International Journal of Clinical Medicine
Vol. 3 No. 7 (2012) , Article ID: 26091 , 5 pages DOI:10.4236/ijcm.2012.37112
State of the Art in Cardiac Intervention: A Case Report
![]()
Medical Research Division, New Terra Enterprises, Los Angeles, USA.
Email: allend.allen@yahoo.com
Received September 6th, 2012; revised October 6th, 2012; accepted November 20th, 2012
Keywords: Clinical Medicine; Angiography; Angioplasty; Bare Metal Stent; Drug-Eluting Stent; Collateral Circulation; Aspirin Intolerance; Emotional Stress in Hospitalized Heart Patients; Team Communication
ABSTRACT
The first acute myocardial infarction (MI) of an elderly male was determined through angiography to be due to an infarct of the circumflex artery. The angiogram also revealed chronic occlusion and diffuse disease of the left anterior descending artery (LAD). This had been compensated for by collateral circulation from the right coronary artery. Since the patient had no prior history of coronary artery disease, the chronic and collateralized disease of the LAD was presumed to be stable and this artery was not treated. Due to a history of aspirin intolerance a bare metal stent was implanted in the circumflex artery. Within hours after stenting the patient had a second acute MI. Despite no change in the angiogram, the EKG suggested that the LAD was the source of the second MI. Indeed, a drug-eluting stent implanted in the LAD resolved the patient’s signs and symptoms and he was discharged with a favorable outcome. The surprising second MI and the inconsistent stenting illustrate that when the unexpected occurs, there is no substitute for the judgment of a skilled clinician.
1. Introduction
The advent of coronary angioplasty and stenting has revolutionized interventional cardiology over the past two decades [1]. Investigations continue into the use of bare metal [2] and drug-eluting stents [3-8] in combination with antiplatelet therapy and aspirin. As is well known, coronary angioplasty carries certain risks of complications ranging from benign rupture to catastrophic events [9-18]. In a large research study [9], one or more acute major complications arose in 34 of 500 cases (6.8%). This is as compared to a primary success rate of 86%. In another study [10], restenosis at one coronary site increased the probability of restenosis at another site. This is intuitive because restenosis reflects such constant factors as the patient’s underlying atherosclerosis and compliance with medications. Usually, however, adverse events are associated with the coronary artery being treated or the implements of intervention such as a fractured guide wire [9].
What gives the present case report teaching value is an acute infarct in the left anterior descending artery (LAD) hours after stenting of the circumflex artery, despite chronic and diffuse disease in a collateralized LAD that should have been stable. The etiology remains mysterious but may be associated with the stress of the procedure and hospitalization. Another unusual aspect of the present report is inconsistent stenting. The incidence of these unusual events is not known and they are not ordinarily disclosed to patients in the United States while obtaining informed consent. For these reasons, this case report serves as a reminder that clinical medicine is very much an art, and that heuristic issues can arise during cardiac intervention. In particular, the case reported here illustrates a limited ability of angiography alone to determine the site of an acute myocardial infarction (MI). It also suggests a need to manage emotional stress during hospitalizations for the management of coronary artery disease (CAD). A further example demonstrates the need for communication between different teams of interventionists who stent a patient with a history of gastrointestinal bleeding second to aspirin therapy.
