International Journal of Otolaryngology and Head & Neck Surgery
Vol.05 No.02(2016), Article ID:64897,7 pages
10.4236/ijohns.2016.52016
Upper Cervical Spine Infection. Complication of Hypopharyngeal Injury
Ghassan Skaf*#, Elias Elias#
Division of Neurosurgery, Department of Surgery, American University of Beirut Medical Center, Beirut, Lebanon

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 25 June 2015; accepted 20 March 2016; published 23 March 2016
ABSTRACT
Background: We describe a rare case of Candida albicans retropharyngeal infection with upper cervical spondylodiscitis associated with epidural abscess triggered by ingestion of a chicken bone. Case Description: A 63-year-old woman presented with posterior neck and bilateral shoulders pain three weeks after choking on a 2-centimeter chicken bone. Magnetic resonance imaging (MRI) revealed spondylodiscitis and epidural abscess with significant spinal cord compression at C2 and C3 levels. A Barium swallow showed a focal disruption of the posterior wall of the esophagus. A posterior upper cervical fixation (C2-C5) was initially performed. One week later an anterior decompressive procedure was carried out followed by iliac crest bony fusion, and repair of the esophageal defect. Intra-operative cultures showed heavy growth of Candida albicans. After a transitory post-operative neurologic worsening, and after six weeks of appropriate antifungal therapy, the patient achieved a full clinical and radiologic recovery. Conclusion: Prompt surgical debridement, fusion and stabilization combined with adequate antimicrobial agents are necessary to guarantee a good outcome and reverse the neurological deficits.
Keywords:
Osteomyelitis, Cervical Spine, Discitis, Retropharyngeal Abscess, Candida albicans

1. Introduction
The majority of foreign bodies are ingested uneventfully via the intestinal tract but around 5% to 10% get stuck in the esophagus possibly leading to grave consequences [1] . Seeking medical care may be delayed in up to 50% of cases [2] . As a result a retropharyngeal abscess may ensue [3] . Cervical osteomyelitis is a rare condition, comprising only 2% to 7% of all bone conditions [4] . Although cervical spondylodiscitis is less common than thoracic and lumbar levels involvement, it can be a much more dramatic and rapidly deteriorating process, leading to early neurological deficits [5] .
Osteomyelitis is more common in immunocompromised patients, but can occur in immunocompetent individuals with no prior history of drug abuse [6] . Bacterial infections especially Staphylococcus aureus remain the most common cause of spondylodiscitis [7] - [11] , whereas Candida sp. are considered rare causative agents [12] .
In this paper, we report a rare case of retropharyngeal abscess, spondylodiscitis and epidural abscess with significant spinal cord compression at C2-C3 levels caused by Candida albicans.
2. Case Report
Presentation
A 63-year-old female, previously healthy, presented to an outside hospital with a 3-month history of neck and bilateral shoulder pain.
Her condition started after swallowing a chicken bone that got stuck in the throat for a few seconds. Later on, she developed dysphagia and underwent an upper endoscopy which revealed a superficial injury to the hypopharynx without obvious tear in the wall of the esophagus. She was discharged on oral antibiotics (Augmentin 1 g q12h) and steroids (Prednisone 20 mg bid) for a period of two weeks.
Her swallowing difficulties improved. However, one month after the initial accident, she developed neck pain radiating to both shoulders associated with low grade fever, she also complained of chest pain. A cervical spine MRI revealed a 2.5 × 1 × 0.5 cm anterior epidural and retropharyngeal abscess at the level of C2-C3 associated to compression of the spinal cord. She was started on Vancomycin (1 g q12h) and Meropenem (1 g q8h), but was shifted to Ciprofloxacin (750 mg q12h) and Tigecycline (100 mg then 50 mg every 12 hours) after she developed a diffuse rash. No surgical intervention was done at this stage. A repeat MRI two weeks later, revealed an increase in the epidural abscess size with progression of the spinal cord compression with evidence of C2-C3 frank osteomyelitis (Figure 1(a), Figure 1(b)).
