Open Journal of Anesthesiology
Vol.2 No.5(2012), Article ID:24822,4 pages DOI:10.4236/ojanes.2012.25054
Ultrasound-Guided Peri-Lymphatic and Peri-Neural Corticosteroid Injection as an Adjuvant to Pain and Lymphedema Management in Terminal Cancer: Two Case Reports
![]()
Department of Anesthesiology, Maimonides Medical Center, New York, USA.
Email: docrosenblum@gmail.com
Received August 27th, 2012; revised September 30th, 2012; accepted October 15th, 2012
Keywords: Corticosteroids; Adjuvant; Cancer Pain; Lymphedema; Peripheral Nerve Block
ABSTRACT
We are reporting two patients presented with intractable cancer pain that was treated with a novel application of an ultrasound-guided peripheral nerve block using corticosteroid. This technique offered relief to both patients whom otherwise their cancer pain was difficult to manage. The first patient developed lymphedema to the right axilla from metastatic squamous cell carcinoma. After multiple injections were deposited around the brachial plexus, lymphedema on the right axilla decreased slightly in size; however, range of motion improved post-procedure prior to his discharge one week later. In the second patient with left inguinal lymphadenopathy from metastatic left ureteral transitional cell carcinoma, there was a dramatic reduction in lymphedema in the left groin and leg as well as a considerable decrease in pain score during a two week follow-up after the peri-neural and peri-lymphatic femoral block. A 75% improvement in patient satisfaction was reported in the office visit’s questionnaire form. Corticosteroids can be used as an adjuvant to peripheral nerve block to decrease the pain secondary to lymphedema caused by the inflammatory response from metastatic cancer. This application can provide an alternative way to manage severe cancer-related pain caused by lymphedema in both upper and lower limbs.
1. Introduction
In the literature, corticosteroids have a wide range of therapeutic effect and usage including anti-inflammatory, immunosuppressive, antiemetic, and pharmacological treatment for endocrine, hematological, rheumatic, respiratory, and collagen diseases. In the treatment of chronic pain, others have advocated steroid injection for lower back pain, lumbosacral radiculopathy, and myofascial pain syndrome [1-3]. Experimental model in animal study has been investigated to describe the feasibility of corticosteroid in the blockade of pain transmission in nerve fibers [4]. Addition of corticosteroid to local anesthetic in some reports had resulted in prolonged duration of analgesia from axillary brachial plexus blocks [5,6]. In our two case reports, we have described the beneficial effect from corticosteroid injection in one patient suffering from intractable terminal metastatic cancer pain to the right axilla and the other patient complaining of pain to the left groin and leg swelling. After both patients received peri-neural and peri-lymphatic corticosteroid injections, they reported improved analgesia and lymphedema reduction.
2. Case Reports
2.1. Case 1
A 90-year-old Hispanic male with history of hypertension, stomach ulcer, and cardiac stent placement for coronary artery disease was admitted to the hospital for right upper extremity lymphedema, pain, motor and sensory impairment, and chronic skin changes. The patient was diagnosed with squamous cell carcinoma two years ago on the right dorsal hand which had metastasized to the right axillary lymph node. The patient remained asymptomatic until the right axillary mass enlarged in size. It was palpable, well circumscribed, and measured 4 cm × 4 cm in diameter under the right axilla buttressing against the chest wall. Physical examination of organ systems was unremarkable except weakness and mild sensory deficits which were noticed on the right extremeity. Strength was 4/5 on the right and 5/5 on the left upper extremity.
A computerized tomography (CT) scan showed no masses in other parts of the body. The mass was biopsied under CT-guided needle localization that correlated positive with the primary cancer. Due to the hypercoagulable state from the cancer, the patient was anticoagulated with warfarin (5 mg daily) for right axillary vein thrombosis. He had completed one round of palliative radiation therapy but the pain became so severe and unrelieved from oral oxycodone (2.5 mg to 5 mg every six hours) and hydromorphone (2 mg every 4 hours to 4 mg every eight hours), that it necessitated hospital admission from home.
Based on the physical findings and observations, we planned an ultrasound-guided right axillary peripheral nerve block (PNB). Warfarin was not discontinued before the procedure because of axillary vein thrombosis. The patient was brought into the block suite and positioned supine with the right arm externally rotated. Careful positioning of the patient was critical to avoid unnecessary pain and to obtain adequate exposure site for ultrasonography. The right axilla was prepped with chlorohexidine and draped in a sterile fashion. Standard American Society of Anesthesiologists (ASA) monitors were applied and sedation was not administered because of patient compliance.
