Journal of Cosmetics, Dermatological Sciences and Applications
Vol.2 No.4(2012), Article ID:26156,6 pages DOI:10.4236/jcdsa.2012.24055
Direct Melanocytes Transplant from Normal Donor Area into Vitiliginous Recipient Area by Dermabrasion Technique*
![]()
1The Scientific Council of Dermatology & Venereology, Iraqi Board for Medical Specializations, Baghdad, Iraq; 2Department of Dermatology & Venereology, College of Medicine, University of Baghdad, Baghdad, Iraq; 3Department of Dermatology & Venereology, Baghdad Teaching Hospita, Baghdad, Iraq.
Email: #ksharquie@ymail.com, adilnoaimi@yahoo.com, hana_almudaris@yahoo.com
Received July 5th, 2012; accepted August 7th, 2012; accepted August 18th, 2012
Keywords: Vitiligo; Melanocytes Transplant; Dermabrasion; Direct Transfer
ABSTRACT
Background: Vitiligo is an autoimmune pigmentory disorder, that affects all age group that is treated by many medical treatments but some of them might need surgical therapy. Objective: To evaluate the dermabrasion technique in the treatment of vitiligo by direct transfer of melanocytes from the dermabraded normal donor area to the vitiliginous recipient area. Patients and Methods: This is a case interventional study was done in Department of Dermatology/Baghdad Teaching Hospital from February 2011-March 2012. Nine Patients with vitiligo were enrolled in this study with different clinical types of vitiligo including 5 segmental, 2 generalized and 2 localized. The donor and recipient areas were anesthetized at the same time with xylocain alone. Dermabrasion of recipient area was done first by manual abrader and left for few minutes until the oozing was stopped. Then the donor area was similarly dermabraded and the dermabraded tissue including the epidermis and superficial epidermis was immediately transferred into the recipient area and dressing was applied. Removal of the dressing was done after 10 - 14 days from the operative time. Follow up was done every 2 weeks in the first month then monthly for six months to record the result of implantation and repigmentation. Results: The re-pigmentation started one month after the operation as small macules and this increased gradually over time: the mean rate of re-pigmentation was 13% at 2 months, 27.8% at 4 months and 36.78% at 6 months. In addition, sun light exposure was applied to enhance re-pigmentation. The pigmentation was diffuse and not follicular in shape. Conclusion: Direct transfer of melanocytes from normal donor area into vitiliginous recipient area by dermabrasion technique was easy, rapid and non-costly and gave 36.78% mean rate of pigmentation at 6 months follow up and without complications.
1. Introduction
Vitiligo is a common autoimmune inflammatory disease where there is absence, deficiency or dysfunction of melanocytes [1-4]. There are many standard therapies for vitiligo like PUVA [5], PUVA Sole [6], Narrow Band UVB [7], 5% Tincture iodine solution [6,8] and lactic acid [9,10]. The response of therapy depends on severity of disease, location of the illness and time factor. Some cases of vitiligo like segmental or localized vitiligo that do not respond to medical types, surgical therapy is indicated.
There are many surgical grafting procedures used in vitiligo but the commonly practiced nowadays are autologous melanocytes transplants that have been used to treat vitiligo patches by using tissue graft, like punch minigraft [11-15], suction blister epidermal grafting [13], and split thickness grafting [15-17] and cellular grafting like transplantation of autologous epidermal cell suspension [18-23] (non-cultured melanocytes grafting and transplantation of cultured autologous melanocytes). The old technique using minigrafting is usually associated with many problems like poor spread of the grafted melanocytes to the surrounding area, cobble stoning and needs punching grafts. While the other techniques are expensive, need sophisticated laboratories and personals [11- 17].
The aim of present work is to look for rapid, time sparing surgical procedure of melanocytes grafting by so called direct melanocytes transplant by dermabrasion technique from dermabraded normal donor area into dermabraded vitiliginous recipient area.
2. Patients and Methods
Nine patients with vitiligo were included in this case interventional study, 3 males and 6 females, their ages range from 8 - 38 years with a mean ± SD of 20.22 ± 10.29 years All clinical types of vitiligo including some areas of generalized, localized and segmental were treated. The number of vitiligo patches varied between patients and the total number of treated patches were 15 (Table 1).