At this point the patient was transferred to our institution at the American University of Beirut Medical Center (AUBMC) in a hard neck collar for further management.
Upon admission, the patient was afebrile, White Blood Count (WBC) = 15,300 with 52% neutrophils, Erythrocyte Sedimentation Rate (ESR) = 34 mm/hr (Nl 10-20) and C-reactive protein (C.R.P) = 10.4 mg/l (Nl 0-205). She was awake and oriented but walked with a spastic gait and mild imbalance. Neurological examination showed diffuse hyperreflexia in upper and lower extremities, proximal upper and lower extremities weakness of 4/5, right sided Hoffman sign and right Babinski sign. Patient was started on Tigecycline and Ceftazidime.
After a careful fiberoptic intubation, the patient underwent surgery and a posterior cervical fusion using pedicle

Figure 1. (a) Preop T1 WI MRI; (b) Pre operation T2 WI MRI.
and lateral mass screws (C2-C5). No decompression was done by fear of contaminating the posterior column. Extubation was carried successfully.
A barium swallow done two days post-operatively revealed a focal disruption of the posterior wall of the esophagus with a linear extravasation of contrast into the retropharyngeal space at C2-C3 level (Figure 2). A nasogastric tube was kept in place.
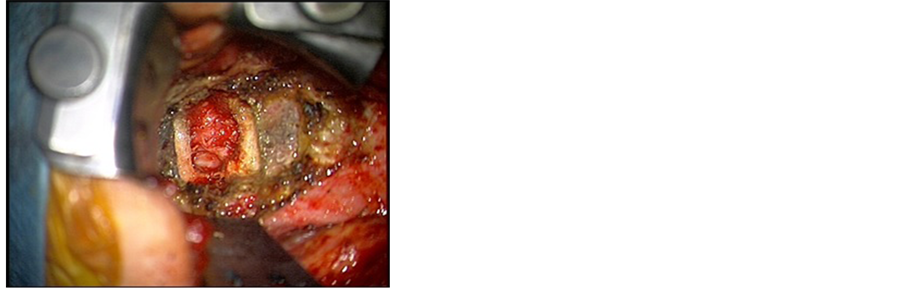
The patient underwent a second surgical procedure. A high right neck horizontal incision just below the level of the mandible was used, extending from the level of the sternocleidomastoid to the midline. After cutting the platysma, the deep neck structures were dissected. The major vessels were identified, and were retracted laterally. The larynx, trachea and underlying esophagus/hypopharynx were retracted medially, revealing the retropharyngeal space and longus colli muscle. A wide exposure was done without the need for submandibular resection [13] . The posterior aspect of the hypopharynx was carefully inspected and a small circular defect was identified representing the fistulous tract of a 1.5 cm diameter adherent to the abscess at C2-C3 disc level verified using C-arm. After minimal manipulation at the C2-C3 disc space, pus was expressed from the infected disc (Figure 3(a), Figure 3(b)).
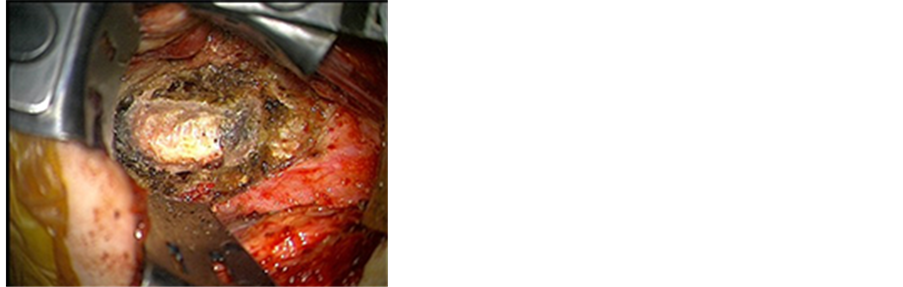
The infected disc was removed in a piecemeal fashion. The posterior longitudinal ligament had been breached by the abscess which was removed in total after drilling of both endplates and part of the vertebral bodies of C2 and C3, leading to adequate spinal cord decompression (Figure 4). Fusion was done using autologus bone graft harvested from the right iliac crest (Figure 5).
