Open Journal of Pediatrics
Vol. 2 No. 1 (2012) , Article ID: 18007 , 6 pages DOI:10.4236/ojped.2012.21011
Nighttime feeding in Turkish children and its association with anemia
![]()
1Department of Pediatrics, Okmeydanı Training and Research Hospital, Istanbul, Turkey
2Family Health Center of Ilgaz, Çankırı, Turkey
3Department of Pediatrics, Göztepe Research and Training Hospital, Istanbul, Turkey
4Hematology/Oncology, Carman and Ann Adams Children’s Hospital of Michigan, Wayne State University, Detroit, USA
Email: *bulentozgonenel@yahoo.com
Received 6 September 2011; revised 20 December 2011; accepted 10 January 2012
Keywords: Survey; Nighttime Feeding; Pediatric Sleep Disorder; Anemia; Iron Deficiency
ABSTRACT
Background: Children who continue to wake up at night to be fed after 6 months of age are called trained nighttime feeders. Nighttime feeding may be associated with dental and medical complications, in addition to causing sleep deprivation in children and parents, as well as with iron-poor nutrition. Methods: We surveyed 614 Turkish children aged 6 months to 5 years from three centers (2 urban and 1 rural) to determine the prevalence of nighttime feeding. We also sought to determine factors associated with continuation of nighttime feedings after 6 months of age. Results: Fifty percent of the participants were nighttime feeders. Nighttime feedings were given once, twice, and three times or more to 19.9%, 15.6%, and 14.5% of the participants, respectively. The rural population had a higher rate of nighttime feeding (57.0% rural vs 46.6% urban, p = 0.016). 168 urban children (median age 25 months) had blood count data. Fifty percent of these children were given nighttime feedings: 19.6% once, 17.9% twice, and 12.5% three times or more. Nighttime meals were breastfeeding in 51.2%, cow’s milk by bottle in 33.3%, and other in 15.5%. Mean hemoglobin level of nighttime feeders was significantly lower: 11.3 ± 1.3 g/dL vs 12.2 ± 1.0 g/dL in non-nighttime feeders (p < 0.001), even dropping to 10.8 ± 1.4 g/dL in those that were fed 3 times or more at night (p < 0.001). 31.0% of nighttime-feeders were anemic compared to 17.9% in those that did not receive nighttime feedings (p = 0.048). We also noted that intense nighttime feeding was associated with lower MCV (p < 0.001) and lower ferritin levels (p < 0.001). Conclusions: Nighttime feeding is prevalent among Turkish children, especially among the rural population. Nighttime feeding was also noted to be associated with anemia in this study. Nighttime feeding should be screened for and treated in children after 6 months of age.
1. INTRODUCTION
Although babies require nighttime meals only up to 4 months of age, some children continue to wake up to be fed even after this age. Such children are called trained nighttime feeders as they have been conditioned to interrupt their sleep cycle for nocturnal feedings [1-3]. The child typically wakes up crying, and cannot return to sleep unless given a nighttime meal. Nighttime feedings are not physiologic after 6 months of age, and the nighttime meals do not reflect hunger [2,3]. Nighttime feeding after 6 months is very troublesome for the caregivers, and causes sleep deprivation both in the child and the parents. Consequently, habitual nighttime feeding may be accompanied by frequent daytime naps. Social-cultural and parental factors may influence the way caregivers respond to nighttime arousals [2-4], and weaning off the nighttime feeding may be delayed until as late as school age in some cases.
Nighttime feeding has been associated with dental and medical complications, such as infant nursing bottle caries [5-9], middle ear problems [10], wheezing [11], and of course, sleep deprivation. Nighttime feeding may cause stress and sleep deprivation in parents as well [12]. Nighttime feeding of infants and children after 6 months of age may also accompany exclusive breastfeeding [6] or excessive cow’s milk intake by bottle [13]. We suspect that nighttime feeding could be associated with iron deficiency anemia in children by promoting iron-deficient nutrition.
In this study, we surveyed Turkish children older than 6 months of age to determine the rate of nighttime feeding and underlying etiologic factors. We also reviewed medical records to seek evidence of association between nighttime feeding and anemia in Turkish children of urban and rural background.
