International Journal of Clinical Medicine
Vol.2 No.5(2011), Article ID:8778,6 pages DOI:10.4236/ijcm.2011.25096
Using the Mini Nutritional Assessment to Evaluate the Profile of Elderly Patients in a Geriatric Outpatient Clinic and in Long-Term Institutions
![]()
1School of Food Engineering, University of Campinas, Campinas, Brazil; 2School of Medical Sciences, University of Campinas, Cam-
pinas, Brazil; 3São Vicente de Paula Home, Atibaia, Brazil.
Email: *valcaselato@gmail.com
Received August 7th, 2011; revised September 21st, 2011; accepted October 12th, 2011.
Keywords: Aging, Malnutrition, Nutritional Status, Nutritional Assessment, Geriatric Assessment
ABSTRACT
Introduction: The Mini Nutritional Assessment (MNA) is a scale developed to evaluate the risk of malnutrition in senior citizens and to identify those who might benefit from early intervention. The objective of this study was to verify the nutritional profile of elderly individuals through the application of the MNA in three different locations: at the Geriatric outpatient clinic and two long-term institutions. Methods: Through transversal observation study the MNA was applied to 90 elderly people of both genders over 60 years of age. The MNA version modified by Rubenstein et al. [4] and translated into Portuguese was used to evaluate the patients for this study. The descriptive analysis of variables is shown as the average ± one standard deviation (SD). Results: At the AG, the risk of malnutrition was found to be 72.73% ± 3.77%, while 27.27% ± 3.77% of the patients were eutrophic; no malnourished elderly patients were found. At the ASVP, 15.38% ± 11.28% of elderly patients were found to be malnourished, 35.90% ± 15.10% were found to be at risk of malnutrition and 48.72% ± 15.72% were eutrophic. At the PMI, 42.50% ± 15.30% of the elderly patients were found to be malnourished, 25% ± 13.40% were at risk of malnutrition and 32.50% ± 14.50% were eutrophic. Conclusions: Due to the high prevalence of elderly patients that were malnourished or at risk of malnutrition, a more detailed evaluation of their nutritional states is required, as well as a regular follow up of those patients and a dietary intervention to reverse the situation.
1. Introduction
Malnutrition in elderly patients is common because daily food consumption decreases with old age. Furthermore, the consumed food is low in calories, contributing to nutritional deficiencies and malnutrition. The signs and symptoms of the aging process can be easily misinterpreted as malnutrition, and thus, the interventions are often inappropriate and less powerful than they could be.
The Mini Nutritional Assessment (MNA) scale was developed to diagnose the risk of malnutrition in elderly individuals. The objective of this scale is to provide a simple and quick evaluation of the nutritional state of elderly people who are in hospital, in geriatric institutions or in the community [1,2].
This scale represents a practical evaluation instrument; it is not invasive, and it takes into account the nutritional state, health conditions, frailty and eventual diseases of elderly individuals [3]. The simplified version of the MNA contemplates all of the items in the original version but is divided into two phases: the screening and the global evaluation phases. In the screening phase, the items are related to the original MNA version (changes in food ingestion, weight loss, decreased mobility, presence of psychological stress and acute diseases, presence of neuropsychological problems and body mass index), enabling patients to be diagnosed as either normal elderly people or as elderly people with the possibility of malnutrition. If the individual falls in the latter category, further evaluation is necessary [4].
In the MNA follow-up, there is a global assessment, in which parameters are established to identify the nutritional state more accurately. This phase includes questions about the place where the person lives, the number of medicines they take, any skin injuries or bed sores (decubitus ulcer), their eating habits, whether their eating habits are self-regulated, their self-perception of health and anthropometry (circumference of the arm and circumference of the calf) [2].
The MNA allows early nutritional risks and lower impact malnutrition to be identified, as some authors find that malnutrition can be difficult to distinguish from the effects of the natural aging process. If not detected, malnutrition can aggravate clinical conditions to which senior citizens are particularly susceptible and can also increase mortality [5,6].
The present study was conducted to establish the profiles of elderly people being assisted in geriatric outpatient clinics and in long-stay institutions and to apply the MAN for the selection of malnourished (or at risk of malnutrition) elderly, so that they could participate in a clinical trial for the evaluation of the effect of a developed dietary product. The research proposal was submitted and approved by the Committee for Ethics in Research of the Faculty of Medical Sciences of the State University of Campinas—Brazil, under approval number 451, on August 25th, 2005.