The sternocleidomastoid was carefully dissected along its length. The greater auricular nerve was identified and spared. The medial half of the muscle was separated from the bulk of the muscle and cut inferiorly, creating a superiorly-based muscle flap (Figure 6).
Figure 2. Pre operation barium swallow.
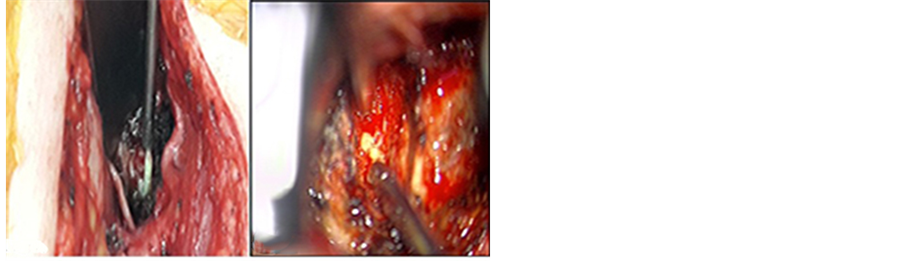
Figure 3. (a) (left) Intraoperative suctioning of purulent discharges (Macroscopic view); (b) (right) Intraoperative suctioning of purulent discharges (Microscopic view).
Figure 4. C2 C3 disc space after evacuation of the abscess and drilling of lower endplate of C2 and upper endplate of C3.
Figure 5. Fusion of C2 C3 using autologus bone graft harvested from right iliac crest.
Figure 6. Muscle flap from sternocleidomastoid muscle.
This flap was rotated medially and was used to close the hypopharyngeal defect completely (Figure 7(a), Figure 7(b)). A few sutures were taken to approximate the surrounding soft tissue structures to further seal the area of the defect. The NG tube was securely sutured to the patient’s collumella in anticipation for a long term use until a complete seal of the defect was secured. The patient tolerated the procedure well and left the Operating Room intubated in a stable condition.
Post-operatively the patient was kept intubated for five days after which a successful extubation was performed. The NG tube was kept in place for six weeks. A transitory proximal lower extremities weakness was noticed when ambulating the patient but eventually recovered three weeks later with the help of physiotherapy and aggressive rehabilitation (Figure 8(a), Figure 8(b)). Intra-operative cultures revealed heavy growth of Candida albicans for which fluconazole (400 mg per day for six weeks) was added to the treatment. Six months later patient presented to clinic for follow-up had significant improvement in her muscle tone. Barium swallow
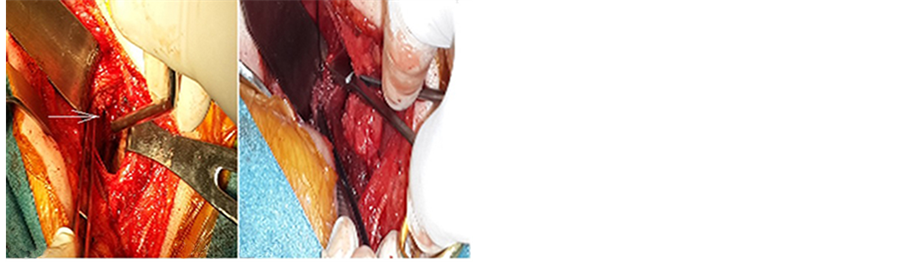
Figure 7. (a) Hypopharyngeal defect; (b) Closure of the defect using muscle flap.

Figure 8. (a) Post operation T2 WI MRI; (b) Post operation T1 WI MRI.
ordered revealed complete healing of the fistula.