2. METHODS
2.1. Study Centers
Children were recruited to the study from both rural and urban outpatient well-child clinics of Turkey. The rural component of the study was conducted at the Family Health Center of Ilgaz, Çankırı between May and October 2010. Ilgaz is a small town in north-western Turkey with a 2010 population of close to 14,000 [14]. The urban component of the study was conducted at the ambulatory pediatric clinics of Okmeydanı and Göztepe Training and Research Hospitals, Istanbul, between July and October 2010.
Children between the ages of 6 months to 5 years presenting to the above-mentioned centers were enrolled in the study after verbal consent was obtained. Demographic information (sex and age in months) was noted, and parents were surveyed with a questionnaire on nighttime feeding. Age was grouped in 5 ranks: 6 - 11 months (infants); 12 - 23 months (1-year-old group); 24 - 35 months (2-year-old group); 36 - 47 months (3-year-old group); and 48 - 59 months (4-year-old group).
2.2. Survey
The questionnaires in both settings inquired whether the child was fed at night and if yes how frequently; frequency of daytime naps. The urban questionnaires also inquired the type of milk consumed during nighttime feedings. The rural questionnaires included questions about maternal level of education and maternal employment. All frequencies were worded as either none, once, twice, or three times or more.
2.3. Laboratory Analysis
When available from the medical records for that particular visit, blood count results were reviewed for hemoglobin and mean corpuscular volume (MCV) values, and serum ferritin levels were recorded. Anemia was defined as a hemoglobin level of <10.5 g/dL for age 6 - 23 months, and <11.5 g/dL for age 24 - 60 months.
2.4. Statistical Analysis
The findings were analyzed using the SPSS (Statistical Package for the Social Sciences) software, PASW Statistics 18.0. Significance was set at p < 0.05.
3. RESULTS
3.1. Demographic Features Associated with Nighttime Feeding
614 children (52.3% male) were recruited to the study from both urban and rural settings. Of these, 414 were recruited from urban locations, and 200 were recruited from the rural area. Most of the children were either in the 1-year-old group (31.9%) or in the 2-year-old group (21.7%). Urban and rural patients had a similar sex distribution (p = 0.140 by chi-square); however, the rural population had a younger age distribution (p = 0.016 by chi-square). Table 1 summarizes the demographic characteristics of the participants.
We had additional demographic information on the mothers of rurally recruited children. Their educational level was as follows: 1.5% illiterate, 8.5% primary school dropouts, 63.0% graduates of primary school (up to the 8th grade) only, 22.5% high-school graduate, and 4.5% graduates of university or similar higher schooling. 93.0% of the rural mothers were homemakers, 1.0% worked part-time, and 6.0% had a full-time job.
Exactly 50.0% of the participants were nighttime feeders. Nighttime meals were given once, twice, and three times or more to 19.9%, 15.6%, and 14.5% of the participants, respectively.
3.2. Factors Associated with Nighttime Feeding
The rural population had a significantly higher rate of nighttime feeding (57.0% rural vs 46.6% urban, p = 0.016 by chi-square). Nighttime feeding intensity per night was similarly higher in the rural population (p = 0.004 by chi-square). Table 2 demonstrates this relationship.
Nighttime feeding was not correlated with gender (p = 0.099 by chi-square); however, as expected, it was significantly correlated with age (p < 0.001 by chi-square).
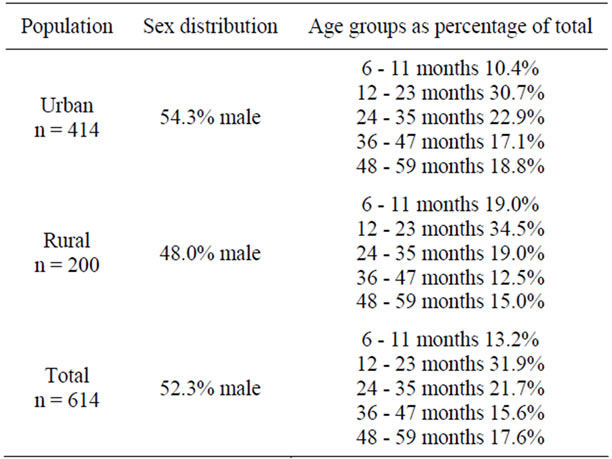
Table 1. Demographic characteristics of study participants.
Both the frequency and the intensity of nighttime feeding were heavier among younger-aged children. Whereas as much as 43.2% of 6 - 11-month old infants and 23.5% of 1-year-old group received nighttime feeding three times or more; only 3% of the 2-year-old group, none of the 3-year-old group, and 3.7% of the 4-year-old ones were still receiving nighttime feeding at this intensity. Table 3 gives the distribution of nighttime feeding in age groups and Figure 1 depicts the relationship between age and nighttime feeding intensity.