A wide band 5 - 10 MHz transducer (LOGIQ e, GE Healthcare) was placed on the right axilla to locate the pulsation of the axillary artery. Anatomy of the neurovascular structures in our patient was challenging to delineate and optimal ultrasound imaging was limited not only to tissue swelling and lymphadenopathy surrounding the axillary nerve bundle, but also to structural distortion from radiation therapy that he received several months before admission (Figure 1). Once the nerves were visualized, a 100-mm 22-gauge needle (Stimuplex® A, B. Braun Medical Inc., Bethlehem, PA) with a total of 40 ml of 0.25% ropivacaine (Naropin®, APP Pharmaceuticals, Schaumburg, IL) mixed with 80 mg methylprednisolone acetate (Depo-Medrol®, Pharmacia-Upjohn, Kalamazoo, MI) was injected around the brachial plexus bundle and peri-lymphatic area. Negative aspiration of blood or cerebrospinal fluid was obtained from the Stimuplex® needle before each injection.
In the postoperative period, the patient reported some degree of paresthesia on the right extremity after 30 minutes of injection. No visible signs of hematoma or bleeding were noticed at the site of puncture. Distal pulse was palpable. During the next five days at the hospital, he was followed-up by the palliative team as well as from the pain management service. Upon discharge, his pain and lymphedema were well controlled. Improved range of motion from the right shoulder was noticed. During a phone interview follow-up several months later, the pa-
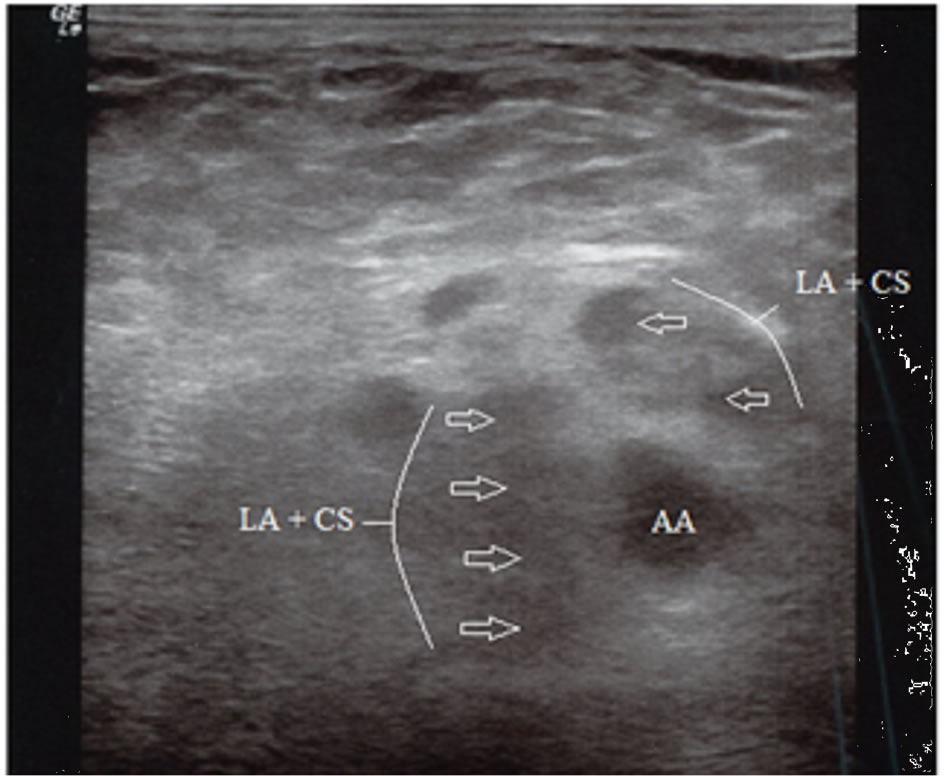
Figure 1. Ultrasound image of the axillary brachial plexus block. Note the tissue distortion from the lymphedema and inflammation. Spread of the local anesthetic and corticosteroid is seen circumscribing the axillary artery. (AA = axillary artery, LA = local anesthetic, CS = corticosteroid).
tient admitted to a decrease in oral opioid consumption. Currently he is taking oral morphine (15 mg twice daily) as needed for his pain and his right axilla has not increased in size; however, tactile sensation and strength have diminished.