2.1. Inclusion Criteria
Localized vitiligo, localized vitiliginous areas from generalized vitiligo and segmental vitiligo were included. Activity of the disease was recorded for each patient to fix the duration of stability of the disease and the patients were divided into two groups stable vitiligo when there was no activity of the disease for more than 6 month before grafting and the second group when the stability of the vitiligo was ranged from 2 - 6 months only before grafting (Table 1).
2.2. Exclusion Criteria
Systemic diseases like hematological problems or drugs that prevent clotting, immune-compromised patient, diabetes mellitus and other debilitating diseases were excluded. Also all patients with active vitiligo at the time of grafting were excluded.
All therapies for vitiligo were stopped at least one month prior to the operation.
The nature and target of this study were explained for each patient. Formal consent was taken from each patient before starting the operation, after full explanation about the nature of the disease, course, the procedure of treatment, follow up, prognosis and the need for pre and post treatment photographs. Also, the ethical approval was given by the scientific committee of the Scientific Council of Dermatology & Venereology-Iraqi Board for Medical Specializations.
All patients were photographed by a digital camera as a baseline and then every two weeks, in the same place with fixed illumination and distance by using a digital camera (Canon: power shoot G12, HS system, 10.0 mega pixels, high-sensitivity, HD movie).
2.3. Technique of Transplant
Xylocain as local anesthesia was used to anesthetize both the vitiliginous recipient area and the normal donor skin at the same time. Sterilized manual dermabrader of different sizes: 6 mm, 10 mm, 16 mm (Aisco Company, Germany) (Figure 1) was used to do superficial dermabrasion of the recipient area, and then was covered with normal saline soaked gauze to stop bleeding. Similar dermabrasion was done for the donor area to remove the epidermis and papillary dermis and directly transferred into the recipient area (Figure 2).
After finishing the transplantation, hypo-allergic semiocclusion plaster (Betafix, Betasam, Turkey) was put as dressing on the recipient and donor areas. Systemic antibiotics were given for ten days.
Dressing was removed 10 - 14 days after the operation. The patient was advised to expose the recipient area to sun light for at least 15 minutes a day for everyday without using any topical therapy. Follow up was done every two weeks for the first month and monthly for 6 months to report the rate of re-pigmentation in the recipient area. Also follow up was done for donor area similar to recipient area watching any complications like koebners phenomenon, scar and keloid formation.
3. Results
After about 2 weeks from the time of operation only redness were noticed. Then the repigmentation at the
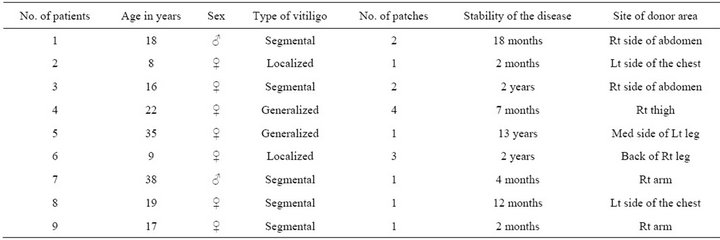
Table 1. The types of vitiligo, stability of the disease, and the site of donor areas.

Figure 1. Showing the manual dermabraders of different sizes.

Figure 2. Melanocytes transfer by dermabrasion technique showing dermabraded donor area.
grafted area was started one month after the time of operation. The pigmentation was macular and sometimes follicular type (Figure 3). At 2 months follow up the rate of pigmentation was increased and surface area was reduced, and the reduction ranged from 3% - 30% with a mean 13%, while at 4 months follow up, the rate of pigmentation was ranged from 7% - 60% with a mean 27.8%. The pigmentation increased gradually to become at 6 month follow up a range from 15% - 70% with a mean 36.33% (Table 2). The pigmentation in six months follow up was diffuse uniform, figurate in shape but not follicular (Figure 4).
Regarding the activity of the disease, also the rate of pigmentation was much less and less rapid in a patient with stable vitiligo for 2 - 6 months compared to stable vitiligo more than 6 months.
In 2 cases while the pigmentation was going on very well in the grafted area there was new vitiliginous areas appeared elsewhere.
Also in 2 patients who had white hairs in the grafted donor area like beard or abdomen, these white hairs changed into pigmented hair at the grafted area.
