Health
Vol.5 No.1(2013), Article ID:26524,9 pages DOI:10.4236/health.2013.51010
Occupational exposures to blood and body fluids (BBF): Assessment of knowledge, attitude and practice among health care workers in general hospitals in Lebanon
![]()
1Faculty of Public Health, Lebanese University, Saida, Lebanon; *Corresponding Author: nsdroubi@inco.com.lb
2Faculty of Economic Sciences and Business Administration, Lebanese University, Nabatieh, Lebanon
3Doctoral School of Literature, Humanities & Social Sciences, Lebanese University, Beyrouth, Lebanon
4Institute of Social Science, Lebanese University, Saida, Lebanon
Received 15 November 2012; revised 16 December 2012; accepted 23 December 2012
Keywords: Occupational Exposure to Blood and Body Fluids; Evaluation of the Professional Practice; Knowledge, Attitude, and Practices (KAP); Controlled Language; Healthcare Workers
ABSTRACT
Healthcare workers (HCWs) who are employed in traditional health care workplaces face a serious danger that may threaten their life; it is their exposure to blood and body fluids (BBF). In Lebanon, the introduction of a hospital accreditation system has put a particular emphasis on staff safety, and on the evaluation of professional practice (EPP) programs. Methods: A crosssectional survey was conducted amongst 277 HCWs working in 4 general hospitals in South Lebanon. Objective: 1) describe the prevalence and the risk factors for occupational exposure to BBF among HCWs; 2) evaluate knowledge, attitude, and practices of HCW concerning bloodborne pathogens and adherence to universal safety precautions. Results: The mean age of the respondents was 32.14 years (SD = 10.33), 57.4% were females. 43.3% of HCWs expressed that they use gloves all the time for every activeity of care. 67.1% were aware that needles should not be recapped after use; registered nurses and nursing students were more aware than physicians and nursing assistants (nurse) in this subject. 30% of HCWs declared having had at least one occupational exposure to BBF; 62.7% of all accidental exposure was reported to the department responsible for managing exposures. Percutaneous injuries were the most frequently reported. Vaccination coverage was 88.4% for hepatitis B, and 48.4% against influenza. The source patient was tested in 43.4% of reported BBF exposures. Accidental exposure to BBF was more frequent in older people (OR = 3.42; p = 0.03) and the more experienced. Subjects working in intensive care unit ward reported more exposure to BBF (OR = 3; p = 0.04). Participants incurring exposure to BBF resorted to different measures after the injury suggesting a lack of a uniform policy for post-exposure prophylaxis. Conclusion: Exposure to BBF represents an important and frequently preventable occupational hazard for HCWs in Lebanon that requires continuous EPP of HCWs, and a comprehensive approach for prevention and management.
1. INTRODUCTION
Healthcare workers (HCWs) who are employed in traditional health care workplaces face a serious danger that may threaten their life; it is their exposure to blood and body fluids (BBF). Indeed, accidental exposure may lead to infections by bloodborne pathogens, (BBPs) particularly hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). Data in the literature indicate that the average risk of seroconversion after a single percutaneous exposure to an infected blood is approximately 2% for HCV, 6% - 60% for HBV, and 0.1% - 0.3% for HIV [1]. Over 90% of these infections take place in low-income countries [2,3].
These injuries have many effects: the direct and indirect costs of the post-exposure medical treatment and the disability and absenteeism of the injured HCW [4]. However, this exposure can have a further influence on the quality of life of the injured HCW, and can cause great worry, anxiety, and fear for himself and his family and colleagues [5], as well as feelings of stigma and low self-confidence [6].
Occupational transmission of bloodborne infections may occur through parenteral, mucous membranes, and non intact skin exposure. The greatest risk for transdermal transmission is via a skin penetration injury sustained with a sharp hollow-bore needle that recently have been removed from a blood-contaminated source [7], or through contact of the eye, nose, mouth, or skin with a patient’s blood.
International health organizations [1,8-10] have published guidelines for the management of occupational blood exposure. These recommendations have become the standard of care for occupational exposure to BBF. Improvement in the diagnosis of infectious diseases transmitted by blood and body fluids, and growing concerns of the risks of work activities have led to the creation of surveillance teams in healthcare centers [11].
Very little data and limited surveillance regarding health care-related occupational exposures and the use of postexposure prophylaxis (PEP) exist in Lebanon [12,13] and the Arabic countries [14,15]. In Lebanon, in 2001, the rates of exposure to BBF were found to be 9% for medical student, 8% for attending physicians, and 5% for nurses [13].