3.3. Nighttime Feeding and Its Association with Daytime Naps
Nighttime feeding intensity was correlated with daytime nap intensity: the more daytime naps the child took, the more frequently was he fed at night. (Spearman’s rho correlation 0.547, p < 0.001). Figure 2 demonstrates this significant relationship. However, when examined within age groups, this significant association was preserved only in infants aged 6 - 11 months (Spearman’s rho correlation 0.235, p = 0.035) and the 1-year-old ones (Spearman’s rho correlation 0.280, p < 0.001). Table 4 depicts the relationship between age and number of daytime naps.
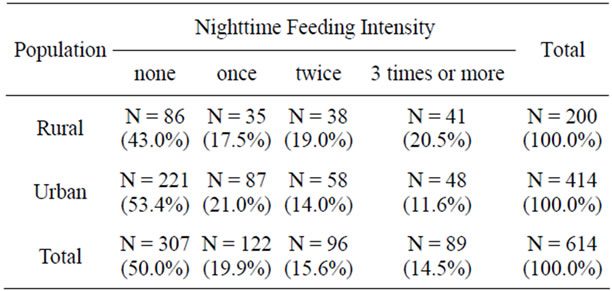
Table 2. Nighttime feeding comparison between urban and rural populations.
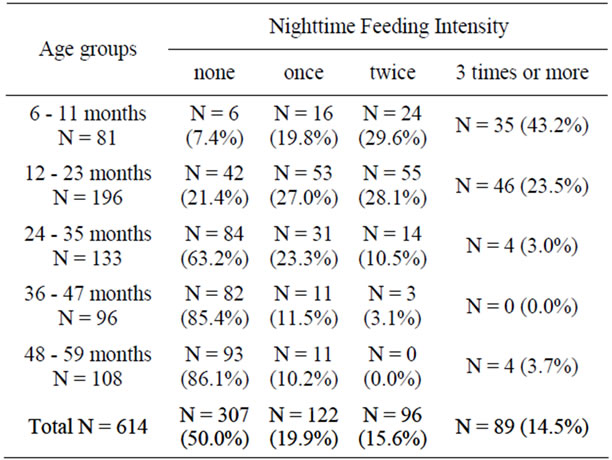
Table 3. Nighttime feeding intensity according to age groups. Percentages in parentheses reflect the proportion of the nighttime feeding intensity within that age group.
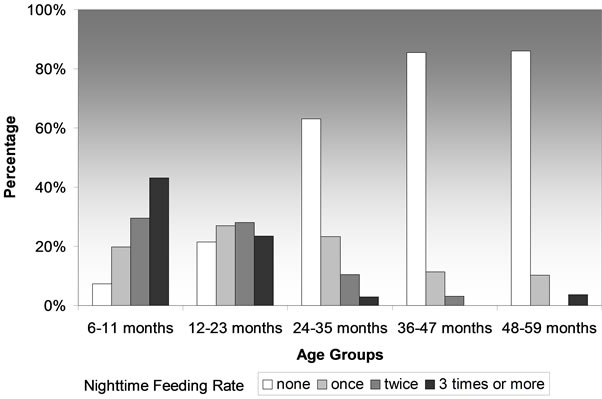
Figure 1. Relationship between age and nighttime feeding.
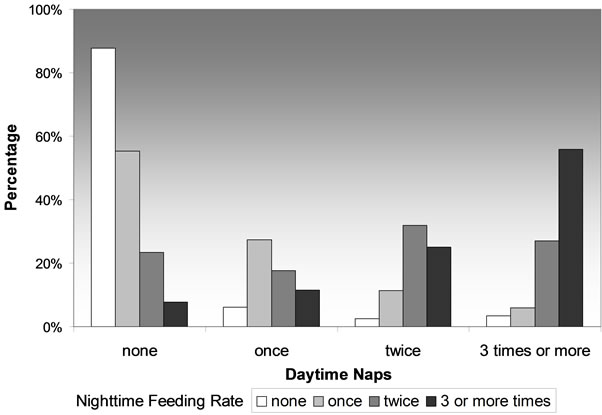
Figure 2. Relationship between daytime naps and nighttime feeding intensity.