3. Discussion
Cervical osteomyelitis is the least common location for spine infection [14] . Multiple causes have been postulated, such as direct spine trauma [15] , post-surgical manifestation [16] , hematogenous seeding [17] or a direct infection from a paravertebral space [18] . Symptoms upon presentation are vague, until neurological deficits develop, usually due to the long time lag between the onset of infection and the diagnosis [19] . In contrast to the thoracic spine area, the cervical spine has less stability and a smaller diameter of the bone canal. This narrow space will confer higher risk of neurological deficit and need an earlier aggressive treatment modality [20] .
Candida species, usually ubiquitous to skin and mucous membrane, are considered rare pathogens to cause osteomyelitis [21] . Candida albicans is the most prevalent in candida osteomyelitis [22] .
A delay between onset and presentation has been reported in the literature with an average of 3.3 months [21] , ranging from few days to more than one year [23] . In our case, endoscopy was done but did not unveil the full picture. However, barium swallow confirmed the retropharyngeal abscess.
Surgery is considered a necessity when there is compression of the spinal cord, when there is bony instability due to severe osteomyelitis or the presence of a severe pain despite conservative management [24] - [26] .
Surgical management involves debridement, neurological decompression, spine stabilization and alignment repair [27] . Anterior and posterior internal fixation should be performed to increase stability and maintain reduction [28] [29] . Grafting can be done in parallel with the stabilization process in order to hasten the healing process even in the presence of purulent material [30] .
4. Conclusion
While candida species are an unusual cause of spinal osteomyelitis, they should be considered in traumatic injuries. Prompt investigation with barium swallows and MRI should be initiated when we have high suspicion. Vertebral destruction associated with abscess formation and cord compression can result when no intervention is implemented. Prompt surgical debridement, fusion and stabilization combined with adequate antimicrobial agents are necessary to guarantee a good outcome and reverse the neurological deficits. Barium Swallow should be the first diagnostic modality in suspected cases following choking injuries. Posterior instrumentation can add to the stability of the spine provided no communication occurs between the posterior column and the rest of the infected spine. Anterior surgical debridement and decompression of the spinal cord followed by bony fusion is the gold standard for treatment, followed by appropriate antifungal treatment after culture results are out.
Cite this paper
GhassanSkaf,EliasElias, (2016) Upper Cervical Spine Infection. Complication of Hypopharyngeal Injury. International Journal of Otolaryngology and Head & Neck Surgery,05,96-102. doi: 10.4236/ijohns.2016.52016
References
- 1. Dahiya, M. and Denton, J.S. (1999) Esophagoaortic Perforation by Foreign Body (Coin) Causing Sudden Death in a 3-Year-Old Child. American Journal of Forensic Medicine & Pathology, 20, 184-188.
http://dx.doi.org/10.1097/00000433-199906000-00016 - 2. Fonga-Djimi, H., Leclerc, F., Martinot, A., Hue, V., Fourier, C., Deschildre, A. and Flurin, V. (1996) Spondylodiscitis and Mediastinitis after Esophageal Perforation Owing to a Swallowed Radiolucent Foreign Body. Journal of Pediatric Surgery, 31, 698-700.
http://dx.doi.org/10.1016/S0022-3468(96)90677-6 - 3. Ngan, J.H., Fok, P.J., Lai, E.C., Branicki, F.J. and Wong, J. (1990) A Prospective Study on Fish Bone Ingestion. Experience of 358 Patients. Annals of Surgery, 211, 459-462.
http://dx.doi.org/10.1097/00000658-199004000-00012 - 4. Sakamoto, M., Ichimura, K., Tayama, N., Nakamura, M. and Inokuchi, K. (1999) Cervical Vertebral Osteomyelitis Revisited: A Case of Retropharyngeal Abscess and Progressive Muscle Weakness. Otolaryngology—Head and Neck Surgery, 121, 657-660.
http://dx.doi.org/10.1016/S0194-5998(99)70078-1 - 5. Ruiz, A., Post, J.D. and Ganz, W.I. (1995) Inflammatory and Infectious Processes of the Cervical Spine. Neuroimaging Clinics of North America, 5, 401-425.