In Lebanon, the introduction of a hospital accreditation system by the Ministry of Public Health in collaboration with the French Higher Health Authority is aiming to create incentives for continuous quality improvement, and evaluate both the safety and the quality of healthcare provision by developing an external evaluation system [16,17]. In the original standards, emphasis was put on organizational aspects and staff qualification and skills. Written protocols were required [16]. They mostly were written in French, or English. A particular emphasis was put on patient and staff safety [16,18], and an evaluation of professional practice (EPP) programs including reporting and surveillance of health risks among patients, and healthcare workers was implemented [19,20].
The focus of this study is 1) to describe the prevalence and the risk factors for occupational exposure to BBF among HCWs in private and public hospitals in south Lebanon; 2) to evaluate knowledge, attitude, and practices of HCW concerning blood-borne pathogens (e.g. HIV, HBV and HCV) and adherence to universal safety precautions, and 3) to create baseline data for future improvement.
2. METHODS
2.1. Data Collection
From December 2011 to July 2012, a cross-sectional survey was conducted amongst HCWs working in 4 general hospitals (1 public and 3 private hospitals) in South Lebanon. The students specializing in nursing are trained in these hospitals as part of their degree in nursing.
The targeted population comprised registered nurses (RN) and nursing assistants (Nurse) currently involved in collecting blood samples and administering injections in all wards of the hospital. The physicians (interns, residents, specialists), and nursing students were also included in this study. Students in this group were required to implement policies and procedures of hospitals regarding hygiene practices during their clinical placements on a regular basis.
The survey aimed to reach all departments at each hospital and was performed for all of shift workers. The exclusion criteria were the HCWs working in laboratory and radiology departments as they form a different exposure category and hence need a separate study. Exposures involving non-visibly bloody solutions, and nonvisibly BBFs (such as tears, urine, sputum, and feces) were considered to have a negligible risk of infection transmission, in addition to exposures involving clean needles.
Expecting the frequency of exposure to BBF during last year to be around 25%, [15] alpha as 5% and margin of error at 5%, the sample size worked out to be 273 [21].
The data collection process involved presenting an anonymous, self-reporting questionnaire, based on available studies, the international guidelines [1,2,8-10,22]. The questionnaire was pre-tested and used for data collection. The questionnaires were administered after obtaining HCW’s consent.
Socio demographic characteristics (age, gender, occupation, department of HCW) and information regarding working experience as HCW were recorded. In addition, respondents were asked about the frequency of exposure to patients’ BBF that they had in the year preceding the study.
The assessment of the knowledge, attitude, and practices (KAP) of Lebanese HCWs regarding the use of protective measures, proper waste disposal after use, immunizations (against hepatitis B virus, diphtheria-tetanus-polio (DTP), and influenza), and prompt management of exposures including the use of post-exposure prophylaxis (PEP) were done through the questionnaire. HCWs were asked about the type of exposure (needle, laceration or splash), activity during exposure, seroconversion among exposed HCWs, and serological status of source patients in cases of exposure accidents.
2.2. Statistical Analysis
Statistical analysis was performed using SPSS version 16.0. Data are presented as mean ± standard deviation (SD), and percentage when appropriate. Analysis included the use chi-square for dichotomous variables.
A Multivariate analysis was conducted to predict factors influencing the occupational exposure to BBF. The analysis was performed by ordinal logistic regression of the dichotomized (yes/no) accidental exposure to BBF variable taking into account the age, gender, occupation, years of experience, work location, vaccination and others preventive measures. Results (expb) are presented as Odds ratios.
All reported p-values are 2-tailed and significance was established at p ≤ 0.01.
3. RESULTS
3.1. Participants’ Characteristics
From 300 HCW selected, the participants consisted of 277 (92.3%) individuals distributed among four groups: physicians (15.5%), RN (62.8%), nurses (13.4%), and students specializing in nursing (8.3%). All participants were between 16 and 64-year-old (mean age = 32.14; SD = 10.33; median = 29 years), and 57.4% were females. The information regarding participants’ work experience shows that 41.2% had been professionally active for less than 5 years. The mean duration of work experience was 8.26 years (SD = 7.64; range: 0 - 40 years). The older persons had more experience (r = 0.86). The HCWs worked in all departments of each hospital (Table 1).