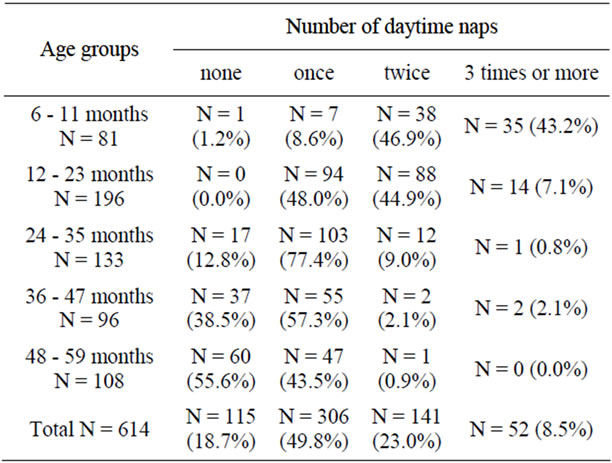
Table 4. Relationship between age and number of daytime naps in the age groups.
3.4. Nighttime Feeding and Its Association with Anemia
168 children from the urban population had blood count data. Median age was 25 months (mean 28.3 ± 14.8 months) for this group. Fifty percent of these children were given nighttime feedings: 19.6% once, 17.9% twice, and 12.5% three times or more. Nighttime meals were breastfeeding in 51.2%, cow milk by bottle in 33.3%, and other (formula milk, yogurt, milk pudding, cow’s milk mixed with other foods) in 15.5%. As in the general population above, nighttime feedings occurred more frequently in younger children (Spearman’s rho correlation: –0.657, p < 0.001).
Mean hemoglobin level of nighttime feeders was significantly lower: 11.3 ± 1.3 g/dL versus 12.2 ± 1.0 g/dL in non-nighttime feeders (Spearman’s rho correlation: –0.398, p < 0.001). As nighttime feeding intensified, hemoglobin levels dropped even lower, reaching a mean of 10.8 ± 1.4 g/dL in those that were fed 3 times or more at night (p < 0.001 by ANOVA), as shown in Table 5. When multiple comparisons were run, it was noted that the hemoglobin levels of only those fed twice per night and those fed 3 times or more were significantly lower compared to non-nighttime feeders. This relationship is illustrated as a box-plot graph in Figure 3.
31.0% of nighttime-feeders were anemic compared to 17.9% in those that did not receive nighttime feedings (p = 0.048 by chi-square). Anemia became more frequent with increasing intensity of nighttime feedings: 21.2% in those fed once at night, 33.3% in those fed twice, and 42.9% in those fed 3 times or more (p = 0.012 by Spearman’s rho correlation).
Because hemoglobin levels were lower in younger children, we examined the relationship between nighttime feeding and presence of anemia in different age groups. With such stratification, nighttime feeding was significantly associated with anemia only in the 2-yearold ones (p = 0.024 by Fisher’s exact test).
The mean MCV was 80.3 ± 4.6 fL in non-nighttime feeders, as compared to 77.9 ± 6.3, 73.5 ± 7.7, and 73.9 ± 8.2 in those who were given nighttime feeding once, twice, and three times or more per night, respectively (p < 0.001 by ANOVA). In multiple comparisons, only those who were fed twice or three times or more had significantly lower MCV compared to non-nighttime feeders.
Serum ferritin results were available for 45 of the children that had blood count data. Children who had ferritin data had a similar mean hemoglobin level as those who
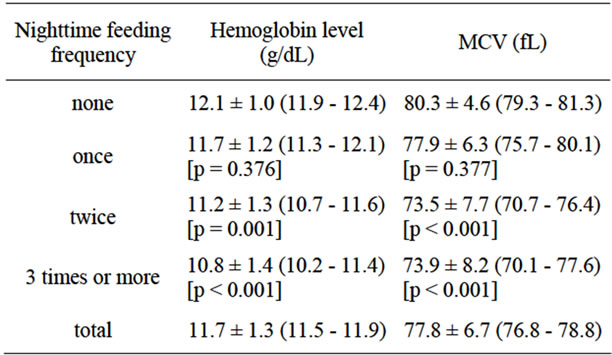
Table 5. Mean hemoglobin and MCV values in nighttime feeding. Values are given as mean ± standard deviation (95% confidence interval). Significance is given in brackets when compared to non-nighttime feeders.