The objective of this study was to verify the nutritional profile of elderly individuals that were being taken care of at the geriatric outpatient clinic of UNICAMP (AG) and in long-term institutions (ASVP and PMI) through the application of the MNA.
2. Methods
Through a transversal observation study, elderly individuals of both genders over 60 years of age who were being assisted at the Geriatric Outpatient Clinic of the Clinical Hospital of UNICAMP in Campinas, SP, were assessed, along with all residents (39 elderly) at the São Vicente de Paula Home and all residents (40 elderly) at the Maria Imaculada Home, both situated in the municipality of Atibaia, Brazil.
The MNA version modified by Rubenstein et al. [4] and translated into Portuguese was used to evaluate the patients for this study. This version contains questions that are equal to the original version and includes two stages: screening and global evaluation. In the screening stage, the maximum score was 14 points, though scores equal to or greater than 12 indicated that the individual was eutrophic and was not required to go through a second stage of screening. Scores equal to or less than 11 indicated that the individual was at risk for malnutrition. At the end of the assessment, results showing less than 17 and 23.5 point indicated malnutrition and values between 17 and 23.5 points indicated a risk of malnutrition [1,4]. The selected elderly individuals were evaluated through the MNA according to the instructions in the MNA manual [7].
At the Geriatric outpatient clinic, the patients were interviewed to fulfill the MNA when they were in attendance with nutritionist. In the São Vicente de Paula Home and the Maria Imaculada Home, an MNA was conducted on all residents.
The MNA was conducted by the principal researcher. Some criteria were established for the interviews with the patients:
1) In the cases in which it was not possible to have an interview with the patient (e.g., patients who had cognitive problems), the interview was conducted with the patient’s caregiver, according to the methods of Vellas et al. 2 and Christensson et al. [8];
2) Those elderly people who were hospitalized or had lost a loved one in the last three months were considered to be under psychological stress, as in Beck et al. [5];
3) Neuropsychological problems were classified based on the subjective impression of the evaluator, as in Beck et al. [5];
4) Skin injuries or bedsores were evaluated by a visual inspection conducted by the researcher, as in Saletti et al. [9];
5) Only the elderly people who agreed to participate in the research after having the research explained to them and who signed the Free and Clarified Consent Term were included in this study. For those who showed a cognitive deficit, this procedure was conducted by the caretaker or the party responsible for the patient.
The anthropometric evaluation included measurements of weight and height to calculate the Body Mass Index (BMI), as well as measurements of the circumferences of the arm and calf.
The weight for all of the subjects was measured by the same person, and patients were required to stand barefoot, wearing minimal clothes while being weighed using the same calibrated WELMY brand mechanical scale platform (the scale had a capacity of 150 kg and an anthropometric ruler with a 2.00 m scale and divisions at 0.50 cm intervals). Similar models were used at the Geriatric outpatient clinic and at the São Vicente de Paula Home. At the Maria Imaculada Home, a TOLEDO brand electronic scale platform, with a 200 kg capacity, an anthropometric ruler with a 2.00 m scale and divisions every 0.50 cm, was used. The difference between the accepted measurements was, at the most, 400 g for an elderly person weighing up to 100 kg.
The heights of patients were measured using an anthropometric ruler coupled to the scales. The elderly individuals were instructed to stand erect against the support and facing forward (Frankfurt horizontal plane). The height could not be measured for some patients, and for these patients, height was estimated according to the equations proposed by Chumlea et al. [10]. BMI measured as weight (kg) divided by squared estimated height (m).
The arm circumference measurements were conducted with a flexible inextensible tape (TBW Importadora Ltda.). Patients were measured while standing up, with their trunk aligned with their legs and arms and their right arm outstretched. To determine the place where the tape should be fixed, an average point was marked between the acromion bone and the olecranon bone with the arm at a 90˚ angle. The difference between the resulting measurements was less than or equal to 0.5 cm.
The calf circumference was measured with a flexible inextensible tape (TBW Importadora Ltda.), with the patient in dorsal decubitus and the left leg forming a 90˚ angle with the knee, at the largest diameter of the calf, without compressing the calf. The accepted difference between measurements was less than or equal to 0.5 cm.
