Advances in Microbiology
Vol.06 No.04(2016), Article ID:65937,7 pages
10.4236/aim.2016.64033
Detection of Listeria monocytogenes in Foods and Characterization by PFGE
Sanghun Park*, Hyowon Jung, Myungsuk Lee, Heejin Choi, Jimin Kim, Jihun Jung, Sungkyu Park, Musang Kim, Kyungsik Kim, Younghee Oh, Aehee Chung, Kweon Jung
Seoul Metropolitan Government Research Institute of Public Health and Environment, Gwacheon-si, Korea

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 11 March 2016; accepted 24 April 2016; published 27 April 2016
ABSTRACT
The aims of the present study were to investigate the prevalence of Listeria monocytogenes in 1042 foods collected from different market to characterize the isolates by phenotypical and molecular methods. In particular, L. monocytogenes obtained from different types of foods such as RTE (kimbap), fish (smoked salmon and seasoned-dried slice fish) and meat (cut raw beef and pork) from 2009 to 2011, were used. Twelve samples (2.1%) were positive for L. monocytogenes. Detection rate of L. monocytogenes varied significantly by food type and ranged from 1.1% to 5.2%. Meat is the highest prevalence for L. monocytogenes (5.2%) followed by RTE (1.8%) and Fish (1.1%). Twelve isolates were also serotyped by the agglutination method. The most common serotypes detected in the 12 strains tested were 1/4b (75.0%), followed by 1/2a (16.7%), and 1/2b (8.3%). For this study, we used serotyping and detected 6 different virulence-associated genes (inlA, inlB, plcA, plcB, hlyA, and actA) and 16s rRNA using multiplex-PCR. PFGE was performed to determine genetic characterization of L. monocytogenes strains to define the genetic diversity.
Keywords:
Listeria monocytogenes, PFGE, RTE

1. Introduction
L. monocytogenes continues to be an important food safety concern [1] . The etiological agent of listeriosis is L. monocytogenes, a gram-positive bacterium that contaminates meat, dairy products, unwashed raw vegetables, cabbage, and ready-to-eat food [2] - [4] . In immune-compromised individuals, L. monocytogenes causes meningitis, encephalitis, abortion in pregnant women and neonatal infections [5] . In the vast majority of human cases, infection is the result of consumption of contaminated food [6] .
Typing of L. monocytogenes isolates is another essential element of tracking bacterial contamination sources throughout food systems [7] - [11] . However, serotyping method often yields a low power of discrimination in strains [12] .
Reliable diagnosis of listeriosis is made by cultural methods, however, the isolation as well as the differentiation of pathogenic and non-pathogenic Listeria remains a time consuming and tedious task [13] . The pathogenic potential of Listeria isolates can be assessed by PCR multiple key virulence factors such as hlyA [14] , internalin A (inlA), internalin B (inlB) [15] , actA, plcA [16] , plcB [17] . Prf is required for the transcriptional activation of all the virulence genes of the cluster [18] .
PFGE has been considered as a standard subtyping method for L. monocytogenes [19] . The PFGE method has a high discriminatory power and has been shown to be very accurate and reproducible for fine structure comparison and molecular typing of L. monocytogenes [20] [21] .
The purpose of the present study was to investigate the prevalence of L. monocytogenes and examine genetic diversity of the L. monocytogenes isolates from RTE, meat and fish in Seoul, Korea.
2. Materials and Methods
2.1. Food Samples
We analyzed 1042 food samples taken from different markets in Seoul and obtained from different types of foods such as RTE (kimbap), fish (smoked salmon and seasoned-dried slice fish) and meat (cut raw beef and pork) from 2009 to 2011, were used.
2.2. Isolation of L. Monocytogenes
Twenty-five ml of buffer including the swabs were inoculated in 225 ml of Fraser Broth (Becton, Dickinson and company sparks, USA), and blended. All samples were incubated at 30˚C for 48 h. A portion (10 ul) of the enrichment broth was streaked on Palcam agar plate (Merk, Germany). After 24 - 48 h incubation at 37˚C the plates were examined for typical L. monocytogenes colonies, which were streaked for purity on horse blood agar plates. Hemolytic colonies on horse blood agar were confirmed as L. monocytogenes by API Listeria kit (Biomerieux, Korea).
2.3. Serotyping
The serotypingof L. monocytogenes isolates was performed by a slide agglutination assay using commercially prepared antisera (Listeria antiserum Seikenkit; DenkaSeikenCo, Tokyo, Japan) according to the manufacturer’s instruction.
