Food and Nutrition Sciences
Vol. 4 No. 10A (2013) , Article ID: 37865 , 7 pages DOI:10.4236/fns.2013.410A011
Recurrent Upper Respiratory Tract Infections in Children; The Influence of Green Vegetables, Beef, Whole Milk and Butter
![]()
Department of Pediatrics, Ziekenhuis Groep Twente, Hengelo, The Netherlands.
Email: e.gaagvander@zgt.nl
Copyright © 2013 Loes G. H. Ten Velde et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received June 27th, 2013; revised July 27th, 2013; accepted August 4th, 2013
Keywords: Nutrients; Respiratory Infections; Common Cold; Dairy Products; Vegetables
ABSTRACT
Background: Immunological mechanism and dietary nutrients are important mediators in the health of children. In this intervention study a dietary advice is given to children between 1 and 6 years of age with recurrent respiratory tract infections. Could a change in nutrient intake result in an altered clinical outcome? Design: In this prospective cohort study 61 children were included and evaluated at a paediatric outpatient clinic. The control group consisted of 32 children included at an infant welfare centre. The patient group followed the dietary advice (green vegetables, beef, whole milk, full-fat butter) for three months, in which parents filled out their dietary intake and health status on a daily basis. A follow up form was filled out by the parents 3 months after completion of the study period. For statistical analysis the programme SPSS version 15.0 was used. Results: In the patient group there was a statistical significant reduction in days with a respiratory infection (15.7 to 11.5 days a month), subfebrile temperature days (1.9 to 0.5 days a month) and febrile temperature days (1.0 to 0.7 days a month) compared to the control group. Also, antibiotic use decreased significantly. No significant changes were measured in body mass index. Conclusions: A change of diet towards green vegetables, beef, whole milk and full-fat butter has positive health effects in children. This diet may work by adding nutrients to optimize immunological mechanisms. There were no adverse effects and it can be utilized by general pediatricians and general practitioners.
1. Introduction
Children with recurrent upper respiratory tract infections without immunological disorders are common among the general population, but are difficult to offer treatment options, since no abnormalities are found. These children are a major problem for parents, general practitioners and pediatricians. Parents seeking help, have to stay away from their work to take care for their sick child. General practitioners encounter these problems first and often send the most complicated or persistent children to a pediatrician. After extensive medical history, physical examination, and laboratory (blood) tests, in 50% no cause for the infections can be found [1]. The current treatment of children with recurrent upper respiratory tract infections is to explain to parents that it is a normal phase in the development and that the child eventually will grow over it [2].
The functioning of the immune system is dependent on environment, age, and nutritional status [3]. Nutrients play an important role in immune system function, so infectious diseases can be prevented when nutritional status is adequate [4]. Micronutrient deficiencies are difficult to detect, only signs of iron deficiency are a common finding when diets are insufficient. In previous studies, we investigated the dietary intake of children with recurrent respiratory infections and healthy control children. No quantitative differences could be found in the major food groups like meat, dairy, fruit or vegetables [5]. When looked into detail, qualitative differences could be found [6]. The children with recurrent infections ate less beef and less green vegetables, both products with high nutrient content [7].
We composed a dietary advice on information of the NEVO table 2010 [7]. This is a Dutch reference manual which contains information of the nutrient content of all kinds of food. Nutrients which are supporting the immune system were chosen for the dietary advice. Products as green vegetables, beef, whole milk and full-fat butter all related with immune system function. Green vegetables contain more zinc, vitamin A and vitamin C than other different colored vegetables [7]. These nutrients have sustained supportive effects on the immune system in children [8-12]. Beef contains more iron, zinc, vitamin A and vitamin E compared to other kinds of meat [7]. All these nutrients play a role in phagocytic function and have immune stimulating effects on lymphocytic cells, especially T-lymphocytic activities [13-16]. They also play a role in immune stimulating and antiviral mechanisms which are effective in upper respiratory tract infections [16]. Furthermore, whole milk contains more vitamin A and B-caroten compared to semi-skimmed milk and skimmed milk and has several health effects [7,17,18]. Full-fat butter is a natural butter, so natural components like vitamin A, D and E can support the immune system [19-21]. In this study we investigated whether change of diet with qualitative high nutrient content would lead to a decrease in upper respiratory tract infections in children without a medical cause for these infections.