- 6. McCullers, J.A. and Flynn, P.M. (1998) Candida Tropicalis Osteomyelitis: Case Report and Review. Clinical Infectious Diseases, 26, 1000-1001.
http://dx.doi.org/10.1086/517629 - 7. Gouliouris, T., Aliyu, S.H. and Brown, N.M. (2010) Spondylodiscitis: Update on Diagnosis and Management. Journal of Antimicrobial Chemotherapy, 65, iii11-iii24.
http://dx.doi.org/10.1093/jac/dkq303 - 8. Belzunegui, J., Del Val, N., Intxausti, J.J., De Dios, J.R., Queiro, R., González, C., Rodríguez-Valverde, V. and Figueroa, M. (1999) Vertebral Osteomyelitis in Northern Spain. Report of 62 Cases. Clinical and Experimental Rheumatology, 17, 447-452.
- 9. Beronius, M., Bergman, B. and Andersson, R. (2001) Vertebral Osteomyelitis in Goteborg, Sweden: A Retrospective Study of Patients during 1990-95. Scandinavian Journal of Infectious Diseases, 33, 527-532.
- 10. Euba, G., Narváez, J.A., Nolla, J.M., Murillo, O., Narváez, J., Gómez-Vaquero, C. and Ariza, J. (2008) Long-Term Clinical and Radiological Magnetic Resonance Imaging Outcome of Abscess-Associated Spontaneous Pyogenic Vertebral Osteomyelitis under Conservative Management. Seminars in Arthritis and Rheumatism, 38, 28-40.
http://dx.doi.org/10.1016/j.semarthrit.2007.08.007 - 11. Hadjipavlou, A.G., Mader, J.T., Necessary, J.T. and Muffoletto, A.J. (2000) Hematogenous Pyogenic Spinal Infections and Their Surgical Management. Spine (Phila Pa 1976), 25, 1668-1679.
http://dx.doi.org/10.1097/00007632-200007010-00010 - 12. Derkinderen, P., Bruneel, F., Bouchaud, O. and Regnier, B. (2000) Spondylodiscitis and Epidural Abscess Due to Candida albicans. European Spine Journal, 9, 72-74.
http://dx.doi.org/10.1007/s005860050013 - 13. Skaf, G.S., Sabbagh, A.S. and Hadi, U. (2007) The Advantages of Submandibular Gland Resection in Anterior Retropharyngeal Approach to the Upper Cervical Spine. European Spine Journal, 16, 469-477.
http://dx.doi.org/10.1007/s00586-006-0228-3 - 14. Malawski, S.K. and Lukawski, S. (1991) Pyogenic Infection of the Spine. Clinical Orthopaedics and Related Research, No. 272, 58-66.
http://dx.doi.org/10.1097/00003086-199111000-00009 - 15. Korovessis, P., Sidiropoulos, P., Piperos, G. and Karagiannis, A. (1993) Spinal Epidural Abscess Complicated Closed Vertebral Fracture. A Case Report and Review of Literature. Spine (Phila Pa 1976), 18, 671-674.
http://dx.doi.org/10.1097/00007632-199304000-00020 - 16. Ghanayem, A.J. and Zdeblick, T.A. (1996) Cervical Spine Infections. Orthopedic Clinics of North America, 27, 53-67.
- 17. Yang, E.C. and Neuwirth, M.G. (1988) Pseudomonas Aeruginosa as a Causative Agent of Cervical Osteomyelitis. Case Report and Review of the Literature. Clinical Orthopaedics and Related Research, No. 231, 229-233.
http://dx.doi.org/10.1097/00003086-198806000-00031 - 18. Battista, R.A., Baredes, S., Krieger, A. and Fieldman, R. (1993) Prevertebral Space Infections Associated with Cervical Osteomyelitis. Otolaryngology—Head and Neck Surgery, 108, 160-166.