• 3.2. Knowledge, Attitude and Practice of Exposure Prevention Measures (Table 2)
Use of gloves
Only 43.3% of HCWs reported that they use gloves all the time for every activity of care. The attitude of HCWs concerning the use of gloves during procedures changed according to the activity. The percentage of adherence was 82.8% for intravenous (IV) insertions, 65.4% for phlebotomies, and dropped respectively to 60% and 46.6% during intramuscular (IM) and subcutaneous (SC) injections.
Recapping of used needles, and use of sharp containers
Concerning recapping of needles, 67.1% were aware that needles should not be recapped after use and among them 13.4% practiced this method all the time with a statistically significant difference according to the job category of HCW. The RNs and students were more aware than the physicians and nurses (74.7%, and 65.2% vs. 51%; p < 0.001). 67% of HCWs declared that needles should not be removed with hands before disposal. 63.9% knew that the ideal method of disposal of sharp waste (e.g. needles, scalpels) was to put it in a container located as close as feasible to the area of care, immediately after use, and put this activity into their regular
Table 1. Study participants’ characteristics.
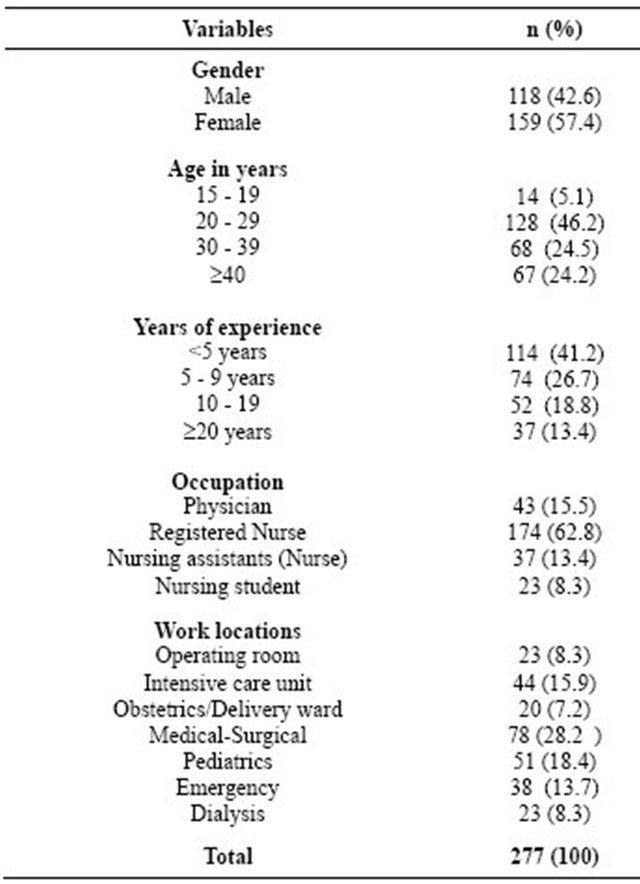
n: number of individual.
practice.
Vaccination against hepatitis B, diphtheria-tetanus-polio (DTP), and influenza
Vaccination coverage for obligatory vaccinations was 88.4% for hepatitis B, and 57.8% against diphtheriatetanus-polio (DTP). HCWs were vaccinated against DTP during childhood, without receiving the booster dose. For recommended vaccinations like influenza, the coverage was 48.4%, 9% declared that vaccination against influenza was not needed. Vaccination coverage is different between HCW categories: 34.8% of nursing students declared that they were not vaccinated against hepatitis B, and 52.2% not vaccinated against DTP (p ≤ 0.0001).
3.3. Accidental Exposure to BBF
Among 277 HCWs, 83 (30%) declared at least one occupational exposure to BBF.
The mean age of exposed HCW was 32.2 years (SD = 10.4 years), 52.2% were females. 57.8% were RNs. Nearly half (49.4%) of them have one accidental exposure and 39.8% had 2 - 5 exposures (Table 3).
Needlestick injury was the type of incident most frequently reported by healthcare staff (75.9%). The RNs, nurses, and nursing students were more exposed to needle stick injuries than physicians (89.6%, 71.4%, and
Table 2. Frequency of use of protective measures by HCW (Chi-square test results).

n: number of individuals; HCWs: Health care workers; RN: registered nurse; Nurse: Nursing assistant; IV: intravenous, IM: intramuscular; SC: subcutaneous; DTP: Diphtheria-tetanus-polio.
66.7% respectively vs 33.6%; p < 0.001). In contrast the physicians were more exposed to the cut injuries (50%) (Figure 1).