2. Subjects and Methods
2.1. Study Design
The study was a prospective cohort study performed at a general pediatric outpatient clinic of a general hospital in The Netherlands. Children with recurrent upper respiratory tract infections were referred by a general practitioner and evaluated by a pediatrician. Patients were included from October 2008 to June 2010, evenly distributed over the seasons. The patients were followed for 7 months.
2.2. Study Population
Children between one and six years of age with recurrent upper respiratory infections were included. They should have respiratory infections for at least 10 days per month (noted by a diary for the last month), and/or have at least 1 period of fever a month for the past three months. Exclusion criteria were met when the children had treatable laboratory abnormalities on immunologic evaluation. Children with other complicated medical disorders like congenital syndromes, heart diseases or rheumatic disorder were excluded. Mild medical disorders like constipation, dysfunctional voiding or wheezing were no exclusion criteria. When the children used medication they were excluded, except for the use of laxantia, aerosols, anti-histamines or antibiotics.
The control group was included at a welfare health centre, Oldenzaal, The Netherlands. All patients gave informed consent before starting the diet.
2.3. Intervention
The patient group was advised to follow a dietary advice which contains green vegetables, beef, whole milk and full-fat butter. No other advice was given, they could eat everything they wanted. We advised normal child portions for all recommended food products; green vegetables (five times a week, 2 - 3 tablespoons every day = 1 - 1.5 oz), beef (three times a week, 1 - 2 tablespoons every day = 0.5 - 1 oz), whole milk (every day one cup of 200 ml = 7 oz), and full-fat butter (every day 1 - 2 times butter on sandwich).
The dietary advice should be followed for three months. Each item of the advice (green vegetables, beef, whole milk and full-fat butter) counted for 25%, when eaten all products on the advised way, a score of 100% per week was given. When eaten less than the advised way, a subsequent percentage was scored. For example; when the child ate 4 times a week green vegetables, he would score 20% out of 25%.
2.4. Measurements
The patient group was evaluated for immunologic disorders as an explanation for their recurrent infections. We used the Dutch flow chart for evaluation of immunologic disorders [22]. The patient group was weighed and measured at the start and after 3 months of following the dietary advice to observe weight gain while ingesting full fat products.
For evaluating the compliance and infection characteristics, parents would fill out a diary for 4 months. Every day, they noted what kind of vegetables, meat, butter or milk their child ate and drank. They also noted if he/she had a respiratory infection and what his /her temperature was. Sub febrile temperature is defined as 37.5˚C - 38.4˚C, febrile temperature as ≥38.5˚C.
The parents filled it out for 1 month without being informed about the dietary advice and for 3 months after being advised. After the 3 months of dietary advice, the child was measured for weight and height again. The results were discussed with the parents and they could choose for themselves if they returned to their pre-advice eating habits or they continued eating according to the advice.
Three months after this visit, all parents received a questionnaire about the health, use of antibiotics and dietary habits of their child at that moment.
To compare the old and new dietary habits and health aspects with the healthy population, the control group filled out the same diary for 3 months without the dietary advice. They wrote down the kind of vegetables, meat, butter or milk their child ate and drank and also if he/she had a respiratory infection and what his /her temperature was. The control parents also received a questionnaire about use of antibiotics.
2.5. Statistics
Patient characteristics were evaluated with Student’s T-test and Chi Square test. For repeated measurements in patient group we used mixed model analysis (repeated measurement analysis). The dietary advice was evaluated with Pearson and Spearman tests. For statistical analysis the program SPSS version 15.0 was used, p < 0.05 is statistically significant.