2.4. Preparation of Genomic DNA
Genomic DNA was extracted using the AccuPrepⓡ Genomic DNA Extraction Kit (Bioneer, Korea) according to the manufacturer’s instruction.
2.5. Identification by the Multiplex-PCR of Virulence-Associated Genes
All of the primers used for specific PCR amplifications of the entire coding sequences of virulence-associated genes are reported in Table 1. PCR was performed in a PCR 9600 thermal cycler (Perkin-Elmer Corporation). A 50-ul aliquot contained buffer (10 mM Tris-HCl, 50 mM KCl, 2.5 mM MgCl2 [pH 8.3]), the dNTP mixture (TaKaRa, Japan) 0.25 mM each, 10 pmols of primer, 25 ng of DNA, and 0.8 U of Taq DNA polymerase (TaKaRa, Japan). The reaction conditions consisted of template DNA denaturation (94˚C for 3 min), 35 cycles of amplification (each cycle consisted of denaturation at 94˚C for 1 min, annealing at 60˚C for 2 min and elongation at 72˚C for 1min). 5 microlitre of the amplified products was separated by electrophoresis in 1.5% agarose gel containing ethidium bromide, and visualized under UV.
2.6. PFGE
PFGE was performed according to the PulseNet standardized protocol [22] , with ApaI as restriction endonuclease
Table 1. Primer pairs used for amplification of virulence genes and 16s rRNA in Listeria isolates.
(Roche, Germany). The electrophoretic parameters used were as follows; initial switch time, 4.0 s; final switch time, 40.0 s; sum time, 22 h; angle, 120˚; gradient, 6.0 V/cm; temperature, 14˚C; ramping factor, linear. After electrophoresis, the gels were stained for 15 - 20 min in 250 ml of deionized water containing 25 ul of ethidium bromide (10 mg/ml) and destained by three washes of 20 - 30 min each using 500 ml of deionized water.
3. Results
Of the samples examined, 12 (1.2%) were found to be positive for L. monocytogene. Listeria species were isolated in, 5 meat samples (cut raw beef and pork, 5.2%), 4 RTE (packed lunch boxes and kimbap, 1.8%), and 3 fish (smoked salmon and seasoned-dried slice fish, 1.1%), respectively.
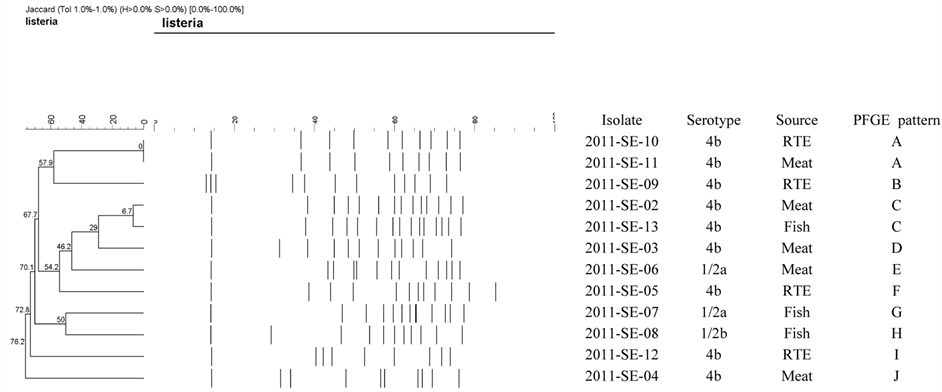
The serotype distribution of the 12 L. monocytogenes strains was as follows; 9 isolates (75.0%) belonged to serotype 4b, 2 isolates (16.7%) belonged to serotype 1/2a, 1 isolates (8.3%) belonged to serotype 1/2b, respectively (Figure 1).
PCR products of the 6 different virulence-associated genes and 16s rRNA (Table 1) were obtained DNA from all Listeria strains considered in this study, the isolates each had 16S rRNA and seven virulence-associated genes (hlyA, plcA, plcB, inlA, inlB, actA, and prfA), suggesting that they are potentially pathogenic.
PFGE (ApaI) types of all isolated strains are presented in Figure 1. It demonstrates examples of all PFGE types indicated in our studies. Among the 12, dendrogram analyses of the PFGE profiles showed that the 12 L. monocytogenes isolates from 10 different PFGE profiles with at 80% relative genetic similarity. The most predominant type was A and C.