2.2. Case 2
A 70-year-old male with history of well-controlled hypertension, spine and gastric surgeries, and metastatic transitional cell carcinoma was referred to the pain office by an urologist for left-sided lower back pain and left groin lymphedema that caused his leg to swell to two to three times the size for the past two months. The patient was diagnosed with primary left ureteral transitional cell carcinoma ten years ago and underwent a left nephrectomy. His cancer was in remission until he presented with a dull, sharp, and constant left groin pain that started in the back and was not relieved with oral opiates. The pain was exacerbated in the sitting position but hot towels to the left groin provided some relief.
Physical examination showed negative Patrick’s test and straight leg test on the right lower extremity; however, exam was unobtainable on the left extremity due to limited range of motion and groin swelling. Visible lymphadenopathy was seen on the left inguinal region and was tender to touch but not erythematous or warm. Lumbar paraspinal muscle tenderness was more on the left lower back than the right. Examination of the sacroiliac joints and palpation of the left psoas muscle were within normal limits. Motor strength was 5/5 on his limbs bilaterally with intact sensation.
A venous Doppler of the left lower extremity showed no deep vein thrombosis. Magnetic resonance imaging (MRI) of the spine showed suspicious metastatic disease affecting the lumbosacral spine, specifically a lesion on the left side of the L4 vertebral body and retroperitoneal lymphadenopathy. A regional femoral nerve block and trigger point injection were planned as well as recommendation for physical therapy and oral gabapentin (300 mg every eight hours) after the procedure.
Patient was prepped and draped in sterile fashion lying supine with the left knee extended and thigh externally rotated while standard ASA monitors were applied prior to the block. Intravenous 2 mg midazolam and 50 mcg fentanyl were administered for sedation. The equipment used was same as described in case 1. Similar to the first patient, tissue distortion and lymphedema around the femoral neurovascular bundle was challenging to visualize. Approximately 10 ml of 0.1% ropivacaine and 20 mg triamcinolone acetonide (Kenalog®, Bristol-Myers Squibb, Princeton, NJ) was deposited around the peri-lymphatic space where it was believed to cause the leg swelling and pain (Figure 2). The needle was then directed toward the fascia iliaca compartment until two pops were felt and an additional 5 ml injectate was deposited around the femoral nerve bundle. Trigger point injections of approximately 20 ml of 0.2% ropivacaine and 40 mg triamcinolone acetonide were infiltrated into the left gluteal and piriformis muscles for spasm. The patient tolerated the procedure well without any complications. During a twoweek follow-up in the office, the patient reported a 75% decrease in pain symptomology as compared to the last visit. Additionally, the swelling in the left leg resolved.
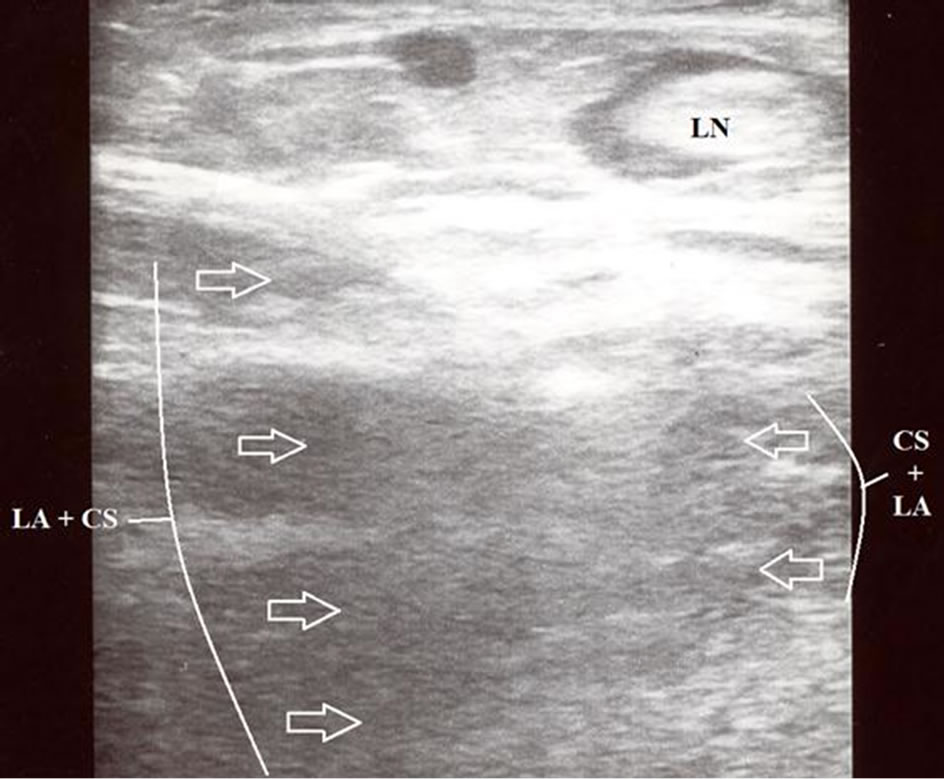
Figure 2. Ultrasound image of the femoral peri-lymphatic space. Note the spread of local anesthetic and corticosteroid in the peri-lymphatic space. (LN = lymph node, LA = local anesthetic, CS = corticosteroid).