Percutaneous injuries occurring during sharps use accounted for 85.3% of all needle injuries. Intravenous injections (administration of medication, phlebotomy and drawing blood for “hemoglucotest”), and intramuscular or subcutaneous injections were the activities showing the highest frequency (42.0%), and (33.7%) respectively (Table 3).
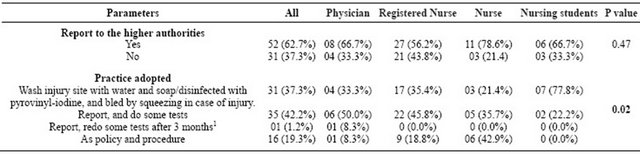
About two thirds (62.7%) of all accidental exposure to BBF was reported to the department responsible for managing exposures (e.g., occupational health, infection control, emergency rooms). This proportion did not vary
Table 3. Details of accidental exposure to blood and body fluids (BBF) amongst Health care workers (HCWs).

n: number of individual; SD: Standard deviation; Nurse: Nursing assistant; IM: intramuscular; SC: subcutaneous; IV: intravenous, 12 (2.4%) cases were associated with blood.
by occupation: RN (56.2%), Nurses (78.6%), and physician and nursing students (66.7%) (p value = 0.47). 37.3% of HCWs reported that in case of injury or splash of BBF, they washed thoroughly with soap and water, and disinfected with pyrovinyliodine, and bled by squeezing in case of injury. 19.3% reported that they adopted the procedures implemented in their hospitals’ without specification of the content.
The source patient was tested in 43.4% of reported BBF exposures. Only 1.2% of all exposures involved a source patient testing positive for one blood borne viruses. No one reported seroconversion among exposed HCWs (Table 4).
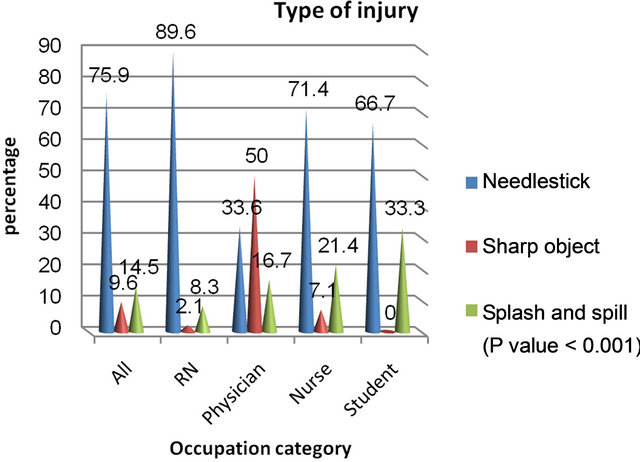
RN: Registered Nurse; Nurse: Nursing assistants, Student: Nursing student; (Chi-square = 32.4; p < 0.0001).
Figure 1. Type of injury according to occupation.
3.4. Factors Influencing the Accidental Exposure to BBF
Logistic regression analysis showed that the accidental exposure to BBF was more frequent in older HCWs (OR = 3.42; p = 0.03), and the more experienced. Subjects working in intensive care unit ward reported more exposure to BBF (OR = 3; p = 0.04). Indeed, avoiding to recap used needles (OR = −2.36; p = 0.04), and avoiding to remove needles with hand before disposal (OR = −2.61; p = 0.02), and sharp containers located as close as feasible to the area in which the items are used (OR = −2.12; p = 0.04) were significant preventive predictors of the accidental exposure to BBF (Table 5).
4. DISCUSSION AND CONCLUSIONS
This current study shows that exposure of HCWs to BBPs remains a problem in Lebanon.
The proportion of HCW who declared accidental exposure to BBF in our study was 30% and only two thirds of them reported their exposure to the department responsible for managing exposures. Almost similar results were reported in other studies [3,15,23,24]. We found that nursing personnel are the most commonly affected group. This is in agreement with other studies [11,23,25], but it differs from that reported by other authors who found the highest frequency of injury among physicians (55.1%), compared to nurses (22.0%) [13,24]. Several reasons may explain nurses’ higher rates of exposure. Indeed, nursing personnel are expected to do the routine blood draws, and IV insertion procedures [11]. In our study, the most exposed to BBF were the older and more experienced HCWs. This in contrast with data reported by others [15,26] where among injured persons, more than of 50% were young staff, and in the group with experience of less than 5 years. Increasing years of experi-
Table 4. Management of occupational exposures to BBF by HCWs (Chi-square test results).
