reachability carried much more weight than extensity. This composite variable was social capital in this study.
A validated instrument was administered to measure health literacy. This instrument consists of 5 health-related items, 4 disease-related items, and 3 drug-related items. Health-related items are five servings of vegetables and fruits per day, ideal body weight, fitness, influenza vaccine, pop smear. Disease-related items are coronary artery, prostate, hormone, and menopause. Drug-
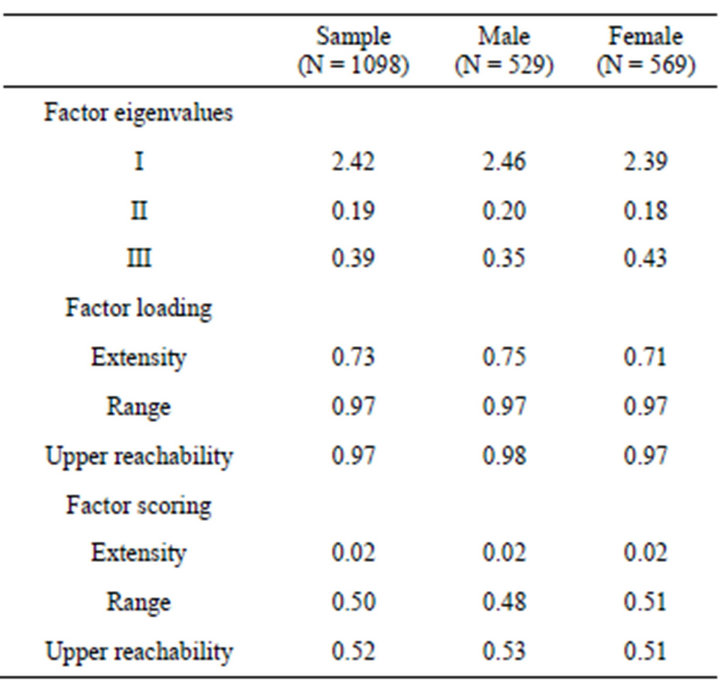
Table 1. Factor structures of access to social capital.
related items are nicotine, antibiotics, and cholesterol. Then, these 12 items made up the scale, and five-point fully semantically anchored scales (“1 = never heard”, “2 = slightly sure”, “3 = moderately sure”, “4 = very sure”, “5 = completely sure”) were used for evaluation.
Health communication ability was measured as the ability to communicate in a clinical setting. The instrument consists of 6 items, and five-point scales ranging from impossible to possible were used. Gender, age, education, and income per month are also included as control variables.
4. RESULTS
The results are presented as below. The description of participants is in Table 2, and regression model in Table 3.
The participants are 529 males and 569 females of average aged 35. Most of them are graduated from university, and over half have income ranging from NTD20000 to NTD60000 per month. They have rather good health communication ability, and social capital.
In Table 3, social capital is regressed on health literacy, and age, gender, education, income, and health communication ability are included as control variables. The result shows that social capital is a good predictor of health literacy. And females have higher health literacy than males, the higher educated have higher health literacy, but not age and income. Further, people who have higher health communication ability will have higher health literacy. The R square is 18.5%.