 (a)
(a) (b)
(b) (c)
(c) (d)
(d)
Figure 3. (a) Vitiligo patch on the right leg of 22 years old female patient preoperative; (b) The same patient at time of dermabrasion; (c) The same patient showing repigmentation after 1 month; (d) The same patient showing 80% repigmentation after 6 months of operation.
In 2 patients the repigmentation and depigmentation process was going on at same time in the same patch.
Regarding the donor area repigmentation was noticed after few weeks. No complications were noticed apart from 6 patients who had hyperpigmentation that went to normal over time.
4. Discussion
Although vitiligo is a common autoimmune pigmentory disorder, still there are many patient do not respond to standard medical therapies especially patient with segmental vitiligo. There are many new satisfactory surgical grafting procedures that have been used for treating vitiligo which is resistant to medical therapies, each one has its merits and disadvantages like culturing and non culturing technique melanocytes transplantation of autologous epidermal cell suspension [18-23], These procedures although effective to induce repigmentation in vitiliginous area but it is time consuming, needs sophisticated laboratories and personnel and they are expensive operations [11-23].
The present work is a new technique, easy to perform; non-expensive procedure that could be carried out in outpatients bases taking very short time. By this new procedure we did a direct transfer of melanocytes from normal donor area into vitiliginous recipient area. The pigmentation appeared at one month and gradually increased over time: the mean rate of repigmentation after two months was 13% while was 27.8% after four months
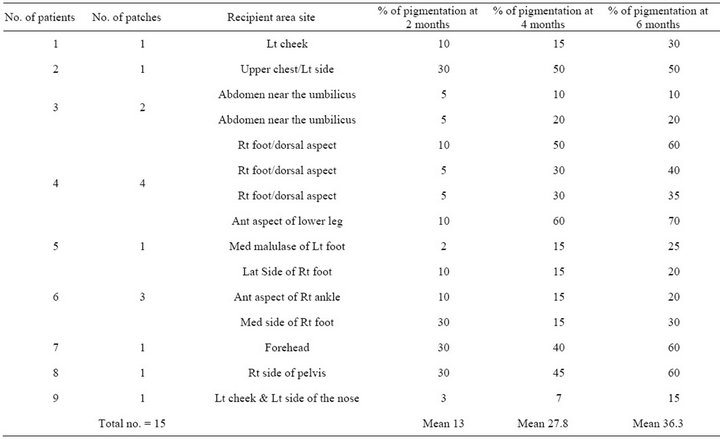
Table 2. The number of patches, the site and rate of pigmentation of the recipient areas after dermabrasion.
 (a)
(a) (b)
(b)
Figure 4. (a) 22 years old female patient with vitiligo patches on her right foot; (b) The same patient showing figurate repigmentation 6 months following dermabrasion.
and 36.78% after six months.
All the successful surgical procedures for treatment of vitiligo like split skin graft [15-17], suction blister epidermal grafting [13], cultured and non-cultured melanocytes [18-23] have transported the normal melanocytes from normal skin into dermabraded vitiliginous recipient areas. The present study was comparable to these surgical procedures where melanocytes in the dermabraded tissues where transferred from normal donor skin into dermabraded recipient area.
The present work showed also that transplant of melanocytes from normal donor area into non-hairy recipient area like dorsum of foot induced successful repigmentation (Figure 4). Also, all re-pigmentation in our patients was diffuse uniform but not follicular and this goes parallel with way of spread of the dermabraded tissue from donor skin into recipient area. Also in two our patients, the white hairs in recipient areas changed into pigmented hair after melanocytes transplant. These observations are in favor that residual hair follicles melanocytes are not the source of re-pigmentation.
In addition, there are some controversies regarding the dermabrasion of the vitiliginous skin was enough to induce repigmentation as there are some studies showed that dermabrasion had failed to induce re-pigmentation [24-27].
Hence, we can conclude that residual melanocytes in the hair follicles in vitiligo skin might play little role in the process of re-pigmentation in the dermabraded vitiliginous skin.