4. Discussion
Even though L. monocytogenes causes relatively few cases of human disease in Korea and all over the world, it is still a major problem for public health because it is widespread and present in many animals, food products, raw materials, and the environment. A latest report from the Centers for Disease Control and Prevention (CDC) has estimated 1455 hospitalizations and 255 deaths per year in the United States [1] . More specific information of the ecological epidemiology and particularly of the genetic structure of Listeria should help us to understand
Figure 1. ApaI PFGE restriction patterns for selected L. monocytogenes isolates obtained from RTE, meat and fish in Seoul, Korea.
the origin of listeriosis in the future.
This study was designed to reveal any correlation between L. monocytogenes strains isolated from seven kinds of foods. The strains were analyzed by serotyping, virulence-associated genes, and PFGE. The results of this study showed that the highest contamination rates were meat, fish, and RTE foods, respectively. These findings are in agreement with previous report on outbreak of febrile gastroenteritis in Austria in which its contamination is fish and seafood, raw meat sausages, soft cheese and cooked meat [23] . These data are in concordance with the RTE foods observed by Allerberger et al. in a study performed in Germany [24] . They found to be recorded an outbreak of 16 cases caused by pre-sliced ready-to-eat (RTE) delicatessen meat (sausage salad) [24] . Moreover, evidence from EU-wide routine food safety investigations indicates that a substantial proportion of RTE products may be contaminated by L. monocytogenes [25] . The result also confirms RTE, meat, and fish are as one of the important enteropathogens responsible for listeriosis.
In the present study, the L. monocytogenes isolates were serotyped. All of the isolates belonged to serotype 4b, 1/2a, and 1/2b; thus, they also had the epidemic potential. A restricted range of strains was responsible for most of the additional cases at that time, and most human cases are still associated with L. monocytogenes serovars 1/2a, 1/2b and 4b [24] [26] .
Our results suggest that three major serotypes may be particularly important as most human infections are reported to be associated with 1/2a, 1/2b, and 4b. Therefore, most of the organisms isolated in this study could lead to human infections and are then possibly pathogenic for humans.
Molecular insight into the genetic characteristics of the 12 L. monocytogenes isolates by determining the presence of virulence-associated genes revealed that isolates carried all the seven traits studied, implying their high pathogenic potential.
In order to define the genetic diversity, we also compared PFGE analyses to determine the genetic characteristics of L. monocytogenes strains isolated from food samples. PFGE is a method with high discriminatory power and it has shown to be very accurate and reproducible for fine structure comparison and molecular typing of L. monocytogenes [12] [20] [21] [27] .
Our result showed L. monocytogenes isolates from various different PFGE profiles (10 pulsotypes) at 80% relative genetic similarity. The data from these studies indicate that we have identical pattern from different source with the same 4b serotype. It was shown that RTE (2011-SE-10) unrelated Meat (2011-SE-11) shared identical patterns, suggesting that they were serologically related. These data are in concordance with C pattern. Previous study indicated that the genetic patterns of strains showed no association with any of the properties that correlated with their origin [28] . It was found that similar subtypes of strains could be found in different product types and in different processing environments. The results of the present study clearly indicate that the recovery of identical patterns forming various food and patient strains does not prove that a particular food is the vehicle of infection [29] . It has been proposed a similar finding with an identical PFGE pattern that was shared by different serotypes, even from different flagella antigen groups [30] . It was shown that the poor correlation between serotyping and molecular subtyping may be due to horizontal gene transfers or point mutations in genomic DNA resulting in phenotypic shifts that affected serotyping [31] .
The results in this study showed specific PFGE types could not be connected with serotype, and especially most fish isolates could differentiate with C, G, and H pattern showing serotypes 1/2a, 1/2b, and 4b which is consistent with results observed in other studies having examined the relation of L. monocytogenes between subtypes and genotypes [32] [33] . It has been investigated that correlations between molecular subtyping and serotyping of L. monocytogenes have been reported previously [31] . Currently, there is no thorough knowledge of the molecular basis for the relationship between serotypes and molecular subtyping of L. monocytogenes [34] . Of interest, it was found that genomic DNA isolates of serotype 4b digested by ApaI enzyme in our study showed relatively distinguishable patterns. This finding is consistent with the study identical PFGE patterns belonged to the same serotype [29] [35] .