5. DISCUSSION AND CONCLUSIONS
Lin proposed that these two ingredients reflect differ-
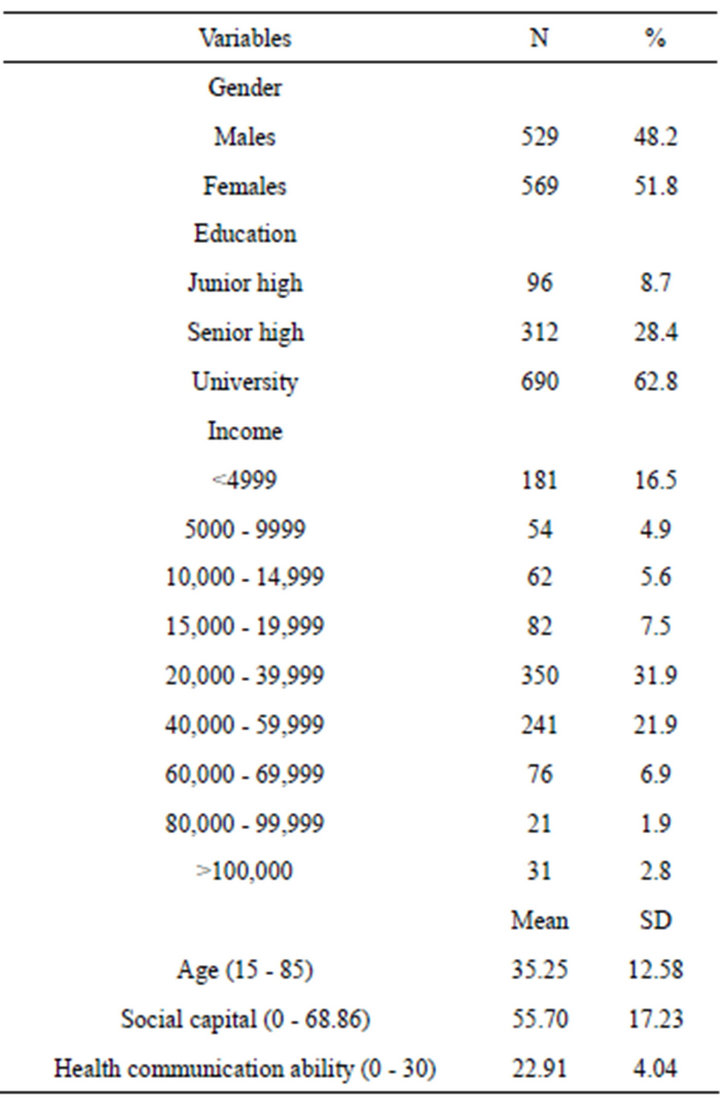
Table 2. Description of participants.
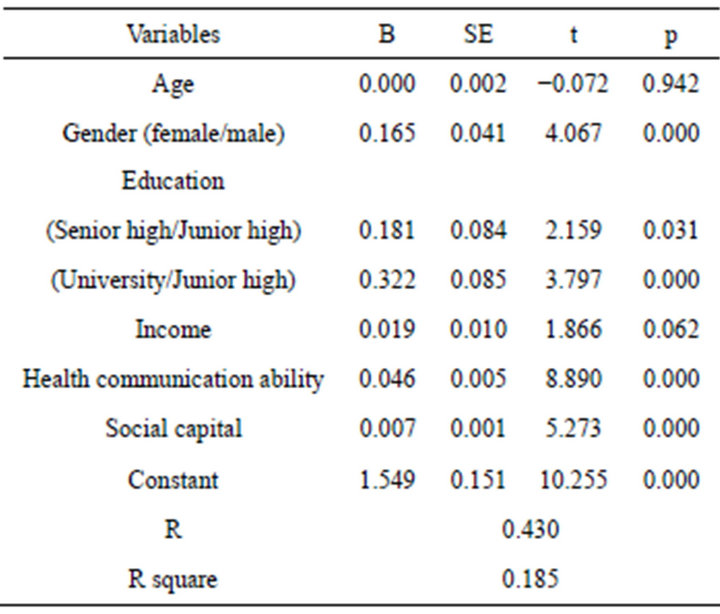
Table 3. Regression model of health literacy.
ential levels of analysis [26]. At the mesostructural level, social capital captures the extent to which individuals have differential accessibility to collective resources. At the microaction level, social capital captures how accessed resources are differentially mobilized by individuals in conjunction with specific actions. Thus, a social capital theory must contain and demonstrate the meso-micro linkage and the dynamic interactive effects between structure and action. The positions were sampled from two structural dimensions: occupational prestige and class. Furthermore, the return of different accessibility was positively correlated with individual health literacy. It is concluded that the theory is suitable for explaining health literacy.