2.6. Ethics
We consulted the CCMO (Central Committee on Research involving Human Subjects) for ethical evaluation. They judged the dietary advice was not a major change in life style and did contain “normal” food, therefore the study did not need to be evaluated by an ethical committee.
3. Results
3.1. Descriptives
A group of 107 children were asked to participate in the study. 75 patients were included at the pediatric outpatient clinic, 32 patients at the welfare health centre. All 75 parents of the patient group agreed to participate, however, 61 finished the study. The other 14 patients agreed to start with the dietary advice but didn’t show up at the scheduled appointments. Of these patients, 6 patients did not want to follow the diet anymore, the other 8 patients did not react or couldn’t be traced by the research assistant. The patient group contains 34 boys and 27 girls, the control group 18 boys and 14 girls. The characteristics of these groups are shown in Table 1. There are no significant differences between both groups for age, gender and dietary intake. On the contrary, the amount of days with a respiratory infection, sub febrile and febrile temperature days based on diary list Baseline do differ and are shown in Table 1.
In the patient group the children were evaluated for immunologic disorders as a possible explanation for their recurrent infections. There were no anemic children found (Hb levels < 6.8 mmol/l). Laboratory results did show a reduced ferritin (<20 µg/l) at 6.7%, and a reduced IgA (<0.1 g/l) in 8.3% of the children. Furthermore 45% of the children show an increased IgE (>0.35 kU/l), and an increased IgM (0.1 - 1.5 g/l) in 21.7% of the children. An insufficient qualitative intake was suggestive in 6.7% at the children, looking at low ferritin levels, no other signs of deficiencies were found.
3.2. Main Clinical Outcomes
The patient group followed the dietary advice for three months. Results of days with respiratory infections, days with sub-febrile and febrile temperature days are shown in Figure 1. Repeated measurement analysis shows a significant reduction in days of respiratory infections (p = 0.04), sub febrile-temperature (p = 0.01) and febrile temperature (p = 0.02). The strongest significant relation is between the month without the dietary advice and the second month of the dietary advice (Table 2). The numbers of the follow up, 3 months after completion of the dietary advice, were not kept in a diary, but retrospectively estimated for the past 3 months. We evaluated if the parents could estimate adequately, by asking them retrospectively about the days of respiratory infections

Table 1. Group descriptives.
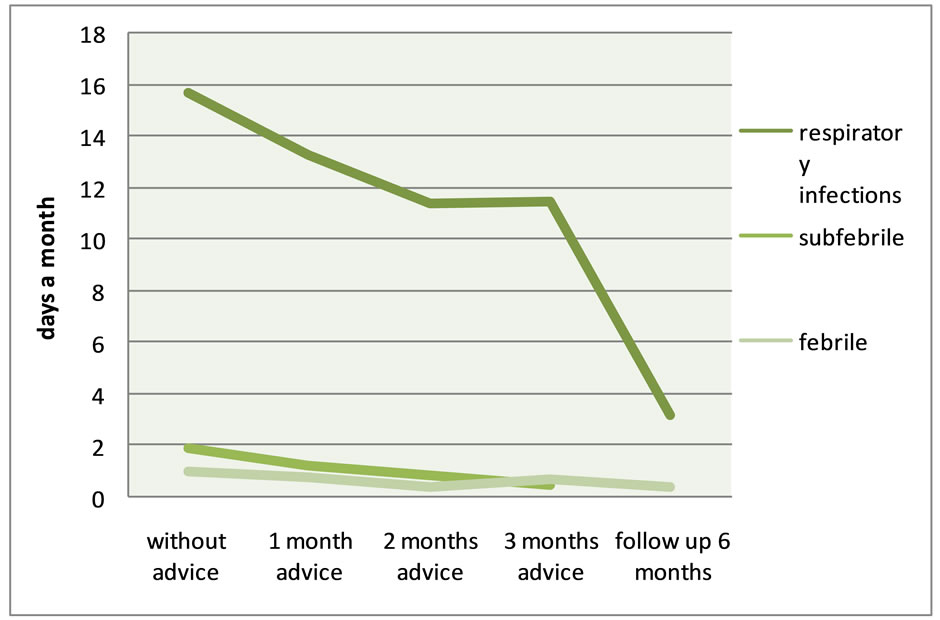
Figure 1. Patient group; Dietary advice and upper respiratory tract infections.