3. Discussion
Corticosteroids have many undesirable side effects that include uncontrolled hyperglycemia in diabetes mellitus, Cushingoid symptoms, osteoporosis, severe hypertension, psychiatric disturbances, and dermatological changes. Methylprednisolone acetate and triamcinolone acetonide are synthetic corticosteroids that are five times more potent than hydrocortisone. They are widely used in interventional pain medicine as anti-inflammatory agents and adjuvants to bridge the gap of inadequate analgesia while offering minimal neurotoxicity in the epidural space and peripheral nerve [7,8].
Managing cancer pain in terminally ill patients can be complex. It is important to realize the proper risk benefit analysis be undertaken since life expectancy is short. Another consideration is to address the type of pain intervention that the patient will receive and whether the regimen will control their pain. Continuous PNB has been devised to treat patients with terminal cancer pain when unwanted side effects from opioid usage prove to be unfavorable for end-of-life care [9].
The first patient had a right axillary deep vein thrombosis requiring continuous full anticoagulation with warfarin therapy. In rare instances, a hematoma can occur during an axillary brachial plexus block resulting in untoward peripheral nerve sequelae even in otherwise healthy patient not receiving anticoagulation therapy [10]. Although vascular damage could occur from the PNB, an experienced and trained anesthesiologist using a thinner infiltrative needle and higher resolution ultrasound can reduce the risk of hematoma [11]. Continuous PNB was not an option in this patient since there was a potential of significant bleeding and formation of an axillary hematoma. Additionally, in both patients, the introduction of a catheter within the peri-neural sheath would be especially difficult because of their distortion and gross distension of the anatomy caused by venous congestion and lymphedema.
The main disadvantage of a single-injection PNB is the inability to deliver a continuous amount of analgesia for an extended duration for pain control [12]. However, due to additional risk and the diminished possibility of success coupled with the increased risk of infection in these patients (first patient was bedridden and wheel chair bound), a continuous PNB was an undesirable choice.
Effective pain control after the PNB was not immediately expected in either patient since we anticipated that they will have continuous swelling over the course of next week as the anti-inflammatory properties of corticosteroid takes at least 5 to 7 days to work. Their breakthrough pain was addressed post-procedurally. The first patient pain was controlled with intravenous hydromorphone (0.7 mg every four hours) supplemented with gabapentin (100 mg every eight hours) whereas the second patient had a remarkable recovery from lymphedema in the left leg within several weeks that required less oral pain medications. Eventually, a fentanyl patch (25 mcg per hour) was prescribed for the second patient back pain that extended to his buttocks that was not relieved by trigger point injections.
The two case reports demonstrate a plausible utility of corticosteroid not only as an anti-inflammatory agent in treating arthritic joint diseases in chronic pain but also in curbing the biological response that vascular tissues suffered from harmful mediators in cancer pain. Although it is intuitive to assume the steroid effect to be beneficial in healthy patients, this is still unknown especially in patients with history of co-morbidities [13]. The applicability of this finding must be verified by evidence-based medicine.
4. Acknowledgements
The authors would like to thank Dennis E. Feierman, MD, PhD (Vice-Chairman, Department of Anesthesiology, Maimonides Medical Center) for his editorial assistance with the manuscript.
