Case Reports in Clinical Medicine
Vol.2 No.4(2013), Article ID:34092,4 pages DOI:10.4236/crcm.2013.24072
Localized pericarditis leading to clinical tamponade with profound shock status and syncope as a major clinical manifestation after posterior wall myocardial infarction—Characterization and descriptive findings by real-time 3-dimensional echocardiography
![]()
1Division of Cardiology, Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Taiwan; *Corresponding Author: jotaro3791@gmail.com
2Mackay Medicine, Nursing and Management College, Taipei, Taiwan
3Mackay Medical College, New Taipei City, Taiwan
Copyright © 2013 Po-Ching Chi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 18 April 2013; revised 21 May 2013; accepted 17 June 2013
Keywords: Pericarditis; Hemopericardium; Tamponade; Myocardial Infarction; Syncope
ABSTRACT
Pericarditis and hemopericardium causing cardiac tamponade, caused by large and transmural ventricular infarction with subsequent rupture into the pericardium, is a rare complication post acute myocardial infarction. This is frequently fatal with rapid clinical course. We reported a 65-year-old female who presented with persistent diaphoresis and dyspnea for several hours followed by syncope. Acute myocardial infarction was diagnosed with primary percutaneous coronary intervention performed though persistent hypotension was observed. Moderate amount of hemopericardium leading to tamponade was found. It was relieved after pericardiocentesis. Real-time three-dimensional echocardiography revealed blood clot with specific whirling pattern around the infracted ventricular wall with suspected leak.
1. INTRODUCTION
Patients are susceptible to a variety of cardiovascular complications following myocardial infarction (MI). Among them, pericarditis or pericardial effusion had been shown to decline in incidence at the current era of revascularization therapy [1]. Early infarct-associated pericarditis or namely “peri-infarction pericarditis”, a clinical scenario most usually seen in extensive anterior wall infarction, may present with pleuritic chest pain, friction rub, characteristic electrocardiographic (ECG) pattern of ST-segment elevation (65% - 70%) [2].
Regional pericarditis as an uncommon situation after MI rarely causes large effusion or clinical tamponade and is extremely difficult to be distinguished from myocardial infarction per se by traditional ECG [3]. Several prior studies had reported an extremely low incidence of typical ST-segment elevation as a typical pattern of global pericarditis [4]. Here in, we reported a 65-year-old female who suffered from acute ST-elevation MI and remained in hemodynamic compromise and persistent ST-elevation after successful revascularization. Illustratice regional pericarditis was diagnosed using bed-side echo with immediate pericardiocentesis performed and significant clinical improvement.
2. CASE REPORT
A 65-year-old female with type 2 diabetes suffered from diaphoresis and dyspnea for several hours followed by syncope was brought to our emergency department. Her blood pressure was measured to be 60/30 mmHg with pulse rate 119 beats/min on arrival. Immediate electrocardiogram (ECG) showed ST-segment elevations (3 mm) on leads II, III, AVF and V4-V6 with reciprocal V1-V3 ST-segment depression and elevated cardiac enzymes which favored the diagnosis of acute myocardial infarction.
Emergent coronary angiography showed complete occlusion of middle left circumflex (LCX-m) coronary artery with subsequent intravenous abciximab 12 mg infused continuously (0.125 mcg/kg/min) with a stent deployed successfully with no contrast extravasation during or after intervention. Intra-aortic balloon pump (IABP) was inserted after PCI due to shock status, however, hypotension persisted and her symptoms (dyspnea, diaphoresis and squeezing) did not improve even with mechanical ventilator support. Bedside echocardiography showed moderate amount pericardial effusion surrounding MI area with semi-fluid, sand-like content (Figure 1) formation and a hyper-enhanced area surrounded by clot formation which may indicate of the possible leak site. Real-time three-dimension echocardiocraphy (RT-3DE) revealed fog-like material with a whirling pattern approximate the inferolateral wall of left ventricle (Figures 2(A)-(F)).
After urgent pericardiocentesis immediately done and dark red blood of about 40 ml removal (Figure 3) with dis-continuation of abciximab, her blood pressure rose up to 120/90 mm Hg and heart rate decreased to 90 beats/min soon. Recovery of local elevated ST segment to normal was observed soon on subsequent bed-side ECG. The hemoglobin concentration of the pericardial effusion drained was 11.2 g/dL similar to serum hemoglobin 11.5 g/dL indicating a leak rather than inflammatory response. The patient discharged on the 7th day of admission and was doing well at subsequent follow up.