When the present study compared with non-cultured melanocytes-keratinocytes transplant; Muleker et al. [18- 21] reported 56% excellent re-pigmentation within 1 - 6 years. While El-Zawahry et al. [22] noticed excellent repigmentation in 32% of cases after 6 - 17 months follow up. While in the present work we had mean of 36.78% rate of re-pigmentation at 6 months.
To enhance the rate of re-pigmentation we strongly recommend increasing the amount of melanocytes in the debraded tissue that transferred from donor into recipient area.
In some cases also melanocytes transfer by dermabrasion could be repeated until we have complete re-pigmentation.
In conclusion, direct melanocytes transplant from normal donor into vitiliginous recipient area by dermabrasion technique is a new approach easy to perform, noncostly and take short time. The re-pigmentation was 36.78% at six months without any complications.
REFERENCES
- K. E. Sharquie, “Vitiligo,” Clinical and Experimental Dermatol, Vol. 9, No. 2, 1984, pp. 117-126.
- K. E. Sharquie, “The Histology and Immunopathology of Vitiligo,” Ph.D. Thesis, University of Sheffield, England, 1982.
- K. E. Sharquie, “Stages of Depigmentation in Vitiligo,” Iraqi Medical Journal, Vol. 36, 1988, pp. 47-50.
- K. E. Sharquie, S. H. Mehenna, A. A Naji and H. AlAzzawi, “Inflammatory Changes in Vitiligo: Stage I and II Depigmentation,” American Journal of Dermatopathology, Vol. 26, No. 2, 2004, p. 108.
- M. B. Abdel-Naser, S. K. Hann and J. C. Bystryn, “Oral Psoralen with UV-A Therapy Releases Circulating Growth Factors That Stimulates Cell Proliferation,” Archives of Dermatology, Vol. 133, No. 12, 1997, pp. 1530-1533.
- K. E. Shaquie and M. H. Majeed, “Treatment of Vitiligo by Topical Application of 5% Tincture Iodine in Comparison with 8-Methoxypsoralen Lotion (0.3%),” Journal of Pan-Arab League of Dermatologist, Vol. 12, No. 1, 2001, pp. 27-33.
- M. D. Njoo, J. D. Bos and W. Westerhof, “Treatment of Generalized Vitiligo in Children with Narrow-Band (TL-01) UVB Radiation Therapy,” Journal of the American Academy of Dermatology, Vol. 42, No. 2, 2011, pp. 245-253. doi:10.1016/S0190-9622(00)90133-6
- K. E. Sharquie, H. R. Al-Hammay and M. H. Al-Obeidy, “Treatment of Vitiligo with Topical Tincture Iodine 5% Solution and Ultaraviolet Light,” Thesis for Fellowship of Iraqi Board for Medical Specializations in Dermatology and Venereology, 2005.
- K. E. Sharquie and M. Y. Saeed, “Treatment of Vitiligo with Topical 15% Lactic Acid Solution in Comparison with Other Topical Therapies in Vitiligo,” Thesis for Fellowship of Iraqi Board for Medical Specializations in Dermatology and Venereology, 2002, pp. 36-46.
- K. E. Sharquie and M. S. Abdulla, “Treatment of Vitiligo by Topical Application of Lactic Acid 15% in Combination with Ultra Violet-A,” Saudi Medical Journal, Vol. 25, No. 5, 2005, pp. 1013-1015.
- S. S. Savant, “Miniature Punch Grafting,” In: S. S. Savant, Ed., Association of Scientific Cosmetology and Dermatosurgeons Textbook of Dermatosurgery and Cosmetology, 2nd Edition, ASCAD, Mumbai, 2005, pp. 359-369.
- S. Malakar and S. Dhar, “Repigmentation of Vitiligo Patches by Transplantation of Hair Follicles,” International Journal of Dermatology, Vol. 38, 1999, pp. 237- 238.
- R. Falabella, “Surgical Therapies for Vitiligo and Other Leukoderma, Part 1: Minigrafting and Suction Epidermal Grafting,” Dermatol Ther, Vol. 14, 2001, pp. 7-14.
- K. E. Sharquie, “Pigment Minigrafting as Treatment for Dermatomal Vitiligo,” The 9th Scientific Congress, College of Medicine, University of Baghdad, Baghdad, 1996.