In the MNA statistical analysis, only three classes were considered: malnourished patients, patients at risk of malnutrition and eutrophic patients. The results were expressed as the average and percentages of patients in frequency tables.
The data were analyzed using the BioEstat 3.0 software [11]. The descriptive analysis of variables is shown as the average ± one standard deviation (SD). An analysis of variance with repeated measurements was used to explain the variation along the time. The significance of every effect in relation to the measurements, evaluated using the Tukey test, established that there was a difference between the groups.
3. Results
Eleven elderly individuals completed the Mini Nutritional Assessment at the Geriatric outpatient clinic of the HC Geriatric Outpatient clinic—UNICAMP. At the São Vicente de Paula Home and at the Maria Imaculada Home, the MNA was completed by, 39 and 40 elderly people, respectively, resulting in a total of 90 elderly people evaluated.
The stipulated quality criteria data and the data obtained in the evaluation were compiled, calculated as percentages and presented in Figure 1. Confidence intervals, at the 95% level, were used to make inferences about these results.
At the HC Geriatric Outpatient clinic—UNICAMP (AG), no malnourished elderly individuals were observed (0% ± 1.96%). On the other hand, a large number of patients were found to be at risk of malnutrition (72.73% ± 3.77%), and 27.27% ± 3.77% were found to be in a eutrophic state.
In the Maria Imaculada Home (PMI), the results showed that 42.50% ± 15.30% were in a state of malnutrition, 25% ± 13.40% were at risk of malnutrition and 32.50% ± 14.50% were in a eutrophic state.
A large percentage of malnourished elderly people were found in the PMI, while there were no undernourished people in the AG. However, the risk of malnutrition was found to be much greater in the AG than at the other institutions. The three institutions were found to have roughly similar proportions of patients in a eutrophic state.
4. Discussion
The nutritional state of the elderly is related to general health conditions. Nutritional diagnosis is important in this age bracket so that nutritional risk conditions in elderly people can be verified and therefore dietary interventions can be made.
The MNA is a nutritional evaluation instrument used in Europe and North America for frail, institutionalized or hospitalized, elderly people. When applied to communities in which malnutrition is prevalent, malnutrition was found to occur at rates of 0% - 6% in elderly people in the general community, 2% - 27% in institutionalized elderly people, and 10% - 30% in hospitalized elderly people [12]. The sensibility and specificity of the MNA is 96% and 98%, respectively [13-15]. In studies conducted in several countries on elderly people from different locations, the sensibility and the specificity of MNA have been compared to objective nutritional state evaluation methods, such as anthropometric, biochemical and dietary indicators[16,17]. These parameters have also been compared to nutritional screening methods and have been found to be in agreement with these results [2,8,9,18,19].
Some studies have found an association between a low MNA score and increased chances of disease [5], increased hospital mortality, increased number of nursing home institutionalizations and longer stays [20].
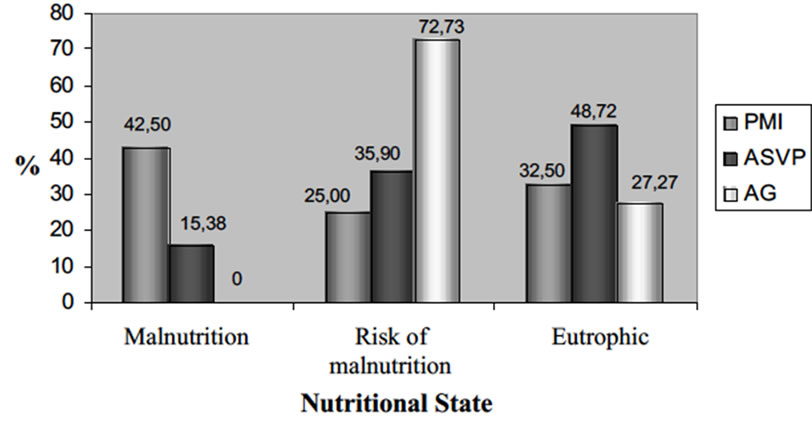
Figure 1. Comparison pf Mini Nutritional Assessment (MNA) among differents institutions evaluated.