3. DISCUSSION
Here we present a case manifested as syncope, profound shock status and persistent ST elevation due to regional pericarditis and hemopericardium on the first day post myocardial infarction. Successful revascularization did not solve these clinical problems until pericardiocentesis was performed. Hemopericardium presented
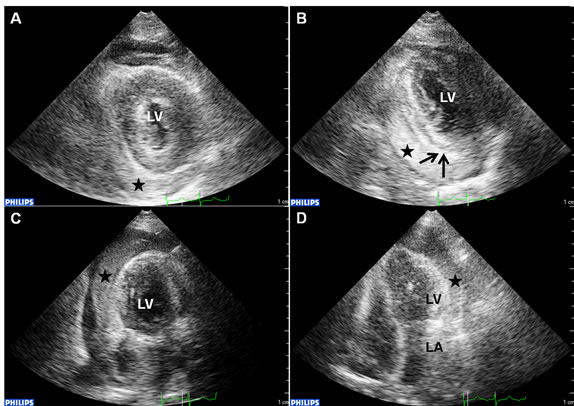
Figure 1. The para-sternal short-axis view (1A and 1B), apical two-chamber view (1C) and four-chamber view (1D) demonstrated the sand-like pericardial effusion (black star) surrounding the possible myocardial leak site (dark arrows). LV: left ventricle.
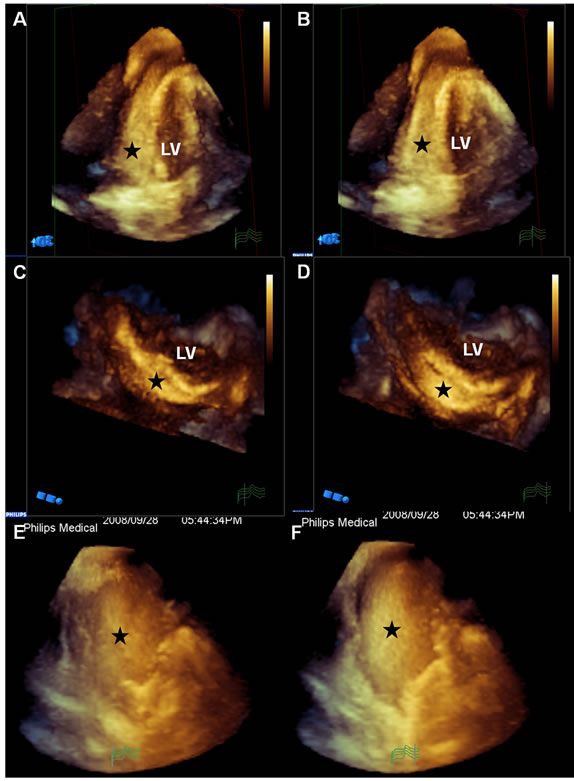
Figure 2. Three-dimensional (2A-F) echocardiograph were shown before pericardiocentesis. The semi-fluid, sand-like content (black star) approximate the inferolateral wall of left ventricle. From apical two-chamber view (2E and F), the whirling pericardial sand-like substance indicative of blood clot (black star) was well demonstrate. LV: left ventricle.

Figure 3. Under echocardiography guide, a 6 French drainage tube was inserted at the left 5th intercostal space in mid-clavicular line. Dark red blood of about 40 ml was drawn.
as acute pericarditis after infarction could be an malignant sign of subsequent ventricular rupture, leading to higher mortality rate [5]. In fact, there was a very low incidence (nearly 5%) of pericardial manifestations without cardiac rupture on the first day of MI in the modern era or reperfusion [6,7]. Pericardial involvement in the context of pericarditis following MI without subsequent rupture had also been shown to be associated with unfavorable outcomes [8,9]. Therefore, there is an urgent need for accurate diagnosis at an earlier stage with subsequent more aggresive therapeutic delivery. However, non-complicated regional pericardial effusion or transudate as common adverse events after myocardial infarction could be difficult to be distinguished from pericarditis-related hemopericardium [10]. Traditional imaging modality like echocardiography is important for early detection and accurate diagnosis [11]. In this regard, characteristic description of the non-complicated regional pericardial fluid that helps differentiate the true “risky components” may help therapeutic strategy decision. So far, regional pericarditis manifested as hemopericardium remained as a rare complication following large, transmural ventricular infarction [12]. Oliva and Mayo ever reported the atypical ECG natures with such regional pericarditis following MI, and so far there is no standardized ECG criteria in such clinical setting [3]. In their report of nearly 40 subjects, only 40% presented with persistent or recurrent ST segment elevation.
Contrast echocardiography or magnetic resonance imaging may be helpful in the early detection of the left ventricular wall partial rupture or tamponade formation [13,14]. In our patient, bed-side real-time three-dimension echocardiography (RT-3DE) was performed and showed fog-like, whirling material characterized by a specific whirling pattern (Figures 2(E) and (F)) surrounding the possible ventricular leak site. Though Möllmann et al. ever demonstrated a challenging case with isolated pericardial tamponade causing hypotension and persistent ST elevation following posterior wall MI [15]. They reported computed tomography as a useful tool in confirming diagnosis and successfully rescued the clinical setting. To our best knowledge, few reports ever presented this detailed, descriptive imaging of ventricular leak by RT-3DE before flank ventricular rupture. It was postulated in a case report that pericardiocentesis would lower the intra-pericardial pressure resulting in clot dislodging with further aggravated intrapericardial bleeding due to increased ventricular-pericardial pressure gradient [10]. In our case, simple pericardiocentesis successfully removed the hemopericardium without recurrence suggesting that the site of ventricular rupture or leak already sealed before pericardiocentesis. This case demonstrated that RT-3DE can provide detailed, characteristic images regarding the particular pattern of hemoperiacrdium which may help early identify the higher risk patients after myocardial infarction that may mandate immediate and aggressive intervention.