- M. Ozdemir, O. Cetinkale, R. Wolf, A. Kotogyan, C. Mat, B. Tuzun and Y. Tuzun, “Comparison of Two Surgical Approaches for Treating Vitiligo: A Preliminary Study,” International Journal of Dermatology, Vol. 41, No. 3, 2002, pp. 135-138.
- A. M. Kahn and M. J. Cohen, “Treatment by Dermabrasion and Epithelial Sheet Grafting,” Journal of the American Academy Dermatology, Vol. 33, No. 4, 1995, pp. 646-648.
- K. Agrawal and A. Agrawal, “Repigmentation with Dermabrasion and Thin Split-Thickness Skin Graft,” Dermatologic Surgery, Vol. 21, No. 4, 1995, pp. 295-300.
- S. V. Mulekar, “Long-Term Follow-Up Study of 142 Patients with Vitiligo Vulgaris Treated by Autologous, NonCultured Melanocyte-Keratinocyte Cell Transplantation,” International Journal of Dermatology, Vol. 44, No. 10, 2005, pp. 841-845.
- S. V. Mulekar, A. Al Issa and A. Al Eisa, “Treatment of Vitiligo on Difficult-to-Treat Sites Using Autologous NonCultured Cellular Grafting,” Dermatologic Surgery, Vol. 35, No. 1, 2009, pp. 66-71.
- S. V. Mulekar, “Stable Vitiligo Treated by a Combination of Low-Dose Oral Pulse Betamethasone and Autologous, Melanocyte-Keratinocyte Cell Transplantation,” Dermatologic Surgery, Vol. 32, No. 4, 2006, pp. 536-541. doi:10.1111/j.1524-4725.2006.32109.x
- S. V. Mulekar, B. Ghwish, A. Al Issa and A. Al Eisa, “Treatment of Vitiligo Leasions by ReCell vs Conventional Melanocyte-Keratinocyte Transplantation: Pilot Study,” The British Journal of Dermatology, Vol. 158, No. 1, 2007, pp. 45-49.
- B. M. El-Zawahry, N. S. Zaki, D. A. Bassiouny, R. M. Sobhi, A. Zaghloul, M. M. Khorshied and H. M. Gouda, “Atologous Melanocyte-Keratinocyte Suspension in the Treatment of Vitiligo,” Journal of European Academy of Dermatology and Venereology, Vol. 25, No. 2, 2011, pp. 215-220.
- R. Czajkowski, W. Placer, T. Drewa, B. Kowaliszyn, J. Sir and W. Weiss, “Autologous Cultured Melanocytea in Vitiligo Treatment,” Dermatologic Surgery, Vol. 33, No. 9, 2007, pp. 1027-1036.
- S. Sethi, B. B. Mahajan, R. R. Gupta and A. Ohri, “Comparative Evaluation of the Therapeutic Efficacy of Dermabrasion, Dermabrasion Combined with Topical 5% 5- Fluorouracil Cream, and Dermabrasion Combined with Topical Placentrex Gel in Localized Stable Vitiligo,” International Journal of Dermatology, Vol. 46, No. 8, 2007, pp. 875-879.
- N. S. Mohamed, M. F. Elgoweini and N. A. Khad, “Dermatomal Vitiligo: Therapeutic Implication of Dermabration,” Journal of Pan-Arab Leaguo of Dermatologists, Vol. 19, 2008, pp. 21-29.
- P. Redondo, A. G. Azcarate, L. Marques, M. G. Guzman, E. Andreu and F. Prosper, “Amniotic Membrane as a Scaffold for Melanocytes Transplantation in Patients with Stable Vitiligo,” Dermatology Research and Practice, 2011, Article ID: 532139. doi:10.1155/2011/532139
- O. T. Vázquez-Martínez, H. G. Matínez-Rodríguez, L. Velásquez-Arenas, D. Baños-González, R. Ortíz-López, G. Padilla-Rivas, O. Welsh and J. Ocampo-Candiani, “Treatment of Vitiligo with a Melanocytes-Keratiocyte Cell Suspension versus Dermabrasion Only: A Pilot Study with a 12 Month Follow up,” Journal of Drug in Dermatology, Vol. 10, No. 9, 2011, pp. 1032-1036.
NOTES
*Disclosure: This is an independent study, not funded by any company.
#Corresponding author.