Table 2. Patient and control group; Data from diary lists.
their child suffered before starting the dietary advice. They mentioned a mean of 46.2 days per 3 months, representing 15.5 days a month. There is a strong correlation with the 15.7 days they noted in the diary questionnaires. They noted a mean of 3.2 days a month with respiratory infections 6 months after completion of the study. In this period, the children suffered 0.4 days a month from febrile temperature.
Antibiotic use decreased from 1.1 treatment per child in 3 months before the dietary advice to 0.2 treatments per child during the advice and 0.1 treatments in the 3 months during follow up (without a relation with the season). In this period, the compliance to the diet decreases with about 15% (Table 3).
3.3. Compliance
Table 3 shows compliance to the dietary advice in the patient group during the study period. The control group, which did not follow the dietary advice, fulfilled 35% of the dietary advice for the entire study period. This percentage was also seen in the children of the intervention group before they started the diet (Table 1). Most likely a normal standard diet for children between 1 and 6 years contains about 35% of the dietary advice.
3.4. Length and Weight
In general it is assumed that full fat products like whole milk and full-fat butter lead to weight gain. In this study the body mass index (BMI) kg/m2 shows no significant changes with Student’s T-test. Body mass index stays equal, before the diet 16.14 kg/m2, and after the diet 16.12 kg/m2. This BMI is within the normal range for children, reference values for girls are estimated at 14.15 - 17.28 and 14.30 - 17.55 for boys.
4. Discussion
Children with recurrent respiratory infections are a common phenomenon. A causal treatment for the children without a medical abnormality, besides antibiotics, is lacking at this moment. However, a dietary advice seems to be an effective and harmless intervention for these children.
In this study we show a significant decrease in days of respiratory infections (p = 0.04), sub febrile (p = 0.01) and febrile temperature (p = 0.02), and antibiotic use during 3 months of following a dietary advice. In the 3 month follow up period there is even a larger decrease in respiratory infections compared to the first 3 months.
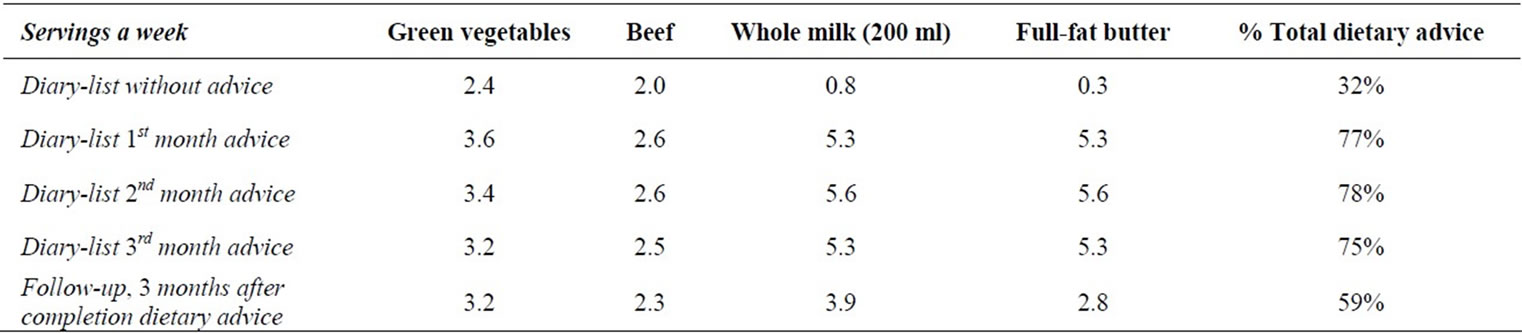
Table 3. Patient group; Compliance to the dietary advice during 6 months.