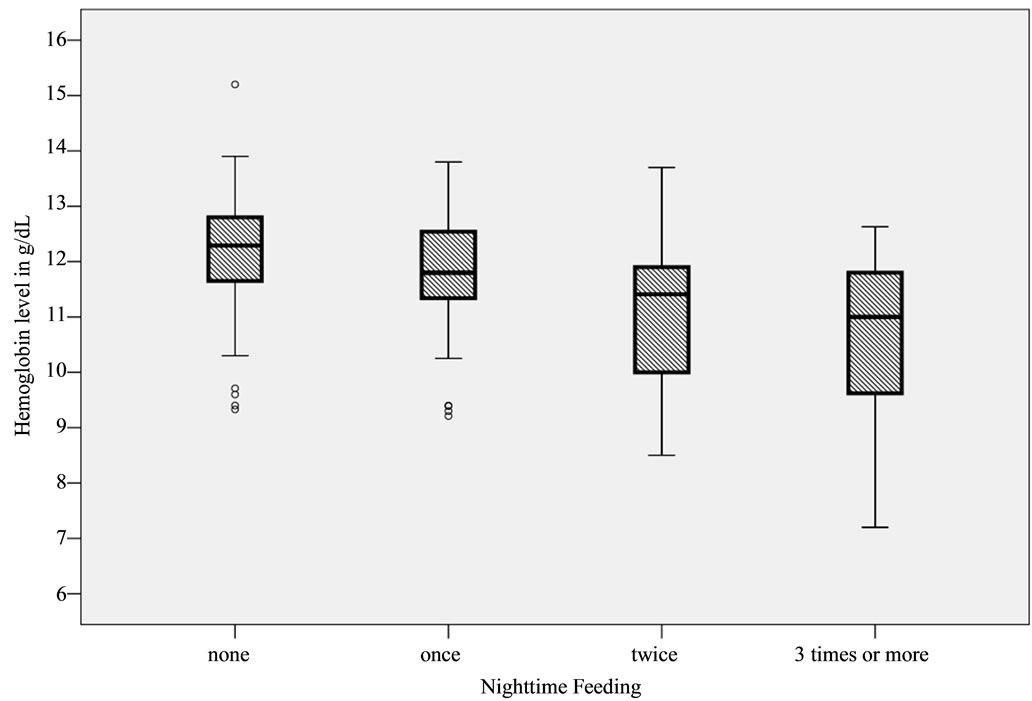
Figure 3. Relationship between nighttime feeding intensity and hemoglobin levels.
did not (p = 0.096 by t-test). The mean serum ferritin level was 22.5 ± 17.6 ng/mL in children that were not fed at night (n = 25), as compared to 15.2 ± 8.7, 13.2 ± 6.9, and 6.5 ± 4.2 ng/mL for those children who were given nighttime feeding once (n = 5), twice (n = 9), and three times or more (n = 6) per night, respectively (p = 0.014 by Kruskal-Wallis). Serum ferritin level was inversely correlated with the intensity of nighttime feeding (Spearman’s rho correlation –0.469, p = 0.001). Iron deficiency, defined as ferritin levels below 10 ng/mL, was present in 37.8% (n = 17) of the 45 children that had ferritin data. Iron deficiency was present in 55% of nighttime feeders compared to 24% of non-nighttime feeders (p < 0.001 by chi-square).
3.5. Comparison of Nighttime Breastfeeding with Cow’s Milk-Feeding
We also compared breastfeeding at night and cow’s milk feeding at night. Of the 21 children that received nighttime feeding three or more times, 90.5% (n = 19) were breastfed, 9.5% (n = 2) received other kind of feeding at night, and none received cow’s milk (p < 0.001 by chisquare). Breastfed children were younger (p < 0.001 by chi-square) than other groups, and the oldest child that was breastfed was 30 months old. Hemoglobin levels and serum ferritin levels were significantly lower in breastfed children compared to cow’s milk-fed children. These findings are summarized in Table 6.
4. DISCUSSION
Trained nighttime feeding in children has not been extensively investigated, and evidence-based information is lacking in the medical literature. Bedtime problems and night waking are reported to exist in 20% - 25% of children aged 1 - 5 years of age [15]. In a report form Iran, where 504 children aged 1 - 3 years were screened for early childhood caries, 85% of the children were noted to receive nighttime feedings [6]. Our results show that a significant proportion of Turkish children aged 6 months to 5 years (50%) received nighttime feedings.