2. Case Report
A 76-year-old male was admitted to the Cardiac Care Unit of a major hospital in the United States with severe chest pain responsive to nitroglycerin and an EKG that was unremarkable except for a left axis deviation as shown in Figure 1. He had multiple risk factors for CAD but no history of CAD. After 10 hours of supportive therapy, a low level of troponin was detected in his peripheral venous blood and he was scheduled for angiography. The angiogram revealed an acute infarct in
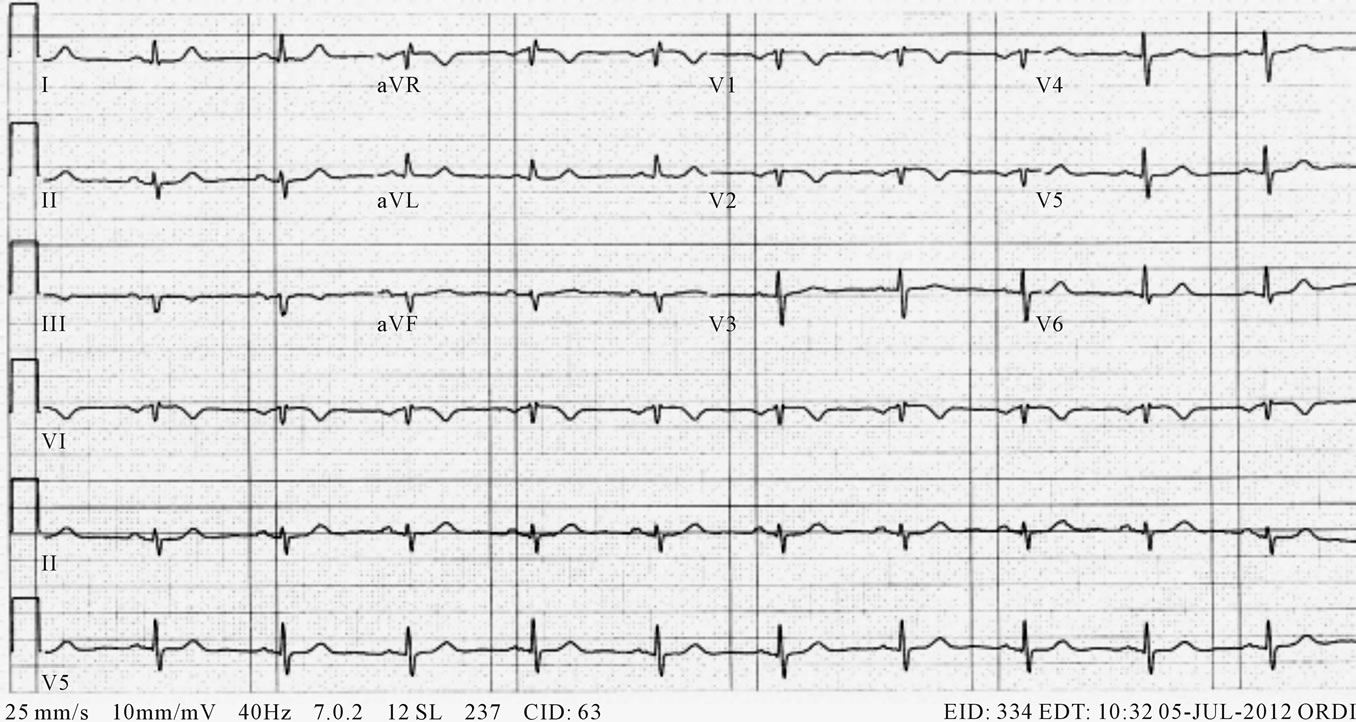
Figure 1. Unremarkable EKG during acute MI due to infarct of the circumflex artery. There is no ST-segment elevation.
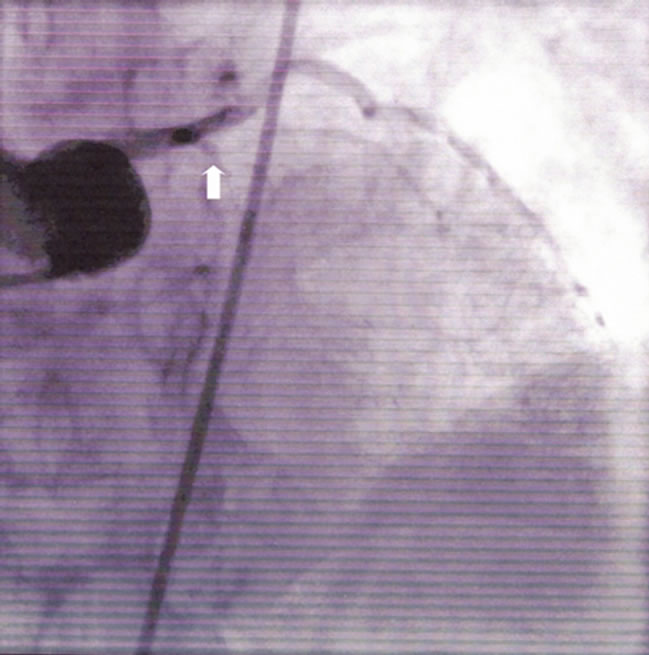
Figure 2. Chronic occlusion of the LAD (arrow) with diffuse disease. Initially asymptomatic.