The mechanisms that embedded resources in social networks will enhance the health outcomes were proposed by Lin [26]. For one, it facilitates the flow of information and increases the health information. Second, these social ties may exert influence on the actors. The actors may be influenced by their friends in taking care of their health. Some social relations with higher prestige and positions may carry more resources and exercise greater power of influence. Third, social resources may be conceived as certifications of the individual’s social credentials. The information offered by these relations may exert powerful influence. And the last, social relations are expected to reinforce identity and recognition.
Comparing with the decreasing tendency by age and income of a Canadian [21] or an American investigation [22], the results are different. In this study, among demographic characteristics, age and income are not correlated with health literacy. In Taiwan, health is a basic human right. Health is not just without disease, but also the social function of individuals with full and complete life-cycle tasks. To enable people to actively care about their community health, and echoed the World Health Organization Health City concept, the department of health began to promote healthy community program since 1999 [32]. Through empowerment, people participate in the program and utilize the community resources to build a healthy environment. As the result, there is no difference of health literacy among each age or income group.
REFERENCES
- Chou Howard, D.H., Gazmararian, J. and Parker, R.M. (2005) The impact of low health literacy on the medical costs of medicare managed care enrollees. American Journal of Medicine, 118, 371-377. doi:10.1016/j.amjmed.2005.01.010
- Baker, D.W., Parker, R.M., Williams, M.V., Clark, W.S. and Nurss, J.R. (1997) The relationship of patient reading ability to self-reported health and the use of health services. American Journal of Public Health, 87, 1027-1030. doi:10.2105/AJPH.87.6.1027
- Scott, T.L., Gazmararian, J.A., Williams, M.V. and Baker, D.W. (2002) Health literacy and preventive health care use among medicare enrollees in a managed care organization. Medical Care, 40, 395-404. doi:10.1097/00005650-200205000-00005
- Williams, M.V., Baker, D.W., Parker, R.M. and Nurss, J.R. (1998) Relationship of functional health literac to patient’s knowledge of their chronic disease: A study of patients with hypertension and diabetes. Archives of Internal Medicine, 158, 166-172. doi:10.1001/archinte.158.2.166
- Gazmararian, J.A., Williams, M.V., Peel, J. and Baker, D.W. (2003) Health literacy and knowledge of chronic disease. Patient Education and Counseling, 51, 267-275. doi:10.1016/S0738-3991(02)00239-2
- Kalichman, S.C., Benotsch, E., Suarez, T., Catz, S., Miller, J. and Rompa, D. (2000) Health literacy and health-related knowledge among persons living with HIV/AIDS. American Journal of Preventive Medicine, 18, 325-331. doi:10.1016/S0749-3797(00)00121-5
- Wolf, M.S., Davis, T.C., Osborn, C.Y., Skripkauskas, S., Bennett, C.L. and Makoul, G. (2007) Literacy, self-efficacy, and HIV medication adherence. Patient Education and Counseling, 65, 253-260. doi:10.1016/j.pec.2006.08.006
- Chew, L.D., Bradley, K.A., Flum, D.R., Cornia, P.B. and Koepsell, T.D. (2004) The impact of low health literacy on surgical practice. The American Journal of Surgery, 188, 250-253. doi:10.1016/j.amjsurg.2004.04.005
- Baker, D.W., Parker, R.M., Williams, M.V. and Scott, W.C. (1998) Health literacy and the risk of hospital admission. Journal of General Internal Medicine, 13, 791- 798. doi:10.1046/j.1525-1497.1998.00242.x
- LeVine, R.A., LeVine, S.E., Rowe, M.L. and Schnell-Anzola, B. (2004) Maternal literacy and health behavior: A Nepalese case study. Social Science & Medicine, 58, 863- 877. doi:10.1016/S0277-9536(03)00261-2