The rural population had a higher rate of nighttime feeding compared to the urban population. This could be explained partly by traditional child-rearing practices in the rural setting that might have fostered nighttime feeding. Alternatively, factors related to urban living, such as the morning commute, might have fostered earlier weaning from nighttime feeding to prevent sleep deprivation of parents. Although we cannot compare the rural and urban populations due to lack of urban data, it is interesting to note that only 27% of the mothers from the rural setting were graduates of high-school or higher level of education, and only 7.0% had a part-time or fulltime job.
Nighttime feeding was also associated with younger age, which is not surprising as many of these children are expected to be weaned off nighttime feeding between the ages of 1 - 3 years old. What is concerning is that a significant fraction of children, that is 14.6% and 13.9%, still continue the nighttime feeding into their three or four years, respectively.
The number of daytime naps was associated with the number of nighttime feedings in our study. Daytime naps, of course, are part of the physiological sleep in younger children, and typically infants between the ages of 6 months to 1 year take two daytime naps per day and toddlers 1 - 3 years old take one daytime nap per day [16]. In our study many children continued to take daytime naps into the fourth year; however, children older than 3 years rarely took daytime naps more than once. Daytime naps more than twice per day after 6 months closely parallel intense nighttime feedings, and may indicate a compensatory mechanism to compensate for nocturnal sleep deprivation. This may be important in obtaining history from parents: number of daytime naps should be questioned at well-child visits, and those who take 3 or more naps should be questioned about nighttime feeding. There is no evidence that preventing a child from taking daytime naps (and thus foster nighttime sleepiness), would facilitate weaning off nighttime feedings, and is not recommended [17].
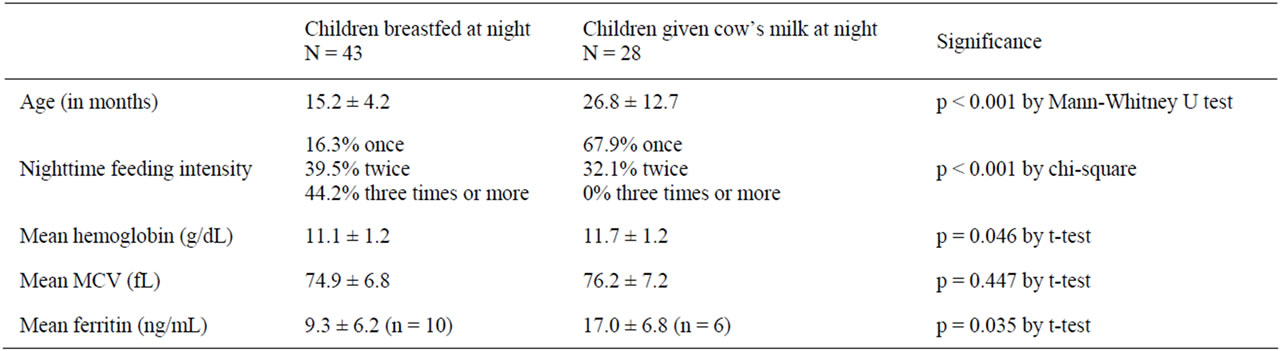
Table 6. Age, nighttime feeding intensity, and hematologic values compared between children breastfed at night versus those fed cow’s milk at night.
In our study, intense nighttime feeding (twice or more) was associated with lower hemoglobin levels, lower MCV values, and anemia, defined as a hemoglobin level of <10.5 g/dL for age 6 - 23 months, and <11.5 g/dL for age 24 - 60 months, in children 6 months to 5 years. Iron-poor nutrition, with its consequent iron deficiency, could account for this anemia. Serum ferritin levels, available from a smaller number of children, tended to be low in those given nighttime feedings three times or more.
It was mostly the breastfed children, who received feeding three or more times per night, whereas children fed cow’s milk received nighttime feeding at a less intense rate. Accordingly, children who received breastfeeding at night had lower hemoglobin and ferritin levels. More frequent nighttime feeding and the younger age of breastfed children could account for these results, and breastfeeding itself should not be blamed. In fact, American Academy of Pediatrics recommends continuing breastfeeding into the third year; however, breastfed infants should be introduced to complementary feedings or receive iron supplementation after 6 months of age [18]. We speculate that nighttime feeding interferes with complementary feedings by promoting exclusive breastfeeding, and thus sets the stage for iron deficiency anemia.