his circumflex artery. It also revealed an occluded, diffusely diseased LAD fully collateralized by the right coronary artery as shown in Figures 2 and 3. The collateral circulation was presumed to be the reason that this patient had no previous history of CAD despite the diffuse disease of his LAD, which appeared to be chronic and to have developed over a period of years if not decades. Since it would have been difficult to implant a stent
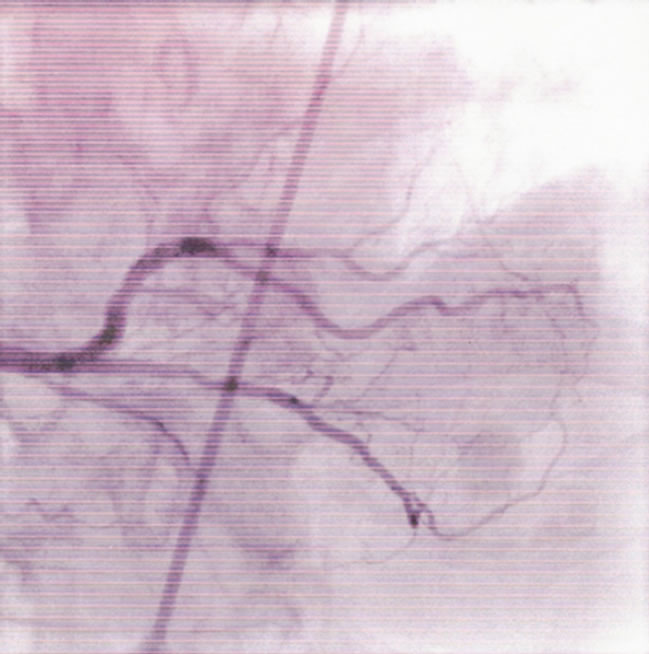
Figure 3. Collateral circulation from the right coronary artery.
in the LAD, a decision was made not to treat that artery. The circumflex artery was implanted with a bare metal stent (Medtronic Integrity) due to the patient’s history of gastrointestinal bleeding when taking aspirin.
Eight hours after his initial angioplasty, the patient again began complaining about chest pain. After another four hours, his EKG had changed to suggest an acute myocardial infarction in his LAD as shown in Figure 4.
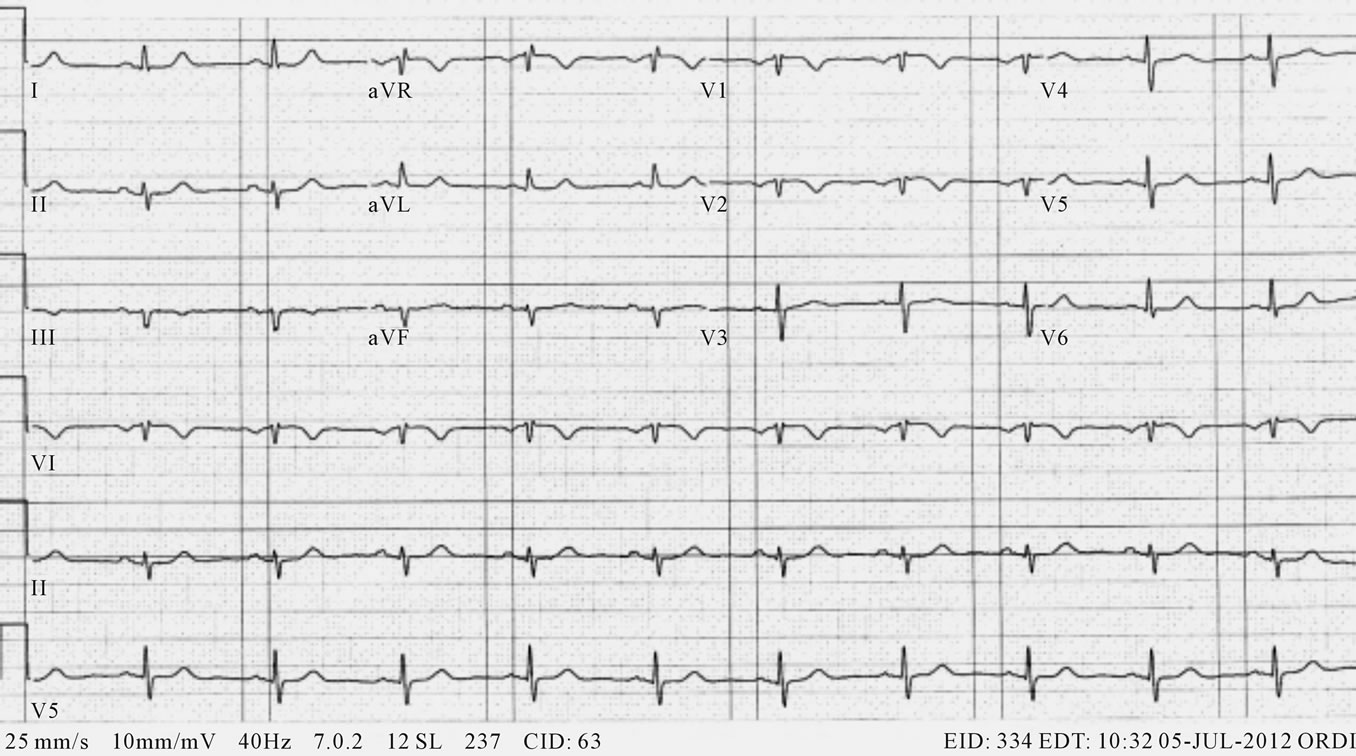
Figure 4. EKG suggesting that the second acute MI following stenting of the circumflex artery was surprisingly due to the LAD.