The MNA possesses good clinical, biochemical and anthropometric correlation for patients that are found to be malnourished, but patients who are identified by the evaluation as being “at risk of malnutrition” could present normal biochemical and anthropometric exams. A low MNA score can be considered to be a predictor of frailty, which appears before the biochemical evaluation of serum albumin and measurements of weight and height to obtain the BMI [2,21]. Some authors suggest that MNA scores above 27 could be considered an indicator of successful aging [22].
In the Geriatric outpatient clinic, no malnourished elderly individuals were detected, but a high percentage of elderly were found to be at risk of malnutrition. A previous study done in Europe indicated that the risk of malnutrition for the elderly in the community is between 0% and 6% [23]. In the United Kingdom, 10% of elderly people living in the community were found to be malnourished, and this value can be higher depending on the geographical region evaluated [24].
Dalacorte et al. [17] compared the founding from the MNA with clinical, biochemical and anthropometric data from 42 elderly people living in the community of Ribeirão Preto, Brazil, and determined that 30.9% of the elderly were at risk of malnutrition. However, the MNA did not detect any malnourished elderly people, although three patients were diagnosed as malnourished condition according to biochemical and clinical evaluations.
The fact that no malnourished elderly people were detected in the Geriatric outpatient clinic through the MNA could be related to the fact that the sample was small and this instrument does not show a high specificity for the detection of malnutrition. However, the MNA can indicate a risk of malnutrition.
In long-term institutions, such as the São Vicente de Paula Home and the Maria Imaculada Home, the presence of malnourished elderly people and of those at risk of malnutrition was higher than at the other institution evaluated. In the São Vicente de Paula Home, the malnourished elderly people and those at risk for malnutrition constituted 15.38% and 35.9% of the total number of residents, respectively. In the Maria Imaculada, a high percentage of malnourished elderly women was observed (42.5%), and 25% of the patients were at risk for malnutrition.
These results are in agreement with the studies demonstrating that the prevalence of malnutrition is high in hospitalized or institutionalized elderly individuals, reaching rates of between 30% and 60% [25]. In a study conducted in Finland on 178 institutionalized elderly individuals, 3% were found to be malnourished, 48% were found to be at risk of malnutrition and 49% were eutrophic [26].
In the São Vicente de Paula Home, the results seemed to be similar to values reported in other studies; however, the results observed at the Maria Imaculada Home could be related to the presence of elderly women under exclusive enteral nutrition, as well as a high number of patients with Alzheimer’s disease. Weight loss is frequently observed in these individuals, and a decline in nutritional state can aggravate the disease. In a study of Alzheimer’s patients, the MNA was used to determine the evolution of the nutritional state in the elderly. The results found an association between weight loss in patients with a low MNA score and a low Mini-Mental score, and showed the worst results in anthropometric markers [27].
In the total sampling, a high prevalence of elderly patients were malnourished and at risk for malnutrition, reaching values of 61.11%, compared to 38.89% that were eutrophic. A longitudinal SENECA study, completed in Denmark, showed that the patients with a score of less than 23.5 showed increased mortality within a five year period after the study [23].
Felix and Souza [28] evaluated the nutritional risk of 37 elderly residents in a long-term institution in the Federal District using different nutritional evaluation instruments, including the MNA. Their results showed that 50.0% of the women and 40.0% of the men presented a risk of malnutrition.
In elderly patients that are in the malnourishment condition and at risk of malnutrition, it is important to conduct a periodic nutritional evaluation, including anthropometric, biochemical and dietary variables, to identify the appearance or worsening of a morbid state and to begin dietary intervention.
5. Conclusions
The MNA, a nutritional evaluation instrument for senior citizens who live in a community, are institutionalized, or are hospitalized. The early diagnosis of malnutrition is essential so that there is no difficulty in recovering the nutritional state that is found to be deficient.
Due to the high prevalence of elderly individuals that are malnourished and are at risk for malnutrition in long term institutions or in referral services for the elderly, it is necessary to have a more detailed evaluation of the nutritional state of those patients and more regular evaluations, in addition to dietary intervention to reverse the observed symptoms.
6. Acknowledgements
The authors are grateful to CNPq—National Council for Research and Development for the grant to author Valéria Maria Caselato de Sousa.
No conflict of interest declared concerning the publiccation of this article.