The application of molecular typing methods for investigating the source of contamination in meat, fish, and RTE foods may lead to a better understanding of the routes of L. monocytogenes spread, thus allowing taking serious measurements to reduce the occurrence of L. monocytogenes in the food production chain.
Cite this paper
Sanghun Park,Hyowon Jung,Myungsuk Lee,Heejin Choi,Jimin Kim,Jihun Jung,Sungkyu Park,Musang Kim,Kyungsik Kim,Younghee Oh,Aehee Chung,Kweon Jung, (2016) Detection of Listeria monocytogenes in Foods and Characterization by PFGE. Advances in Microbiology,06,343-349. doi: 10.4236/aim.2016.64033
References
- 1. Scallan, E., Hoekstra, R.M., Angulo, F.J., Tauxe, R.V., Widdowson, M.A., Roy, S.L., Jones, J.L. and Griffin, P.M. (2011) Foodborne Illness Acquired in the United States Major Pathogens. Emerging Infectious Diseases, 17, 7-15.
http://dx.doi.org/10.3201/eid1701.P11101 - 2. Todd, E.C.D. and Notermans, S. (2011) Surveillance of listeriosis and Its Causative Pathogen, Listeria monocytogenes. Food Control, 22, 1484-1490.
http://dx.doi.org/10.1016/j.foodcont.2010.07.021 - 3. Ferreira, V., Wiedmann, M., Teixeira, P. and Stasiewicz, M.J. (2014) Listeria monocytogenes Persistence in Food-Associated Environments: Epidemiology, Strain Characteristics, and Implications for Public Health. Journal of Food Protection, 77, 150-170.
http://dx.doi.org/10.4315/0362-028X.JFP-13-150 - 4. Lomonaco, S., Nucera, D. and Filipello, V. (2015) The Evolution and Epidemiology of Listeria monocytogenes in Europe and the United States. Infection, Genetics and Evolution, 35, 172-183.
http://dx.doi.org/10.1016/j.meegid.2015.08.008 - 5. Bonazzi, M., Lecuit, M. and Cossart, P. (2009) Listeria monocytogenes Internalin and Ecadherin: from Structure to Pathogenesis. Cellular Microbiology, 11, 693-702.
http://dx.doi.org/10.1111/j.1462-5822.2009.01293.x - 6. Fenlon, D.R., Wilson, J. and Donachie, W. (1996) The Incidence and Level of Listeria monocytogenes Contamination of Food Sources at Primary Production and Initial Processing. Journal of Applied Bacteriology, 81, 641-650.
http://dx.doi.org/10.1111/j.1365-2672.1996.tb03559.x - 7. Autio, T., Hielm, S., Miettinen, M., Sjoberg, A.M., Aarnisalo, K., Bjorkroth, J., Mattila, S.T. and Korkeala, H. (1999) Sources of Listeria monocytogenes Contamination in a Cold-Smoked Rainbow Trout Processing Plant Detected by Pulsed-Field Gel Electrophoresis Typing. Applied and Environmental Microbiology, 65, 150-155.
- 8. Johansson, T., Rantala, L., Palmu, L. and Honkanen-Buzalki, T. (1999) Occurrence and Typing of Listeria monocytogenes Strains in Retail Vacuum-Packed Fish and in a Production Plant. International Journal of Food Microbiology, 47, 111-119.
http://dx.doi.org/10.1016/S0168-1605(99)00019-7 - 9. Miettinen, M.K., Bjorkroth, K.J. and Korkeala, H.J. (1999) Characterization of Listeria monocytogenes from an Ice Cream Plant by Serotyping and Pulsed-Field Gel Electrophoresis. International Journal of Food Microbiology, 46, 187-192.
http://dx.doi.org/10.1016/S0168-1605(98)00185-8 - 10. Norton, D.M., McCamey, M.A., Gall, K.L., Scarlett, J.M., Boor, K.J. and Wiedmann, M. (2001) Molecular Studies on the Ecology of Listeria monocytogenes in the Smoked Fish Processing Industry. Applied and Environmental Microbiology, 67, 198-205.
http://dx.doi.org/10.1128/AEM.67.1.198-205.2001 - 11. Hoffman, A.D., Gall, K.L., Norton, D.M. and Wiedmann, M. (2003) Listeria monocytogenes Contamination Patterns for the Smoked Fish Processing Environment and for Raw Fish. Journal of Food Protection, 66, 52-60.