An emergency intervention was ordered and the second angiogram showed no change in the LAD from the previous one. Indeed, it should be clear from Figure 2 that no change would be found. Nonetheless, it was clinically clear that the LAD was now the site of an acute myocardial infarction. Consequently, a drug-eluting stent (Boston Scientific PROMUS Element Plus) was successfully implanted in the LAD, albeit with some difficulty. This resolved the patient’s signs and symptoms and he was discharged with a good outcome.
3. Discussion
Since the second angiogram failed to detect any changes in the LAD that would reflect the acute infarct, this illustrates that angiography alone has a limited ability to differentiate chronic from acute occlusion. What triggered the second myocardial infarction is a more interesting question. Unless it was just a coincidence given the patient's pre-existing risk factors, an obvious mechanism would be the physical and emotional stress of the hospital experience and the thrombogenic and vasoactive agents associated with the initial stenting procedure, any or all of which might have impaired the collateral circulation show in Figure 3. Among other stressors, the patient complained of anxiety and anger due to interactions with the nursing staff. Although stress as the etiology of Tako-Tsubo cardiomyopathy is controversial [19,20], it is well established that emotional stress can trigger a frank, acute myocardial infarction in susceptible or predisposed individuals [21-24].
Finally, one may ask why two different types of cardiac stents were implanted in this patient by the same facility on consecutive days. The first interventionist reported that, in light of the patient’s history, he had implanted a bare metal stint in the circumflex artery in order to minimize the time the patient would need to take aspirin. An attending cardiologist, however, was of the opinion that a fourth-generation, drug-eluting stent would not have required aspirin therapy for longer than a bare metal stent, and would have preferred a drug-eluting stint in the circumflex artery to reduce the risk of restenosis. A consulting cardiologist, by contrast, felt that a bare metal stent should have been implanted in the LAD once this type of stent had been implanted in the circumflex artery. The interventionist who implanted the drug-eluting stent disagreed. He felt that the diseased state of the LAD would have risked immediate restenosis if a bare metal stent has been used.
In summary, there was much disagreement on this point. Nor was there a clear consensus as to the events that had led to the use of different types of stents. Clearly, there had been a lack of communication between the different interventionists and cardiologists.
4. Conclusions
In this era of rapidly advancing medical technology, it is well to remember that clinical medicine is largely an art and that the judgment of the skilled clinician is a necessary adjunct to technologies such as angiography.
Although the outcome was good for the patient reported here, the unexpected acute infarction in his chronically occluded and collateralized LAD might have been prevented if better trained nurses had not exacerbated the stress of hospitalization or if countermeasures for inflammation and vasoconstriction had been administered during stenting of the circumflex artery.
Given the many issues to be considered in selecting the type of stent to be implanted in a patient with a history of aspirin intolerance, good communication between different intervention teams and cardiologists could improve the standard of care.
5. Acknowledgements
The author thanks Terry N. Talkin, M.D., F.A.C.C. for helpful discussions and Indubala Vardhan, M.D., F.A.C.C. for assistance with electronic files.
REFERENCES
- G. M. Howard-Alpe, J. de Bono, L. Hudsmith, W. P. Orr, P. Foex and J. W. Sear, “Coronary Artery Stents and Non-Cardiac Surgery,” British Journal of Anaesthesia, Vol. 98, No. 5, 2007, pp. 560-574. doi:10.1093/bja/aem089
- G. A. Nuttall, M. J. Brown, J. W. Stombaugh, W. John, P. B. Michon, M. F. G. Hathaway, K. C. Lindeen, A. C. Hanson, D. R. Schroeder, R. Darrell, W. C. Oliver, D. R. Holmes and C. S. Rihal, “Time and Cardiac Risk of Surgery after Bare-Metal Stent Percutaneous Coronary Intervention,” Anesthesiology, Vol. 109, No. 4, 2008, pp. 588-595.