REFERENCES
- J. Mobaleghi, F. Allahdini, K. Nasseri, B. Ahsan, S. Shami, M. Faizi and F. Gharibi, “Comparing the Effects of Epidural Methylprednisolone Acetate Injected in Patients with Pain Due to Lumbar Spinal Stenosis or Herniated Disks: A Prospective Study,” International Journal of General Medicine, Vol. 4, 2011, pp. 875-878.
- C. Roy, N. Chatterjee, S. N. Patro, A. Chakraborty, G. R. V. Kumar and R. Sengupta, “The Efficacy of Transforaminal Epidural Steroid Injections in Lumbosacral Radiculopathy,” Neurology India, Vol. 59, No. 5, 2011, pp. 685-689. doi:10.4103/0028-3886.86541
- A. V. Rde, F. G. Alencar and C. Zamperini, “Different Substances and Dry-Needling Injections in Patients with Myofascial Pain and Headaches,” Cranio, Vol. 26, No. 2, 2008, pp. 96-103.
- A. Johansson, J. Hao and B. Sjolund, “Local Corticosteroid Applications Blocks Transmission in Normal Nociceptive C-Fibres,” Acta Anaesthesiologica Scandinavica, Vol. 34, No. 5, 1990, pp. 335-338. doi:10.1111/j.1399-6576.1990.tb03097.x
- A. Movafegh, M. Razazian, F. Hajimaohamadi and A. Meysamie, “Dexamethasone Added to Lidocaine Prolongs Axillary Brachial Plexus Blockade,” Anesthesia & Analgesia, Vol. 102, No. 1, 2006, pp. 263-267. doi:10.1213/01.ane.0000189055.06729.0a
- T. Stan, E. J. Goodman, C. Bravo-Fernandez and C. R. Holbrook, “Adding Methylprednisolone to Local Anesthetic Increases the Duration of Axillary Block,” Regional Anesthesia and Pain Medicine, Vol. 29, No. 4, 2004, pp. 380-381.
- R. S. Cicala, R. Turner, E. Moran, R. Henley, R. Wong and J. Evans, “Methylprednisolone Acetate Does Not Cause Inflammatory Changes in the Epidural Space,” Anesthesiology, Vol. 72, No. 3, 1990, pp. 556-558. doi:10.1097/00000542-199003000-00026
- S. E. Mackinnon, A. R. Hudson, F. Gentili, D. G. Kline and D. Hunter, “Peripheral Nerve Injection Injury with Steroid Agents,” Plastic and Reconstructive Surgery, Vol. 69, No. 3, 1982, pp. 482-490. doi:10.1097/00006534-198203000-00014
- A. T. Esch, A. Esch, J. L. Knorr and A. P. Boezaart, “Long-Term Ambulatory Continuous Nerve Blocks for Terminally Ill Patients: A Case Series,” Pain Medicine, Vol. 11, No. 8, 2010, pp. 1299-1302. doi:10.1111/j.1526-4637.2010.00900.x
- B. Ben-David and S. Stahl, “Axillary Block Complicated by Hematoma and Radial Nerve Injury,” Regional Anesthesia and Pain Medicine, Vol. 24, No. 3, 1999, pp. 264- 266. doi:10.1097/00115550-199924030-00016
- L. H. Ferraro, M. A. Tardelli, A. M. Yamashita, J. D. Cardone and J. M. Kishi, “Ultrasound-Guided Femoral and Sciatic Nerve Blocks in an Anticoagulated Patient. Case Reports,” Revista Brasileira de Anestesiologia, Vol. 60, No. 4, 2010, pp. 422-428.
- H. B. Fischer, T. M. Peters, I. M. Fleming and T. A. Else, “Peripheral Nerve Catheterization in the Management of Terminal Cancer Pain,” Regional Anesthesia, Vol. 21, No. 5, 1996, pp. 482-485.
- B. A. Williams, B. B. Murinson, B. R. Grable and S. L. Orebaugh, “Future Considerations for Pharmacologic Adjuvants in Single-Injection Peripheral Nerve Blocks for Patients with Diabetes Mellitus,” Regional Anesthesia and Pain Medicine, Vol. 34, No. 5, 2009, pp. 445-457. doi:10.1097/AAP.0b013e3181ac9e42