This could be due to the kind of reporting of the parents (dairies or retrospective questionnaire), or because of the time the body needs to recover from the infections. These results support the conception that nutrition can have positive effects on the health of children. The strength of the study is a dietary advice with 4 components instead of a single nutrient or supplement. Of the 4 food compounds, green vegetables were the hardest for the children to eat, as is known from the literature [23]. Full fat butter and whole milk weren’t very difficult. Another strong aspect is the role of the parents. They can assist their children by offering them food to support the natural recovering and strengthening of the body.
We realize full fat dairy products are not recommended by the American Heart Association and American Academy of Pediatrics [24]. However, there is a growing interest for the beneficial effects of full fat dairy products [18,25]. Epidemiologic studies support the contributive effects of full fat dairy products, such as the KOALA and PIAMA study. The KOALA birth cohort study shows that pre-natal maternal exposure to fatty acids protects against eczema [26]. The PIAMA study showed less asthma and wheezing at age 3 when children consumed daily full fat milk and butter [27]. Nonetheless, these were observational and no intervention studies. As far as we know, there are no studies of full fat dairy products in combination with green vegetables or beef and their influence on respiratory symptoms in children. We emphasize us advice normal, age-adequate child portions of whole milk and full-fat butter. We do not support extremely large portions of full fat dairy, we also do not support saturated fried fat or trans fat.
All four advised food compounds are rich of nutrients. It contains a combination of high energy density food (butter) and low energy density food (vegetables). Milk and beef contain mean values of energy. When all food compounds are eaten, a balanced pattern can be reached. There is evidence that whole milk would not lead to an elevated risk of weight gain in children [28], and whole milk is not associated with an increased BMI [29]. Still, we followed the children for 4 months, and not for several years.
It is difficult to calculate the exact effect of green vegetables, beef, whole milk and full-fat butter on the immune system. We directed recommendations, although every child has a different nutrient absorption. Also difficult is the measurement of the actual consumption of the diet and nutrients. Fresh vegetables contain other amounts of nutrients compared to canned, bottles or frozen vegetables. Children without eating problems are likely to eat more vegetables than children with eating problems. Nevertheless, we tried to compose a dietary pattern which could fit in daily routines of families. It was not intended to imitate vitamin supplementation, but to make parents aware of the health benefits of nutrition and conscious choices.
If this dietary advice has truly immune modulating mechanisms, then it could be measured by laboratory research. A clinical study with laboratory immunologic measurement is recommended. We only looked at the clinical outcomes. Possible mechanisms could be by Th1 mediated immunity, since this immunity is mostly used to combat viral infections [10].
The natural course of children with recurrent infections is also an important feature. When the children reach the age of about 4 years of age, the infections usually decrease. Our study population is a little younger compared to the control population. The infection rate in the control population stays the same, in our study group it is significantly decreasing. Another weakness is the study design. The study is not randomized or blinded. This was not possible in this set up. One can imagine the people who enrolled the study have more positive feelings about nutrition and the treatment and that could bias the outcome of the study. Future studies should consist of a randomized clinical trial to encounter the problems of the design of this pilot study.
5. Conclusion
A dietary advice with green vegetables, beef, whole milk and full-fat butter can lead to significant reduction of upper respiratory tract infections in children between 1 and 6 years. The precise mechanism is unknown, but it could represent a stimulating effect of nutrients on the immune system. Dietary advice is a possible treatment for children with recurrent upper respiratory tract infections, without medical abnormalities and without any causal treatment possibilities at this moment. There are some scientific limitations in this pilot study, however, the practical aspect that includes the diet into every-day family routines suits most families. Besides the feasibility, it has no side-effects, and is useful for general practitioners and pediatricians.
6. Acknowledgements
We thank Prof. Dr. J. Van der Palen, epidemiologist at Medical School Twente Enschede, for his expert statistical advices and help and Prof. H.R. Byers, Santa Barbara, USA, for critically reading the manuscript.