http://dx.doi.org/10.1177/019459989310800209 - 19. Reid, P.J. and Holman, P.J. (2007) Iatrogenic Pyogenic Osteomyelitis of C-1 and C-2 Treated with Transoral Decompression and Delayed Posterior Occipitocervical Arthrodesis. Case Report. Journal of Neurosurgery: Spine, 7, 664-668.
http://dx.doi.org/10.3171/SPI-07/12/664 - 20. Schimmer, R.C., Jeanneret, R.C., Nunley, P. and Jeanneret, B. (2002) Osteomyelitis of the Cervical Spine: A Potentially Dramatic Disease. Journal of Spinal Disorders & Techniques, 15, 110-117.
http://dx.doi.org/10.1097/00024720-200204000-00004 - 21. Khazim, R.M., Debnath, U.K. and Fares, Y. (2006)Candida Albicans Osteomyelitis of the Spine: Progressive Clinical and Radiological Features and Surgical Management in Three Cases. European Spine Journal, 15, 1404-1410.
http://dx.doi.org/10.1007/s00586-005-0038-z - 22. Lewis, R.E. and Klepser, M.E. (1999) The Changing Face of Nosocomial Candidemia: Epidemiology, Resistance, and Drug Therapy. American Journal of Health-System Pharmacy, 56, 525-533.
- 23. Hendrickx, L., Van Wijngaerden, E., Samson, I. and Peetermans, W.E. (2001) Candidal Vertebral Osteomyelitis: Report of 6 Patients, and a Review. Clinical Infectious Diseases, 32, 527-533.
http://dx.doi.org/10.1086/318714 - 24. Hsieh, P.C., Wienecke, R.J., O’Shaughnessy, B.A., Koski, T.R. and Ondra, S.L. (2004) Surgical Strategies for Vertebral Osteomyelitis and Epidural Abscess. Neurosurgical Focus, 17, E4.
http://dx.doi.org/10.3171/foc.2004.17.6.4 - 25. Chen, W.H., Jiang, L.S. and Dai, L.Y. (2007) Surgical Treatment of Pyogenic Vertebral Osteomyelitis with Spinal Instrumentation. European Spine Journal, 16, 1307-1316.
http://dx.doi.org/10.1007/s00586-006-0251-4 - 26. Darouiche, R.O. (2006) Spinal Epidural Abscess. The New England Journal of Medicine, 355, 2012-2020.
http://dx.doi.org/10.1056/NEJMra055111 - 27. Bydon, M., De la Garza-Ramos, R., Macki, M., Naumann, M., Sciubba, D.M., Wolinsky, J.P., Bydon, A., Gokaslan, Z.L. and Witham, T.F. (2014) Spinal Instrumentation in Patients with Primary Spinal Infections Does Not Lead to Higher Recurrent Infection Rates: An Analysis of 118 Cases. World Neurosurgery, 82, 807-814.
http://dx.doi.org/10.1016/j.wneu.2014.06.014 - 28. Guven, O. (1996) Posterior Instrumentation and Anterior Interbody Fusion for Tuberculous Kyphosis of Dorsal and Lumbar Spines. Spine (Phila Pa 1976), 21, 1840-1841.
- 29. Moon, M.S., Woo, Y.K., Lee, K.S., Ha, K.Y., Kim, S.S. and Sun, D.H. (1995) Posterior Instrumentation and Anterior Interbody Fusion for Tuberculous Kyphosis of Dorsal and Lumbar Spines. Spine (Phila Pa 1976), 20, 1910-1916.
http://dx.doi.org/10.1097/00007632-199509000-00013 - 30. Emery, S.E., Chan, D.P. and Woodward, H.R. (1989) Treatment of Hematogenous Pyogenic Vertebral Osteomyelitis with Anterior Debridement and Primary Bone Grafting. Spine (Phila Pa 1976), 14, 284-291.
NOTES

*Corresponding author.
#Ghassan Skaf: MD, FRCSC; Elias Elias: MD, MPH.