- 12. Heir, E., Lindstedt, B.A., Røtterud, O.J., Vardund, T., Kapperud, G. and Nesbakken, T. (2004) Molecular Epidemiology and Disinfectant Susceptibility of Listeria monocytogenes from Meat Processing Plants and Human Infections. International Journal of Food Microbiology, 96, 85-96.
http://dx.doi.org/10.1016/j.ijfoodmicro.2004.03.014 - 13. Rawool, D.B., Malik, S.V., Shakuntala, I., Sahare, A.M. and Barbuddhe, S.B. (2007) Detection of Multiple Virulence-Associated Genes in Listeria monocytogenes Isolated from Bovine Mastitis Cases. International Journal of Food Microbiology, 113, 201-207.
- 14. Riedo, F.X., Weaver, R.E., Plikaytis, B.D. and Broome, C.V. (1994) A Point-Source Food Borne Listeriosis Outbreak: Documented Incubation Period and Possible Mild Illness. The Journal of Infectious Diseases, 170, 693-696.
http://dx.doi.org/10.1093/infdis/170.3.693 - 15. Yong, S.J., Joseph, F., Frank, R., Brackett, E. and Jinru, C. (2003) Polymerase Chain Reaction Detection of Listeria monocytogenes on Frankfurters Using Oligonucleotide Primers Targeting the Genes Encoding Internalin AB. Journal of Food Protection, 66, 237-241.
- 16. Gianfranceschi, M., Fransiosa, G., Gattuso, A. and Aureli, P. (1998) Detection of Two Phospholipases C by Means of Plate Tests for the Rapid Identification of Pathogenic Listeria monocytogenes. Archiv fur Lebensmittelhygiene, 49, 54-57.
- 17. Winters, D.K., Maloney, T.P. and Johnson, M.G. (1999) Rapid Detection of Listeria monocytogenes by a PCR Assay Specific for an Aminopeptidase. Molecular and Cellular Probes, 13, 127-131.
http://dx.doi.org/10.1006/mcpr.1999.0224 - 18. Vázquez-Boland, J.A., Domínguez-Bernal, G., González-Zorn, B., Kreft, J. and Goebel, W. (2001) Pathogenicity Islands and Virulence Evolution in Listeria. Microbes and Infection, 3, 571-584.
http://dx.doi.org/10.1016/S1286-4579(01)01413-7 - 19. Graves, L.M., Hunter, S.B., Ong, A.R., Schoonmaker-Bopp, D., Hise, K., Kornstein, L., De Witt, W.E., Hayes, P.S., Dunne, E., Mead, P. and Swaminathan, B. (2005) Microbiological Aspects of the Investigation That Traced the 1998 Outbreak of Listeriosis in the United States to Contaminated Hot Dogs and Establishment of Molecular Subtyping-Based Surveillance for Listeria monocytogenes in the PulseNet Network. Journal of Clinical Microbiology, 43, 2350- 2355.
http://dx.doi.org/10.1128/JCM.43.5.2350-2355.2005 - 20. Graves, L.M. and Swaminathan, B. (2001) PulseNet Standardized Protocol for Subtyping Listeria monocytogenes by Macrorestriction and Pulsed-Field Gel Electrophoresis. International Journal of Food Microbiology, 65, 55-62.
http://dx.doi.org/10.1016/S0168-1605(00)00501-8 - 21. Wagner, M., Auer, B., Trittremmel, C., Hein, I. and Schoder, D. (2007) Survey of the Listeria Contamination of Ready-to-Eat Food Products and Household Environments in Vienna, Austria. Zoonoses and Public Health, 54, 16-22.
http://dx.doi.org/10.1111/j.1863-2378.2007.00982.x - 22. Allerberger, F. and Wagner, M. (2010) listeriosis: A Resurgent Foodborne Infection. Clinical Microbiology and Infection, 16, 16-23.
http://dx.doi.org/10.1111/j.1469-0691.2009.03109.x - 23. European Food Safety Authority (2009) The Community Summary Report on Trends and Sources of Zoonoses and Zoonotic Agents in the European Union in 2007. European Food Safety Authority Journal, 223, 118-141.