Notes and abbreviations: BBF: blood and body fluids; HCWs: Health care workers; Nurse: Nursing assistant; 1The source patient testing positive for one blood borne viruses.
Table 5. Relationship between sociodemographic characteristics, protective measures, and exposure to BBF using multivariate analysis (logistic regression: Logit) (n = 277).
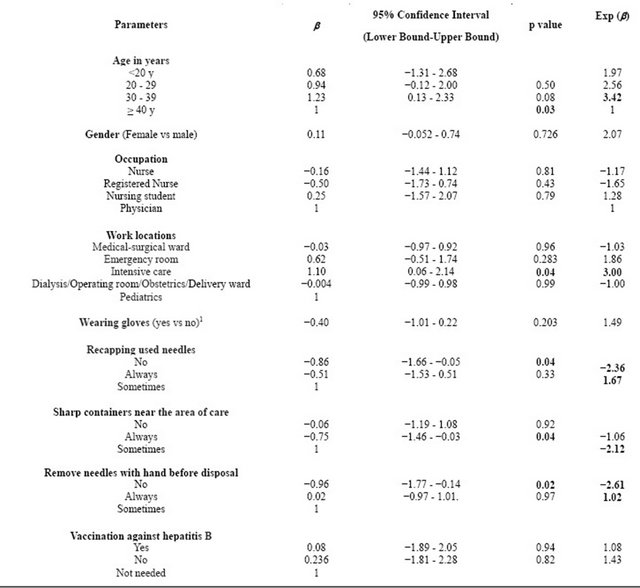
Notes and abbreviations: R-Square = 21.5%; Chi-Square of the total model = 45.482; p = 0.001; Intercept = −0.13. Values are represented as Odds ratios (OR) were derived from logistic regression model that controlled for age, gender, and occupation. 1Wearing gloves for all activities (recoded into 2 categories yes vs no).
ence may be a negative predictor of adherence to recommended practices by healthcare personnel as reported by Siegel et al. [27]. HCWs working in the ICU reported the largest proportion of exposures, and could be likely from the numerous interventions and devices used in these specialized settings [25].
Percutaneous exposures were the most frequently reported. This may be explained by the large number of tasks performed involving sharp material (intramuscular or intravenous administration of medication, drawing blood test…) [11,23,25], and /or the underreporting in activities where there is no percutaneous exposure (e.g. splash of BBF) [11].
Participants demonstrated their negative attitude towards accidental exposure to BBF prevention. The behavior of recapping needles persists despite the welldocumented dangers and international recommendations against this practice [1,9,22]. In addition, there are deficits in knowledge, and practice of simple protective measures such as wearing gloves, not removing needles with hand before disposal, and using disposal containers. While Aiken et al. [28], suggest that providing HCW with safer devices is warranted despite the higher costs of such devices and the seeming opposition of a sizable percentage of hospital managers to paying for them, Miceli et al. [29] found that the availability of resources and post exposure programs do not guarantee appropriate HCW behavior to adhere to protective measures, PEP and follow up in hospitals. The non-utilization of protective measures is indeed related to the “feeling that they are not needed” [13]. In this context, hospital administrators and the infection control teams should build safety consciousness and prompt staff to adopt participation in a “culture of safety”, wherein everyone commits to personal responsibility for safety [13].
As reported by others [10,24,30] the nursing and medical staffs were generally well covered by hepatitis B vaccination. However, the rate of vaccinated students against hepatitis B was low (52.2%). Concerning recommended vaccinations e.g. influenza, policy should be reinforced and the vaccination status for these vaccines should be better documented in all occupations [10,31].
Practice among HCWs about post occupational exposure to blood and body fluids is inadequate. Knowing the infectious-disease status of the source patient, as well as understanding the risks of transmission, might make HCWs more adherent to infectious-diseases prescriptions [29,32,33]. Testing for Hepatitis B surface antigen, HCV, and HIV is recommended at the time of injury. This is useful primarily as baseline evaluation [7]. The administration of the post-exposure prophylaxis is recommended for HCW who has been occupationally exposed to HBV (vaccine/immunoglobulin) and HIV (antiretroviral drugs) [9]. In the HCWs that have not been vaccinated, hepatitis B vaccination is recommended for any exposure regardless of the source person’s HBV status [9]. The HCW must allow the wound to bleed freely [1].
Immediately reporting blood exposure is very important [1]. In our study, like several studies, many exposures were not reported [24,30,34].