REFERENCES
- M. E. Conley and E. R. Stiehm, “Immunologic Disorders in Infants and Children,” 4th Edition, 1996.
- A. C. Bernard-Bonnin, “Feeding Problems of Infants and Toddlers,” Canadian Family Physician, Vol. 52, No. 10, 2006, pp. 1247-1251.
- J. L. Van den Brande, H. S. A. Heymans and L. A. H. Monnens, “Pediatrics,” 3rd Edition, Vol. 2, Elsevier, Maarssen, 2000.
- C. J. Field, I. R. Johnson and P. D. Schley, “Nutrients and Their Role in Host Resistance to Infection,” Journal of Leukocyte Biology, Vol. 71, No. 1, 2002, pp. 16-32.
- N. van Droffelaar and E. J. van der Gaag, “Can Food Intake Be a Reason for Recurrent Infections?” Samenvattingen der Voordrachten Dertigste Congres Kindergeneeskunde, 2008, p. 115.
- M. Munow and E. J. van der Gaag, “Ailing Toddlers-Is There a Relation between Behavior and Health?” Book of Abstracts 27th Annual Meeting of the European Society for Paediatric Infectious Diseases, 2009, p. 764.
- Dutch Food Center, “NEVO-Tabel 2006: Nederlands Voedingsstoffenbestand,” Dutch Food Center, The Hague, 2006.
- A. S. Prasad, “Zinc: Role in Immunity, Oxidative Stress and Chronic Inflammation,” Current Opinion in Clinical Nutrition and Metabolic Care, Vol. 12, No. 6, 2009, pp. 646-652. http://dx.doi.org/10.1097/MCO.0b013e3283312956
- K. H. Brown, J. M. Peerson, J. Rivera and L. H. Allen, “Effect of Supplemental Zinc on the Growth and Serum Zinc Concentrations of Prepubertal Children: A MetaAnalysis of Randomized Controlled Trials,” The American Journal of Clinical Nutrition, Vol. 75, No. 6, 2002, pp. 1062-1071.
- S. Maggini, S. Wenzlaff and D. Hornig, “Essential Role of Vitamin C and Zinc in Child Immunity and Health,” Journal of International Medical Research, Vol. 38, No. 2, 2010, pp. 386-414. http://dx.doi.org/10.1177/147323001003800203
- C. Jimenez, I. Leets, R. Puche, E. Anzola, R. Montilla, C. Parra, A. Aguilera and M. N. Garcia-Casal, “A Single Dose of Vitamin A Improves Haemoglobin Concentration, Retinol Status and Phagocytic Function of Neutrophils in Preschool Children,” British Journal of Nutrition, Vol. 103, No. 6, 2010, pp. 798-802. http://dx.doi.org/10.1017/S0007114509992765
- E. S. Wintergerst, S. Maggini and D. H. Hornig, “Immune-Enhancing Role of Vitamin C and Zinc and Effect on Clinical Conditions,” Annals of Nutrition and Metabolism, Vol. 50, No. 2, 2006, pp. 85-94. http://dx.doi.org/10.1159/000090495
- C. Ekiz, L. Agaoglu, Z. Karakas, N. Gurel and I. Yalcin, “The Effect of Iron Deficiency Anemia on the Function of the Immune System,” The Hematology Journal, Vol. 5, No. 7, 2005, pp. 579-583. http://dx.doi.org/10.1038/sj.thj.6200574
- B. J. Cherayil, “Iron and Immunity: Immunological Consequences of Iron Deficiency and Overload,” Archivum Immunologiae et Therapiae Experimentalis, Vol. 58, No. 6, 2010, pp. 407-415. http://dx.doi.org/10.1007/s00005-010-0095-9
- E. R. Monsen, “Dietary Reference Intakes for the Antioxidant Nutrients: Vitamin C, Vitamin E, Selenium, and Carotenoids,” Journal of the American Dietetic Association, Vol. 100, No. 6, 2000, pp. 637-640. http://dx.doi.org/10.1016/S0002-8223(00)00189-9
- I. M. Roitt, J. Brostoff and D. K. Male, “Immunology,” 5th Edition, Houten, 2000.