- J. A. Rabbitts, G. A. Nuttall, M. J. Brown, A. C. Hanson, W. C. Oliver, D. R. Holmes and R. Charanjit, “Cardiac Risk of Noncardiac Surgery after Percutaneous Coronary Intervention with Drug-Eluting Stents,” Anesthesiology, Vol. 109, No. 4, 2008, pp. 596-604.
- H. P. Brunner-La Rocca, C. Kaiser, A. Bernheim, M. J. Zellweger, R. Jeger, P. T. Buser, S. Osswld and M. Pfisterer, “Cost-Effectiveness of Drug-Eluting Stents in Patients at High or Low Risk of Major Cardiac Events in the Basel Stent KostenEffektivitäts Trial (BASKET): An 18- Month Analysis,” Lancet, Vol. 370, No. 9598, 2007, pp. 1552-1559. doi:10.1016/S0140-6736(07)61660-2
- I. Iakovou, T. Schmidt, E. Bonizzoni, L. Ge, G. M. Sangiorgi, G. Stankovic, F. Airoldi, A. Chieffo, M. Montorfano, M. Cartino, I. Michev, N. Corvaja, C. Briguori, U. Gerckens, E. Grube and A. Colombo, “Incidence, Predictors, and Outcome of Thrombosis after Successful Implantation of Drug-Eluting Stents,” Journal of American Medical Assocition, Vol. 293, No. 17, 2005, pp. 2126-2130. doi:10.1001/jama.293.17.2126
- M. N. Babaputte, L. Joseph, P. Bélisle, J. M. Brophy and M. J. Eisenberg, “A Hierarchical Bayesian Meta-Analysis of Randomised Clinical Trials of Drug-Eluting Stents,” Lancet, Vol. 364, No. 9434, 2004, pp. 583-591. doi:10.1016/S0140-6736(04)16850-5
- J. Schofer, M. Schlüter, A. H. Gershlick, W. Wijns, E. Garcia, E. Schampaert and G. Breithardt, “SirolimusEluting Stents for Treatment of Patients with Long Atherosclerotic Lesions in Small Coronary Arteries: Double-Blind, Randomised Controlled Trial (E-SIRIUS),” Lancet, Vol. 362, No. 9390, 2003, pp. 1093-1099. doi:10.1016/S0140-6736(03)14462-5
- H. Schühlen, M. Hadamitzky, H. Walter, K. Ulm and A. Schömig, “Major Benefit from Antiplatelet Therapy for Patients at High Risk for Adverse Cardiac Events after Coronary Palmaz-Schatz Stent Placement,” Circulation, Vol. 95, No. 8, 1997, pp. 2015-2021. doi:10.1161/01.CIR.95.8.2015
- G. Steffenino, B. Meier, L. Finci, V. Velebit, L. von Segesser, B. Faidutti and W. Rutishauser, “Acute Complications of Elective Coronary Angioplasty: A Review of 500 Consecutive Procedures,” British Heart Journal, Vol. 59, No. 2, 1988, pp.151-158. doi:10.1136/hrt.59.2.151
- W. S. Weintraub, C. L. Brown, H. A. Liberman, D. C. Morris, J. S. Douglas Jr. and S. B. King III, “Effect of Restenosis at One Previously Dilated Coronary Site on the Probability of Restenosis at Another Previously Dilated Coronary Site,” American Journal of Cardiology, Vol. 72, No. 15, 1993, pp. 1107-1113. doi:10.1016/0002-9149(93)90977-K
- G. L. Kaluza, J. Joseph, J. R. Lee, M. E. Raizner and A. E. Raizner, “Catastrophic Outcomes on Noncardiac Surgery Soon after Coronary Stenting,” Journal of the American College of Cardiology, Vol. 35, No. 5, 2000, pp. 1288-1294. doi:10.1016/S0735-1097(00)00521-0
- J. J. Badimon, A. F. Ortiz, B. Meyer, A. Mailhac, J. T. Fallon, E. Falk, L. Badimon, J. H. Chesebro and V. Fuster, “Different Response to Balloon Angioplasty of Carotid and Coronary Arteries: Effects on Acute Platelet Deposition and Intimal Thickening,” Atherosclerosis, Vol. 140, No. 2, 1998, pp. 307-314. doi:10.1016/S0021-9150(98)00134-8
- J. B. Foley, R. I. Brown and I. M. Penn, “Thrombosis and Restenosis after Stenting in Failed Angioplasty: Comparison with Elective Stenting,” American Heart Journal, Vol. 128, No. 1, 1994, pp. 12-20. doi:10.1016/0002-8703(94)90004-3