In our study a point of concern was nil or inappropriate post-exposure management; participants incurring exposure to BBF resorted to different measures after the injury suggesting a lack of a uniform policy for postexposure prophylaxis. The higher Authority of Health in France recommends “Reco2clics” which provides a format for recommendations for good practice in 2 clicks [35].
Our study has some limitations. It is a cross-sectional study design; it is unable to determine causal relationships [36]. In addition, self limitations in reporting were likely to occur [37]. No one reported a seroconversion (considered as taboos as others communicable disease) after exposure to BBF. While the sample size was adequate for this analysis, it is insufficient to allow for a more detailed analysis across different hospitals’ departments. This study was also limited to South Lebanon because of a lack of resources [37].
Whereas the access to registry of occupational exposure to BBF in the Infection Control Office of hospitals is mostly not allowed for researchers, self-reported morbidity is a useful measure because it allows public health researchers to obtain data from a random population sample and not only from those who need medical assistance [37]. This survey is based on the analysis of multiprofessional practices with reference to international recommendations. It is an essential element of the risk management since it may identify the immediate causes and latent occurrence of the adverse events occurring to HCWs, and prevent the recurrence of such events by implementing preventive measures [19].
In conclusion, achieving accreditation in hospitals in Lebanon does not guarantee that care is optimal, as reported by Ammar et al. [16]. The exposure to BBF represents an important and frequently preventable occupational hazard for HCWs that requires a comprehensive approach to prevention and management [25]. Knowledge about blood borne pathogens and universal precautions has been identified as a prerequisite for change in behavior and could be beneficial for protection of HCWs. We recommend more education for the HCWs to increase knowledge of good practice in this regard [2,18,38]. A hospital’s occupational post exposure management program should encourage prompt reporting, evaluation, and counseling, and should provide prophylactic drugs and follow-up [29].
Finally, the continuous evaluation of the professional practice of HCWs, and the development of protocols using a Controlled Language [35,39], without ambiguity, and written in Arabic may create an inherent culture of quality improvement, furnish evidence that policies and protocols are appropriate and are actually put into practice, and may provide a fast knowledge, and timely implementation of the management of occupational exposure to BBF.
5. ACKNOWLEDGEMENTS
The authors wish to acknowledge Mrs. F. Badran for her help and advice on the manuscript. We are grateful to the subjects who participated in this survey, and helped to carry out this study.
![]()
![]()
REFERENCES
- World Health Organization (WHO) (2010) Exposure to blood or other body. International Travel and Health: Situation as on 1 January 2010. World Health Organization, Geneva, 165-170. http://www.who.int/ith/ITH2010.pdf
- World Health Organization (2003) For a strategy to protect health workers from infection with bloodborne viruses. AIDE-MEMOIRE. World Health Organization, Geneva. http://www.who.int/injection_safety/toolbox/en/AM_HCW_Safety_EN.pdf
- Sangwan, M.C.B.R., Kotwal, C.A. and Verma, B.A.K. (2011) Occupational exposure to blood and body fluids amongst health care workers in a teaching hospital of the armed forces. Medical Journal Armed Forces India, 67, 21-24. http://medind.nic.in/maa/t11/i1/maat11i1p21.pdf
- Bassil, A.A. (2012) Sharps safety in hospitals. Human & Health, 18, 12-16.
- Gupta, A., Anand, S., Sastry, J., Krisagar, A., Basavaraj, A., Bhat, S.M., Gupte, N., Bollinger, R.C. and Kakrani, A.L. (2008) High risk for occupational exposure to HIV and utilization of post-exposure prophylaxis in a teaching hospital in Pune, India. BMC Infectious Diseases, 8, 142. doi:10.1186/1471-2334-8-142
- Gonzalez-Medina, D. and Le, Q.V. (2011) Infectious diseases and interpersonal trust: International evidence. Health, 3, 206-210. doi:10.4236/health.2011.34037
- Mathieu, N., Waseem, M., Gernsheimer, J.R., Kulkarni, R., Keim, S.M., Looneyand, D.G., et al. (2012) Body Fluid Exposures Treatment & Management, 6 p. http://emedicine.medscape.com/article/782611-overview#showall
- Wilburn, S.Q. and Eljkemans G. Y., (2004) Preventing needlestick injuries among healthcare workers: A WHOICN collaboration. International Journal of Occupational and Environmental Health, 10, 451-456. http://www.who.int/occupational_health/activities/5prevent.pdf
- Department of Health & Human Services, CDC (2008) Exposure to blood what healthcare personnel need to know. Centers for Disease Control and Prevention (CDC). http://www.cdc.gov/HAI/pdfs/bbp/Exp_to_Blood.pdf
- Guthmann, J.P. and Abiteboul, D. (2011) Vaccinations chez les soignants des établissements de soins de France, 2009. Couverture Vaccinale, Connaissances et Perceptions vis-à-vis des Vaccinations, Rapport Final 2011. Institut de Veille Sanitaire, Saint-Maurice, 76 p. http://opac.invs.sante.fr/doc_num.php?explnum_id=7347.