REFERENCES
- Y. Guigoz, B. Vellas and P. J. Garry, “Assessing the Nutritional Status of the Elderly: The Mini Nutritional Assessment as Part of the Geriatric Evaluation,” Nutrition Review, Vol. 54, 1996, pp. S59-S65. doi:10.1111/j.1753-4887.1996.tb03793.x
- B. Vellas, Y. Guigoz, P. J. Garry, F. Nourhashemi, S. Lauque and J. L. Albadere, “The Mini-Nutritional Assessment (MNA) and Its Use in Grading the Nutritional State of Elderly Patients,” Nutrition, Vol. 15, 1999, pp. 116- 122. doi:10.1016/S0899-9007(98)00171-3
- P. J. Garry and B. Vellas, “Practical and Validate Use of the Mini Nutritional Assessment in Geriatric Evaluation,” Nutrition Clinical Care, Vol.2, No. 30, 1999, pp. 146-154. doi:10.1046/j.1523-5408.1999.00108.x
- L. Z. Rubenstein, J. O. Harker, A. Salva, Y. Guigoz and B. Vellas, “Screening for Undernutrition in Geriatric Practice: Developing the Short-form Mini Nutritional Assessment (MNA-SF),” Journals of Gerontology Medical Sciences, Vol. 56, No. 6, 2001, pp. M366-M372. doi:10.1093/gerona/56.6.M366
- A. M. Beck and L. Ovesen, “At Which Body Index and Degree of Weight Loss Should Hospitalized Elderly Patients Be Considered at Nutritional Risk?” Clinical Nutrition, Vol. 17, 1998, pp.195-198. doi:10.1016/S0261-5614(98)80058-7
- G. S. Sacks, K. Dearman, W. H. Repoglie, V. L. Cora, M. Meeks and T. Canada, “Use of Subjective Global Assessment to Identify Nutrition-Associated Complications and Death in Geriatric Long-Term Care Facility Residents,” American College of Nutrition, Vol. 19, 2001, pp. 570-577.
- “A Guide to Completing the Mini Nutritional Assessment—MNA,” 2008. http://www.mna_elderly.com/ mna_guide.pdf
- L. Christensson, M. Unosson and A. C. Ek, “Evaluation of Nutritional Assessment Techniques in Elderly People Newly Admitted to Municipal Care,” European Journal of Clinical Nutrition, Vol. 56, 2002, pp. 810-818. doi:10.1038/sj.ejcn.1601394
- A. Saletti, E. Y. Lindgren, L. Johansson and T. Ceterholm, “Nutritional Status According to Mini Nutritional Assessment in an Institutionalized Elderly Population in Sweden,” Gerontology, Vol. 46, 2000, pp. 136-145. doi:10.1159/000022149
- W. C. Chumlea, A. F. Roche and M. L. Steinbaugh, “Estimating Stature from Knee Height for Persons 60 to 90 Year of Age,” Journal of American Geriatric Society, Vol. 33, No. 2, 1985, pp. 116-120.
- M. Ayres, M. Ayres Jr, D. M. Ayres and A. S. Santos “BioEstat 3.0: Aplicações Estatísticas nas Areas das Ciências Biológicas e Médicas,” Sociedade Civil Mamirauá, Belém, 2003.
- Y. Guigoz, B. Vellas and P. J. Garry, “Mini Nutritional Assessment: A Practical Assessment Tool for Grading Nutritional State of Elderly Patients,” Facts Research of Gerontology, Vol. 4, No. 2, 1994, pp. S15-S59.
- J. M. Bauer and C. C. Sieber, “Significance and Diagnosis of Malnutrition in the Elderly,” Zeitschrift Arztl Fortbild Qualitat, Vol. 101, No. 9, 2007, pp. 605-609.
- M. Cuyac Lantigua and S. Santana Porbán, “The Mini Nutritional Assessment of the Elderly in the Practice of a Hospital Geriatrics Service: Inception, Validation and Operational Characteristics,” Archivos Latinoamericanos de Nutricion, Vol. 54, No. 3, 2007, pp. 255-265.