- 24. Tappero, J.W., Schuchat, A., Deaver, K.A., Mascola, L. and Wenger, J.D. (1995) Reduction in the Incidence of Human listeriosis in the United States: Effectiveness of Prevention Efforts? The Journal of the American Medical Association, 273, 1118-1122.
http://dx.doi.org/10.1001/jama.1995.03520380054035 - 25. Graves, L.M., Hunter, S.B., Ong, A.R., Schoonmaker-Bopp, D., Hise, K., Kornstein, L., DeWitt, W.E., Hayes, P.S., Dunne, E., Mead, P. and Swaminathan, B. (2005) Microbiological Aspects of the Investigation That Traced the 1998 Outbreak of listeriosis in the United States to Contaminated Hot Dogs and Establishment of Molecular Subtyping-Based Surveillance for Listeria monocytogenes in the PulseNet Network. Journal of Clinical Microbiology, 43, 2350-2355.
http://dx.doi.org/10.1128/JCM.43.5.2350-2355.2005 - 26. Bille, J. and Rocourt, J. (1996) WHO International Multicenter Listeria Monocytogenes Subtyping Study-Rationale and Set-Up of the Study. International Journal of Food Microbiology, 32, 251-262.
http://dx.doi.org/10.1016/S0168-1605(96)01140-3 - 27. Suihko, M.L., Salo, S., Niclasen, O., Gudbjörnsdóttir, B., Torkelsson, G., Bredholt, S., Sjöberg, A.M. and Gustavsson, P. (2002) Characterization of Listeria monocytogenes Isolates from the Meat, Poultry and Seafood Industries by Automated Ribotyping. International Journal of Food Microbiology, 72, 137-146.
http://dx.doi.org/10.1016/S0168-1605(01)00631-6 - 28. Martinez, I., Rørvik, L.M., Brox, V., Lassen, J., Seppola, M., Gram, L. and Fonnesbech-Vogel, B. (2003) Genetic Variability among Isolates of Listeria monocytogenes from Food Products, Clinical Samples and Processing Environments, Estimated by RAPD Typing. International Journal of Food Microbiology, 84, 285-297.
http://dx.doi.org/10.1016/S0168-1605(02)00423-3 - 29. Autio, T., Lundén, J., Fredriksson-Ahomaa, M., Björkroth, J., Sjöberg, A.M. and Korkeala, H. (2002) Similar Listeria monocytogenes Pulsotypes Detected in Several Foods Originating from Different Sources. International Journal of Food Microbiology, 77, 83-90.
http://dx.doi.org/10.1016/S0168-1605(02)00055-7 - 30. Margolles, A., Mayo, B. and de los Reyes-Gavilan, C.G. (1998) Polymorphism of Listeria monocytogenes and Listeria innocua Strains Isolated from Short-Ripened Cheeses. Journal of Applied Microbiology, 84, 255-262.
http://dx.doi.org/10.1046/j.1365-2672.1998.00339.x - 31. Nadon, C.A., Woodward, D.L., Young, C., Rodgers, F.G. and Wiedmann, M. (2001) Correlations between Molecular Subtyping and Serotyping of Listeria monocytogenes. Journal of Clinical Microbiology, 39, 2704-2707.
http://dx.doi.org/10.1128/JCM.39.7.2704-2707.2001 - 32. Giovannacci, I., Ragimbeau, C., Queguiner, S., Salvat, G., Vendeuvre, J.L., Carlier, V. and Ermel, G. (1999) Listeria monocytogenes in Pork Slaughtering and Cutting Plants: Use of RAPD, PFGE and PCR-REA for Tracing and Molecular Epidemiology. International Journal of Food Microbiology, 53, 127-140.
http://dx.doi.org/10.1016/S0168-1605(99)00141-5 - 33. Wallace, F.M., Call, J.E., Porto, A.C., Cocoma, G.J. and Luchansky, J.B. (2003) Recovery Rate of Listeria monocytogenes from Commercially Prepared Frankfurters during Extended Refrigerated Storage. Journal of Food Protection, 66, 584-591.
- 34. Okwumabua, O., O’Connor, M., Shull, E., Strelow, K., Hamacher, M., Kurzynski, T. and Warshauer, D. (2005) Characterization of Listeria monocytogenes Isolates from Food Animal Clinical Cases: PFGE Pattern Similarity to Strains from Human listeriosis Cases. FEMS Microbiology Letters, 249, 275-281.
http://dx.doi.org/10.1016/j.femsle.2005.06.018 - 35. Chung, H.C. and Wang, C. (2006) Genetic Relatedness between Listeria monocytogenes Isolates from Seafood and Humans Using PFGE and REP-PCR. International Journal of Food Microbiology, 110, 135-148.
http://dx.doi.org/10.1016/j.ijfoodmicro.2006.02.003
NOTES

*Corresponding author.