- Monge, V., Mato, G., Mariano, A., Fernández, C. and Fereres, J. (2001) Epidemiology of biological-exposure incidents among Spanish healthcare workers. Infection Control and Hospital Epidemiology, 22, 776-780. doi:10.1086/501862
- Kahhaleh, J.G. and Jurjus, A.R. (2005) Adherence to universal precautions among laboratory personnel in Lebanon. Eastern Mediterranean Health Journal, 11, 929-942. http://applications.emro.who.int/emhj/1105_6/11_5-6_2005_929_942.pdf
- Musharrafieh, U.M., Bizri, A.R.N., Nassar, N.T., Rahi, A.C., Shoukair, A.M., Doudakian, R.M., and Hamadeh, G.N. (2008) Health care workers’ exposure to bloodborne pathogens in Lebanon. Occupational Medicine, 58, 94-98. doi:10.1093/occmed/kqm139
- Khader, Y., Burgan, S. and Amarin, Z. (2009) Self-reported needle-stick injuries among dentists in north Jordan. Eastern Mediterranean Health Journal, 15, 185-189. http://applications.emro.who.int/emhj/1501/15_1_2009_0185_0189.pdf
- Sreedharan, J., Muttappallymyalil, J. and Venkatramana, M. (2010) Knowledge and practice of standard measures in occupational exposure to blood and body fluids among nurses in a University Hospital in the United Arab Emirates. Italian Journal of Public Health, 7, 90-94.
- Ammar, W., Wakim, R. and Hajj, I. (2007) Accreditation of hospitals in Lebanon: A challenging experience. Eastern Mediterranean Health Journal, 13, 138-149. http://applications.emro.who.int/emhj/1301/13_1_2007_138_149.pdf
- Salès-Wuillemin, E., Morlot, R., Fontaine, A., Pullin, W., Galand, Ch., Talon, D. and Minary-Dohen, P. (2011) Evolution of nurses’ social representation of hospital hygiene: From training to practice. Revue Européenne de Psychologie Appliquée, 61, 51-63. doi:10.1016/j.erap.2010.06.001
- Haute Autorité de Santé (HAS) (2012) Professional practice assessment. http://www.has-sante.fr/portail/jcms/c_408940/evaluation-des-pratiques-professionnelles
- MOPH (2008) Evaluation of Professional Practices (EPP) or clinical practice assessment. Lebanon, 4 p. http://www.moph.gov.lb/HospitalAccreditation/Documents/EPP.pdf
- MOPH (2008) PS: Patient safety and risk management. Lebanon. http://www.moph.gov.lb/HospitalAccreditation/Documents/PatientSafetyandRiskManagement.pdf
- Calculator, Raosoft (2004) Sample size. Raosoft. http://www.raosoft.com/samplesize.html
- World Health Organization (2007) Standard precautions in health care. WHO, Geneva. http://www.who.int/csr/resources/publications/EPR_AM2_E7.pdf
- Ndiaye, M., Cissokho, B.D. and Sow, M.L.L. (2011) Les accidents avec exposition au sang (AES) au CHNU de Fan de Dakar (Senegal). CAMIP—L’Actualite de la Sante au Travail, 1, 10 p. http://www.camip.info/IMG/pdf/AES_Senegal.pdf
- Wicker, S., Jung, J., Allwinn, R., Gottschalk, R. and Rabenau, H.F. (2007) Prevalence and prevention of needlestick injuries among health care workers in a German university hospital. International Archives of Occupational and Environmental Health, 81, 347-354. doi:10.1007/s00420-007-0219-7
- The National Surveillance System for Healthcare Workers (NaSH) (2007) Summary report for blood and body fluid exposure data collected from participating healthcare facilities. Centers for Disease Control and Prevention, 25 p. http://www.cdc.gov/nhsn/PDFs/NaSH/NaSH-Report-6-2011.pdf
- Fabin, C. and Fu-Prudhomot, P. (2008) Observatoire ACMS des accidents avec exposition au sang (AES) bilan de 5 ans de fonctionnement. Cahier de Medecine Inter Professionnelle, 2, 117-124. http://www.camip.info/IMG/pdf/ObservatoireAESACMS5ans2008-2-2.pdf