REFERENCES
- Dorfman, T.A. and Aqel, R. (2009) Regional pericarditis: A review of the pericardial manifestations of acute myocardial infarction. Clinical Cardiology, 32, 115-120. doi:10.1002/clc.20444
- Bainey, K.R. and Bhatt, D.L. (2009) Acute pericarditis: Appendicitis of the heart? Mayo Clinic Proceedings, 84, 5-6. doi:10.4065/84.1.5
- Oliva, P.B., Hammill, S.C. and Edwards, W.D. (1993) Electrocardiographic diagnosis of postinfarction regional pericarditis. Ancillary observations regarding the effect of reperfusion on the rapidity and amplitude of T wave inversion after acute myocardial infarction. Circulation, 88, 896-904. doi:10.1161/01.CIR.88.3.896
- Aydinalp, A., Wishniak, A., Van den Akker-Berman, L., Or, T. and Roguin, N. (2002) Pericarditis and pericardial effusion in acute ST-elevation myocardial infarction in the thrombolytic era. Israel Medical Association Journal, 3, 181-183.
- Køber, L., Møller, J.E. and Torp-Pedersen, C. (2010) Moderate pericardial effusion early after myocardial infarcttion: Left ventricular free wall rupture until proven otherwise. Circulation, 122, 1898-1899. doi:10.1161/CIRCULATIONAHA.110.986935
- Guereta, P., Khalifeb, K., Jobicc, Y., Fillipid, E., Isaaze, K., Tassan-Manginaf, S., Baixasg, C., Motreffh, P. and Meunei, C., (on Behalf of the Study Investigators) (2008) Echocardiographic assessment of the incidence of mechanical complications during the early phase of myocardial infarction in the reperfusion era: A French multicentre prospective registry. Archives of Cardiovascular Diseases, 101, 41-47. doi:10.1016/S1875-2136(08)70254-7
- Belkin, R.N., Mark, D.B. and Aronson, L. (1991) Pericardial effusion after intravenous recombinant tissue-type plasminogen activator for acute myocardial infarction. The American Journal of Cardiology, 67, 496. doi:10.1016/0002-9149(91)90010-I
- Widimsky, P. and Gregor, P. (1995) Pericardial involvement during the course of myocardial infarction. A longterm clinical and echocardiographic study. Chest, 108, 89. doi:10.1378/chest.108.1.89
- Sugiura, T., Iwasaka, T., Tarumi, N., et al. (1994) Clinical significance of pericardial effusion in Q-wave inferior wall myocardial infarction. The American Journal of Cardiology, 73, 862. doi:10.1016/0002-9149(94)90810-9
- Kaplan, K., Davison, R., Parker, M., Przybylek, J., Light, A., Bresnahan, D., et al. (1985) Frequency of pericardial effusion as determined by M-mode echocardiography in acute myocardial infarction. American Journal of Cardiology, 55, 335-337. doi:10.1016/0002-9149(85)90371-6
- Saito, Y., Donohue, A., Attai, S., Vahdat, A., Brar, R., Handapangoda, I., et al. (2008) The syndrome of cardiac tamponade with “small” pericardial effusion. Echocardiography, 25, 321-327. doi:10.1111/j.1540-8175.2007.00567.x
- Sugiura, T., Iwasaka, T., Takehana, K., et al. (1993) Clinical significance of pericardial effusion associated with pericarditis in acute Q-wave anterior myocardial infarction. Chest, 104, 415. doi:10.1378/chest.104.2.415
- Wilkenshoff, U.M., Ale Abaei, A., Kuersten, B., Pauschinger, M., Schwimmbeck, P., Hetzer, R., et al. (2004) Contrast echocardiography for detection of incomplete rupture of the left ventricle after acute myocardial infarction. Zeitschrift fur Kardiologie, 93, 624-629. doi:10.1007/s00392-004-0103-3
- Nemeth, M.A., Coulter, S. and Flamm, S.D. (2003) Pericarditis after myocardial infarction. Texas Heart Institute Journal, 30, 246-247.
- Möllmann, H., Zirlik, A., Nef, H.M., Weber, M., Hamm, C.W. and Elsässer, A. (2007) Left ventricular tamponade—A clinical chameleon. The Journal of Thoracic and Cardiovascular Surgery, 55, 325-327.