- Davis, T.C., Arnold, C., Berkel, H.J., Nandy, I., Jackson, R.H. and Glass, J. (1996) Knowledge and attitude on screening mammography among low-literate, low-income women. Cancer, 78, 1912-1920. doi:10.1002/(SICI)1097-0142(19961101)78:9<1912::AID-CNCR11>3.0.CO;2-0
- Kalichman, S.C., Ramachandran, B. and Catz, S. (1999) Adherence to combination antiretroviral therapies in HIV patients of low health literacy. Journal of General Internal Medicine, 14, 267-273. doi:10.1046/j.1525-1497.1999.00334.x
- Lee, S.-Y.D., Arozullah, A.M. and Cho, Y.I., (2004) Health literacy, social support, and health: A research agenda. Social Science & Medicine, 58, 1309-1321. doi:10.1016/S0277-9536(03)00329-0
- Andrzejewski, C.S., Reed, H.E. and White, M.J. (2009) Does where you live influence what you know? Community effects on health knowledge in Ghana. Health & Place, 15, 228-238. doi:10.1016/j.healthplace.2008.05.002
- Macario, E., Emmons, K.M., Sorensen, G., Hunt, M.K. and Rudd, R.E. (1998) Factors influencing nutrition education for patients with low literacy skills. Journal of the American Dietetic Association, 98, 559-564. doi:10.1016/S0002-8223(98)00125-4
- Almgren, G., Magarati, M. and Mogford, L. (2009) Examining the influences of gender, race, ethnicity, and social capital on the subjective health of adolescents. Journal of Adolescence, 32, 109-133. doi:10.1016/j.adolescence.2007.11.003
- Institute of Medicine (2004) Health Literacy: A Prescription to end confusion. National Academies Press, Washington DC.
- Satcher, D. and Eve, J.H. (2007) The public health approach to eliminating disparities in health. American Journal of Public Health, 98, 400-403. doi:10.2105/AJPH.2007.123919
- WHO (1986) Ottawa charter for health promotion. Geneva.
- Kickbusch, I., Wait, S. and Maag, D. (2006) Navigating health: The role of health literacy. Alliance for Health and the Future, International Longevity Centre, London. http://www.ilcuk.org.uk/files/pdf_pdf_3.pdf
- Health Literacy in Canada (2007) Initial results from the international adult literacy and skills survey. Ottawa.
- Kutner, M., Greenberg, E., Jin, Y. and Paulsen, C. (2006) The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy (NCES 2006- 483). US Department of Education, National Center for Education Statistics, Washington DC.
- Hawe, P. and Shiell, A. (2000) Social capital and health promotion: A review. Social Science & Medicine, 51, 871- 885. doi:10.1016/S0277-9536(00)00067-8
- Portes, A. (1998) Social capital: Its origins and applications in modern sociology. Annual Review of Sociology, 24, 1-24.
- Woolcock, M. (1998) Social capital and economic development: Toward a theoretical synthesis and policy framework. Theory and Society, 27, 151-208. doi:10.1023/A:1006884930135
- Lin, N. (2001) Social capital: A theory of social structure and action. Cambridge University Press, New York. doi:10.1017/CBO9780511815447
- Yan, Y. (1996) The flow of fifts: Reciprocity and social networks in a Chinese village. Stanford University Press, Stanford.
- King, A.Y.C. (1988) Analysis of Renqing in interpersonal relations. In: Yang, K.-S., Ed., Psychology of the Chinese, Guiguan Press, Taipei, 319-345.
- Lin, N. and Dumin, M. (1986) Access to occupations through social ties. Social Networks, 8, 365-385. doi:10.1016/0378-8733(86)90003-1
- Hansen, M.H. and Hauser, P.M. (1945) Area sampling— Some principles of sample design. Public Opinion Quarterly, 9, 183-193. doi:10.1086/265732
- Lin, N., Fu, Y. and Hsung, R.M. (2001) The position generator: Measurement techniques for investigations of social capital. In: Lin, N., Cook, K. and Burt, R.S., Eds., Social Capital: Theory and Research, Walter de Gruyter, New York, 57-81.
- http://www.bhp.doh.gov.tw/BHPnet/Web/Index/Index.aspx