- L. Ferreira, L. F. Nascimento and M. F. N. Marucci, “Use of the Mini Nutritional Assessment Tool in Elderly People from Long-Term Institutions of Southeast of Brazil,” Journal of Nutrition, Health and Aging, Vol. 12, No. 3, 2008, pp. 213-217. doi:10.1007/BF02982623
- Y. Guigoz, S. Lauque and B. J. Vellas, “Identifying the Elderly at Risk for Malnutrition the Mini Nutritional Assessment,” Clinocal Geriatric Medical, Vol. 18, 2002, pp. 737-757. doi:10.1016/S0749-0690(02)00059-9
- R. R. Dalacorte, J. C. Moriguti, F. D. Matos, J. S. Marchini and E. Ferriolli, “Mini-Nutritional Assessment Score and the Risk for Undernutrition in Free-Living Older Persons,” Journal of Nutrition, Health and Aging, Vol. 8, 2004, pp. 531-534.
- M. D. Persson, K. E. Brismar, K. S. Katzarski, J. Nordenström and T. E. Cederholm, “Nutritional Status Using Mini Nutritional Assessment and Subjective Global Assessment Predict Mortality in Geriatric Patients,” Journal of American Geriatrics Society, Vol. 50, No. 12, 2002, pp. 1996-2002. doi:10.1046/j.1532-5415.2002.50611.x
- L. Barone, B. Milosavljevic and B. Gazibarich, “Assessing the Older People: Is the MNA a More Appropriate Nutritional Assessment Tool than the SGA?” Journal of Nutrition, Health and Aging, Vol. 7, No. 1, 2003, pp. 13- 27.
- M. C. Van Nes, F. R. Herrmann, G. Gold, J. P. Michel and R. Rizzoli, “Does the Mini Nutritional Assessment Predict Hospitalization Outcomes in Older People?” Age in Aging, Vol. 30, 2001, pp. 221-226. doi:10.1093/ageing/30.3.221
- B. Vellas, Y. Guigoz, M. Baumgartner, P. J. Garry, S. Lauque and J. L. Albadere, “Relationships between Nutritional Markers and the Mini-Nutritional Assessment in 155 Older Persons,” American Geriatric Society, Vol. 48, 2000, pp. 1300-1309.
- K. Scheirlinckx, B. Vellas and P. J. Garry, “The MNA Score in People Who have Aged Successfully,” In: B. Vellas, P. J. Garry and Y. Guigoz, Eds., Nestle Nutrition Wokshop Series Clinical & Performance Programme, Nestec Ltd., Basel, 1999. p. 65-66.
- L. C. P. G. M. De Groot, A. M. Beck, M. Schroll and W. Van Staveren, “Evaluating the DETERMINE Your Nutritional Health Checklist and the Mini Nutritional Assessment as Tools to Identify Nutritional Problems in Elderly Europeans,” European Journal of Clinical Nutrition, Vol. 52, 1998, pp. 877-883. doi:10.1038/sj.ejcn.1600658
- B. M. Margetts, R. L. Thompson, M. Elia and A. A. Jackson, “Prevalence of Risk of Undernutrition is Associated with Poor Health Status in Older People in the UK,” European Journal of Clinical Nutrition, Vol. 57, No. 1, 2003, pp. 69-74. doi:10.1038/sj.ejcn.1601499
- B. Vellas, S. Lauque, S. Andrieu, F. Nourhashemi, Y. Roland, R. Baumgartner and P. J. Garry, “Nutrition Assessment in the Elderly,” Current Opinion in Clinical Nutrition and Metabolic Care, Vol. 4, No. 1, 2001, pp. 5-8. doi:10.1097/00075197-200101000-00002
- H. Soini, P. Routasalo and H. Langström, “Characteristics of the Mini-Nutritional Assessment in Elderly HomeCare patients,” European Journal of Clinical Nutrition, Vol. 58, 2004, pp. 64-70. doi:10.1038/sj.ejcn.1601748
- S. Gillette-Gyonnet, F. Nourhashémi, S. Andrieu, I. Glisezinski, P. J. Ousset, D. Rivière, J. L. Albarède and B. Vellas, “Weight Loss in Alzheimer Disease,” American Journal of Clinical Nutrition, Vol. 71, 2000, pp. 637S-642S.
- L. N. Felix and E. M. T. Souza, “Avaliação Nutricional de Idosos em uma Instituição por Diferentes Instrumentos,” Revista Nutrição, Vol. 22, No. 4, 2009, pp. 571-580.