5. CONCLUSION
Our pilot survey study unequivocally demonstrates that trained nighttime feeding is prevalent among Turkish children aged 6 months to 5 years, possibly constituting a public health problem. Nighttime feeding is associated with anemia in this age group: it could merely be a marker for the iron-deficient nutrition; alternatively, it could be one of the causative risk factors for nutritional iron deficiency anemia because it fosters iron-poor nutrition. Prospective studies are needed to test this hypothesis. Because of its dental and medical complications, in addition to depriving both children and their caregivers of precious sleep, nighttime feeding after 6 months of age should be discouraged. Pediatricians should screen for nighttime feeding in children older than 6 months, and provide anticipatory guidance and counseling on weaning to parents.
REFERENCES
- Howard, B.J. and Wong, J. (2001) Sleep disorders. Pediatrics in Review, 22, 327-342. doi:10.1542/pir.22-10-327
- Mindell, J.A. and Owens, J.A. (2010) A clinical guide to pediatric sleep, diagnosis and management of sleep problems. 2nd Edition, Lippincott Williams & Wilkins, Philadelphia.
- Thiedke, C.C. (2001) Sleep disorders and sleep problems in childhood. American Family Physician, 63, 277-284.
- Sadeh, A., Tikotzky, L. and Scher, A. (2010) Parenting and infant sleep. Sleep Medicine Reviews, 14, 89-96. doi:10.1016/j.smrv.2009.05.003
- Menghini, G., Steiner, M. and Imfeld, T. (2008) Early childhood caries-facts and prevention. Therapeutische Umschau, 65, 75-82. doi:10.1024/0040-5930.65.2.75
- Mohebbi, S.Z., Virtanen, J.I., Vahid-Golpayegani, M. and Vehkalahti, M.M. (2008) Feeding habits as determinants of early childhood caries in a population where prolonged breastfeeding is the norm. Community Dentistry and Oral Epidemiology, 36, 363-369. doi:10.1111/j.1600-0528.2007.00408.x
- Slabsinskiene, E., Milciuviene, S., Narbutaite, J., et al. (2010) Severe early childhood caries and behavioral risk factors among 3-year-old children in Lithuania. Medicina (Kaunas), 46, 135-141.
- Van Everdingen, T., Eijkman, M.A. and Hoogstraten, J. (1996) Parents and nursing-bottle caries. ASDC Journal of Dentistry for Children, 63, 271-274.
- Zhong, Z.Q. (2009) The relationship between the infant nursing bottle caries and the feeding patterns, oral health behavior and parents’ oral health information. Shanghai Journal of Stomatology, 18, 588-591.
- Tully, S.B., Bar-Haim, Y. and Bradley, R.L. (1995) Abnormal tympanography after supine bottle feeding. Journal of Pediatric, 126, S105-S111.
- Celedon, J.C., Litonjua, A.A., Ryan, L., Weiss, S.T. and Gold, D.R. (2002) Bottle feeding in the bed or crib before sleep time and wheezing in early childhood. Pediatrics, 110, e77. doi:10.1542/peds.110.6.e77
- Wake, M., Morton-Allen, E., Poulakis, Z., Hiscock, H., Gallagher, S. and Oberklaid, F. (2006) Prevalence, stability, and outcomes of cry-fuss and sleep problems in the first 2 years of life: Prospective community-based study. Pediatrics, 117, 836-842. doi:10.1542/peds.2005-0775
- Brotanek, J.M., Schroer, D., Valentyn, L., Tomany-Korman, S. and Flores, G. (2009) Reasons for prolonged bottle-feeding and iron deficiency among Mexican-American toddlers: An ethnographic study. Academy of Pediatrics, 9, 17-25. doi:10.1016/j.acap.2008.10.005
- Demir, K. (2011) Ilgaz nüfus müdürlüğü.
- Mindell, J.A. (1999) Empirically supported treatments in pediatric psychology: Bedtime refusal and night wakings in young children. Journal of Pediatric Psychology, 24, 465-481. doi:10.1093/jpepsy/24.6.465
- Ferber, R. (1985) Solve your child’s sleep problems. Simon & Schuster, New York.
- Mindell, J.A. (2005) Sleeping through the night: How infants, toddlers, and their parents can a get a good night’s sleep. Harper Paperbacks, New York.
- Gartner, L.M., Morton, J., Lawrence, R.A., et al. (2005) Breastfeeding and the use of human milk. Pediatrics, 115, 496-506. doi:10.1542/peds.2004-2491
NOTES
*Corresponding author.