- A. Haug, A. T. Hostmark and O. M. Harstad, “Bovine Milk in Human Nutrition—A Review,” Lipids in Health and Disease, Vol. 6, 2007, p. 25. http://dx.doi.org/10.1186/1476-511X-6-25
- H. de B. A. Zevenbergen, M. Zeelenberg, K. van D. G. Laitinen and E. Floter, “Foods with a High Fat Quality Are Essential for Healthy Diets,” Annals of Nutrition and Metabolism, Vol. 54, No. S1, 2009, pp. 15-24. http://dx.doi.org/10.1159/000220823
- J. B. German and C. J. Dillard, “Saturated Fats: What Dietary Intake?” The American Journal of Clinical Nutrition, Vol. 80, No. 3, 2004, pp. 550-559.
- J. B. German, “Dietary Lipids from an Evolutionary Perspective: Sources, Structures and Functions,” Maternal & Child Nutrition, Vol. 7, No. S2, 2011, pp. 2-16. http://dx.doi.org/10.1111/j.1740-8709.2011.00300.x
- L. Moeyersoms, “Milkproducts,” 2003, pp. 11-17.
- E. De Vries, “Patient-Centred Screening for Primary Immunodeficiency: A Multi-Stage Diagnostic Protocol Designed for Non-Immunologists,” Clinical & Experimental Immunology, Vol. 145, No. 2, 2006, pp. 204-214. http://dx.doi.org/10.1111/j.1365-2249.2006.03138.x
- R. Havermans and A. Jansen, “Zoete Spruiten, Bittere Spruiten,” De psycholoog, 2010, pp. 11-18.
- S. S. Gidding, B. A. Dennison, L. L. Birch, S. R. Daniels, M. W. Gillman, A. H. Lichtenstein, K. T. Rattay, J. Steinberger, N. Stettler and L. Van Horn, “Dietary Recommendations for Children and Adolescents: A Guide for Practitioners,” Pediatrics, Vol. 117, No. 2, 2006, pp. 544- 559. http://dx.doi.org/10.1542/peds.2005-2374
- M. Pfeuffer and J. Schrezenmeir, “Milk and the Metabolic Syndrome,” Obesity Reviews, Vol. 8, No. 2, 2007, pp. 109-118. http://dx.doi.org/10.1111/j.1467-789X.2006.00265.x
- M. L. Notenboom, M. Mommers, E. H. Jansen, J. Penders and C. Thijs, “Maternal Fatty Acid Status in Pregnancy and Childhood Atopic Manifestations: KOALA Birth Cohort Study,” Clinical & Experimental Allergy, Vol. 41, No. 3, 2011, pp. 407-416. http://dx.doi.org/10.1111/j.1365-2222.2010.03672.x
- A. H. Wijga, H. A. Smit, M. Kerkhof, J. C. De Jongste, J. Gerritsen, H. J. Neijens, H. C. Boshuizen and B. Brunekreef, “Association of Consumption of Products Containing Milk Fat with Reduced Asthma Risk in Pre-School Children: The PIAMA Birth Cohort Study,” Thorax, Vol. 58, No. 7, 2003, pp. 567-572. http://dx.doi.org/10.1136/thorax.58.7.567
- S. Y. Huh, S. L. Rifas-Shiman, J. W. Rich-Edwards, E. M. Taveras and M. W. Gillman, “Prospective Association between Milk Intake and Adiposity in Preschool-Aged Children,” Journal of the American Dietetic Association, Vol. 110, No. 4, 2010, pp. 563-570. http://dx.doi.org/10.1016/j.jada.2009.12.025
- G. Barba, E. Troiano, P. Russo, A. Venezia and A. Siani, “Inverse Association between Body Mass and Frequency of Milk Consumption in Children,” British Journal of Nutrition, Vol. 93, No. 1, 2005, pp. 15-19. http://dx.doi.org/10.1079/BJN20041300