- Siegel, J.D., Rhinehart, E., Jackson, M., Chiarello, L., The Healthcare Infection Control Practices Advisory Committee (2007) Guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. CDC, 225 p. http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf
- Aiken, L.H., Sloane, D.M. and Klocinski J.L. (1997) Hospital nurses’ occupational exposure to blood: Prospective, retrospective, and institutional reports. American Journal of Public Health, 87, 103-107. doi:10.2105/AJPH.87.1.103
- Miceli, M., Herrera, F., Temporiti, E., Li, D., Vila, A. and Bonvehí, P. (2005) Adherence to an occupational blood borne pathogens exposure management program among healthcare workers and other groups at risk in Argentina. The Brazilian Journal of Infectious Diseases, 9, 454-458. doi:10.1590/S1413-86702005000600002
- Shiva, F., Sanaei, A., Shamshiri, A.R. and Ghotbi, F. (2011) Survey of needle-stick injuries in paediatric health personnel of 5 University Hospitals in Tehran. Journal of Pakistan Medical Association, 61, 127-131.
- Guthmann, J.-P., Fonteneau, L., Ciotti, C., Bouvet, E., Pellissier, G., Lévy-Bruhl, D. and Abiteboul, D. (2011) Couverture vaccinale des soignants travaillant dans les établissements de soins de France. Résultats de l’enquête nationale Vaxisoin, 2009. Bulletin Épidémiologique Hebdomadaire, 35-36, 371-376.
- Panlilio, A.L., Cardo, D.M., Grohskopf, L.A., Heneine, W. and Ross, C.S. (2005) Updated US public health service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. Morbidity and Mortality Weekly Report, 54, No. RR-9. http://www.cdc.gov/mmwr/PDF/rr/rr5409.pdf
- Baudu, A., Lot, F., Abiteboul, D., L’Hériteau, F., Touche, S., Giard, M., Jarno, P., Venier, A.-G., Bouvet, E., Rabaud, C., Floret, N., pour le Comité de Pilotage National de la Surveillance AES-Raisin-Geres (2011) Suivi des accidents exposant au sang chez les professionnels de santé non immunisés et exposés au VHB, 2005-2007 (France). Bulletin Épidémiologique Hebdomadaire, 35-36, 388-391. http://www.invs.sante.fr/Publications-et-outils/BEH-Bulletin-epidemiologique-hebdomadaire
- Ghofranipour, F., Asadpour, M., Ardebili, H.E., Niknami, S. and Hajizadeh, E. (2009) Needle sticks/sharps injuries and determinants in nursing care workers. European Journal of Social Sciences, 11, 191-197.
- Haute Autorité de Santé (HAS) (2012) Découvrez les recommandations cliquables “Reco2clics”. HAS, France. http://www.has-sante.fr/portail/jcms/c_1103133/decouvrez-les-recommandations-cliquables
- Dabis, F., Drucker, J. and Moren, A. (1992) Epidemiologie d’intervention. Arnette, Paris, 589 p.
- Sabbah, I., Vuitton, D.-A., Droubi, N., Sabbah, S. and Mercier, M. (2007) Morbidity and associated factors in rural and urban populations of South Lebanon: A crosssectional community-based study of self-reported health in 2000. Tropical Medicine and International Health, 12, 907-919. doi:10.1111/j.1365-3156.2007.01886.x
- Janjua, N.Z., Razaq, M., Chandir, S., Rozi, S. and Mahmood, B. (2007) Poor knowledge—Predictor of nonadherence to universal precautions for blood borne pathogens at first level care facilities in Pakistan. BMC Infectious Diseases, 7, 81. doi:10.1186/1471-2334-7-81
- Cardey, S., Anantapochal, R., Beddar, M., Devitre, D., Greenfield, P., Jin, G., Renahy, J., Spaggiari, L., Vuitton, D. (2009) Model for automatic translation system. Multilingual Project TACT Lise (Linguistics and Security). In: Actes du WISG’09, Workshop Interdisciplinaire sur la Sécurité Globale, Université de Technologie de Troyes, Troyes, 27-28 January 2009, CD-ROM, 10 p.