- C. Indolfi, F. Piscione, A. Rapacciuolo, G. Esposito, N. Esposito, R. Ceravolo, E. Di Lorenzo, A. Maione, M. Condorelli and M. Chiariello, “Coronary Artery Vasoconstriction after Successful Single Angioplasty of the Left Anterior Descending Artery,” American Heart Journal, Vol. 128, No. 5, 1994, pp. 858-864. doi:10.1016/0002-8703(94)90580-0
- V. P. Moles, F. Chappuis, P. Urban, F. De La Serna, A. K. Pande and B. Meier, “Aortic Dissection as Complication of Percutaneous Transluminal Coronary Angioplasty,” Catheterization and Cardiovascular Diagnosis, Vol. 26, No. 1, 1992, pp. 8-11. doi:10.1002/ccd.1810260103
- H. Nassar, Y. Hasin and M. S. Gotsman, “Cardiac Tamponade Following Coronary Arterial Reupture During Coronary Angioplasty,” Catheterization and Cardiovascular Diagnosis, Vol. 2, No. 3, 1991, pp. 177-179. doi:10.1002/ccd.1810230306
- R. H. Graf and M. S. Verani, “Left Main Coronary Artery Stenosis: A Possible Complication of Transluminal Coronary Angioplasty,” Catheterization and Cardiovascular Diagnosis, Vol. 10, No. 2, 1984, pp. 163-166. doi:10.1002/ccd.1810100207
- D. Kimbiris, A. S. Iskandrian, I. Goel, C. E. Bemis, L. Gehl, J. Owens and B. L. Segal, “Transluminal Coronary Angioplasty Complicated by Coronary Artery Perforation,” Catheterization and Cardiovascular Diagnosis, Vol. 8, No. 5, 1982, pp. 481-487.doi:10.1002/ccd.1810080507
- E. Quattromani, A. Aldeen, W. Mosloey II and D. Courtney, “A Case Series and Review of Takotsubo Cardiomyopathy: Does Stress Really Cause the Stress Cardiomyopathy? Flying-Machine,” International Journal of Clinical Medicine, Vol. 2, No. 1, 2011, pp. 28-34. doi:10.4236/ijcm.2011.21007
- P. M. S. Carvalho, J. H. Lima, J. B. Cunha, P. G. D. Dias, J. G. D. Vieira and J. M. N. Costa, “Tako-Tsubo Cardiomyopathy—The Role of Physical and Emotional Stressors: Two Case Reports,” International Journal of Clinical Medicine, Vol. 3, No. 2, 2012, pp. 145-150. doi:10.4236/ijcm.2012.32029
- A. Rosengren, S. Hawken, S. Ôunpuu, K. Sliwa, M. Zubaid, W. A. Almahmeed, K. N. Blackett, C. SitthiAmorn, H. Sato and S. Yusuf, “Association of Psychological Risk Factors with Risk of Acute Myocradial Infarction in 11,119 Cases and 13,648 Controls from 52 Countries (The INTERHEART Study): Case-Control Study,” Lancet, Vol. 364, No. 9438, 2004, pp. 953-962. doi:10.1016/S0140-6736(04)17019-0
- W. Jiang, M. Babyak, D. S. Krantz, R. A. Waugh, R. E. Coleman, M. M. Hanson, D. J. Frid, S. McNulty, J. J. Morris, C. M. O’Connor and J. A. Blumenthal, “Mental Stress—Induced Myocardial Ischemia and Cardiac Events,” Journal of American Medical Association, Vol. 275, No. 21, 1996, pp. 1651-1656. doi:10.1001/jama.275.21.1651
- M. A. Mittleman, M. Maclure, J. B. Sherwood, R. P. Mulry, G. H. Tofler, S. C. Jacobs, R. Friedman, H. Benson and J. E. Muller, “Triggering of Acute Myocardial Infarction Onset by Episodes of Anger,” Circulation, Vol. 92, No. 7, 1995, pp. 1720-1725. doi:10.1161/01.CIR.92.7.1720
- N. Frasure-Smith, F. Lespérance and M. Talajic, “The Impact of Negative Emotions on Prognosis Following Myocardial Infarction: Is it More Than Depression?” Health Psychology, Vol. 14, No. 5, 1995, pp. 388-398. doi:10.1037/0278-6133.14.5.388

