Open Journal of Gastroenterology
Vol.3 No.2(2013), Article ID:32207,4 pages DOI:10.4236/ojgas.2013.32023
Is there a correlation between endoscopy and imaging findings in Crohn’s disease?*
![]()
1Department of Hepatology and Gastroenterology, Hassan II University Hospital, Fez, Morocco
2Department of Radiology, Hassan II University Hospital, Fez, Morocco
3Department of Epidemiology, Hassan II University Hospital, Fez, Morocco
Email: #charifiliass82@hotmail.com
Copyright © 2013 I. Charif et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 11 February 2013; revised 25 March 2013; accepted 1 May 2013
Keywords: Crohn’s Disease; Imaging; Endoscopy; Correlation
ABSTRACT
Background and Aims: Crohn’s disease is a chronic inflammatory bowel disease (IBD). Endoscopy and radiology play an important role in the diagnosis and management of this specific disease. The ability of each of these two tests to detect the gastrointestinal involvement (ulceration, stenosis, fistula, polyp, mucosal thickening) varies according to the type of Crohn’s lesions. The purpose of our study was to evaluate the correlation between these two diagnostic methods in the detection of those specific lesions in 70 patients diagnosed with Crohn’s Disease (CD) during the period of 3 years. Methods: In this retrospective study, including 70 patients with Crohn’s disease, Four major characteristic lesions (ulceration, stenosis, fistula and polyps) were studied by endoscopy and radiological exams to evaluate the relationship between endoscopy and imaging findings in the detection of these lesions. The analysis of our results was made by statistical analysis system: EpiInfo and SPSS. Results: The concordance of each of these diagnostic modalities is average for stenosis and fistulas and low diagnostic significance for ulcers and polyps. However, the imaging features of mucosal thickening are sensitive but not specific.
1. INTRODUCTION
The inflammatory bowel disease (IBD) is a recurrent acute and chronic disorder, characterized by extensive inflammatory lesions of the intestinal wall. This complex disease also called multifactorial and polygenic disorders [1].
Crohn’s disease (CD) is characterized by intermittent areas and discontinuous transmural digestive tract inflammation (skip areas), which can affect all segments of the gastrointestinal tract from the mouth to the anus but most commonly in ileal, colonic, and anal regions.
Initially, this inflammation can manifest by superficial lesions which progress over time and can lead to the development of stenotic complications and fistulas. Their consequences have been observed in approximately two thirds of patients after 10 years of evolution [2,3].
Evaluation of the small bowel and colon lesions in Crohn’s disease is essential in managing these disorders. Endoscopy can be useful to evaluate the severity and extension of the disease, to assess treatment effectiveness and to detect dysplasia and cancerous changes [4,5].
Colonoscopy remains the gold standard for the assessment of superficial lesions of the terminal ileum and the colon and much progress has been made in the imaging field.
The aim of our study was to investigate the relationship between the data of endoscopy and the imaging findings in the detection of endoscopic and radiological signs of Crohn’s disease (ulceration, stenosis, fistula, mucosal thickening and polyp).
2. MATERIALS AND METHODS
The study was observational, monocentric and retrospective, including 70 patients who were admitted in our university hospital and underwent endoscopy and further imaging: CT enterography or MR enterography or small bowel series or just abdominal ultrasound. The indications of these imaging tests were different according to the clinical context. Those diagnostic tests have been done as part of initial diagnosis or follow-up. The diagnosis of Crohn’s disease was made based on a combination of clinical, biological, endoscopic, radiological and histological features. All these cases were diagnosed from January 2009 to April 2012 in University Hospital Center (FES, MOROCCO). Data collection is made from the patient records. We excluded patients who have not undergone an imaging or endoscopic examination, or patients in whom the diagnosis of Crohn’s disease was reviewed because of the appearance of new data allowing to exclude this disease.
The analysis of our results was made by statistical analysis system: EpiInfo and SPSS.
Four major characteristic lesions (ulceration, stenosis, fistula and polyps) were studied by endoscopy and radiological exams to evaluate the relationship between endoscopy and imaging findings in the detection of these lesions. Bowel wall thickening is the sign most frequently found in the imaging, which prompted us to study the endoscopic lesions that correspond.
The comparative study of these endoscopic and radiological lesions was made by studying the kappa scores by using the SPSS system. The interpretation of our results was as follows: good if Kappa concordance >0.6, bad if <0.3 and intermediate if Kappa values between the two scores.
Although the importance of this study, it was limited by the lack of data concerning sensitivity and specificity of each imaging test for revealing the lesions studied compared to the endoscopic findings. These sensitivities and specificities are very different according to the type of imaging.
3. RESULTS
3.1. Patients General Data
The average age of our patients was 36.2 +/− 15. The sex ratio was 1.12 (male/female). Two of our patients (2.8%) had a previous history of appendicitis and appendectomy, five (7.1%) had arthritis, two (2.8%) had a Crohn family history and 16 patients (22.8%) were chronic smokers.
Abdominal pain was present in 60 patients (87.0%), chronic diarrhea in 55 cases (78.6%). Rectal bleeding was found in 25 patients (35.7% of cases). 12 patients (17.1% of cases) had Koenig syndrome and 28 patients (40% of cases) had a rectal or dysenteric syndrome.
Biological tests showed an inflammatory syndrome in 45 patients: leukocytosis, increased CRP and/or ESR (erythrocyte sedimentation rate).
3.2. Endoscopic Lesions Found in Our Patients
Four major lesions were studied: ulcers, stenosis, fistulas and polyps. Ulcers were present in 50 patients (71.4%). Stenosis in 23 patients (32.9%). Fistulas were found in 3 patients (4.3%), and polyps were found in 15 patients (21.4%).
3.3. Radiological Lesions Observed in Our Series
Ulcerations were found in 13 patients (18.6%). Fistula in 10 cases (14.3%). Stenoses were observed in 13 patients (18.6%) and polyps were not highlighted by imaging exams. In addition, digestive wall thickening was present in 39 patients (55.7%).
3.4. Study of the Correlation between Endoscopy and Imaging Findings of Crohn’s Disease Lesions
The study of the previous lesions, mentioned above, were found in endoscopy and radiology, allowed us to study the correlation between these two diagnostic tools for highlighting these Crohn lesions.
The comparative study of each lesion found by endoscopy and radiological exploration (Figure 1) showed a kappa of 0.01 for ulcerations. For stenosis and fistulae, the concordance correlation Kappa was 0.56 and 0.42. Moreover, it was impossible to find any relationship between endoscopy and imaging findings for polyps observed in radiology.
4. DISCUSSION
The Crohn’s disease and the ulcerative colitis are the two major forms of chronic Inflammatory bowel disease (IBD) [6,7]. The diagnosis of Crohn’s disease is established by acombination of clinical presentation, endoscopic appearance, radiology, histology, and, more recently, serology and genetics [6]. All patients included in this study, fulfilled these diagnostic criteria.
Most of our patients were young, which is consistent and coherent with several epidemiological studies [8,9]. In contrast with the literature, where a majority of studies report a female predominance, in our patients a discrete male predominance was noted.
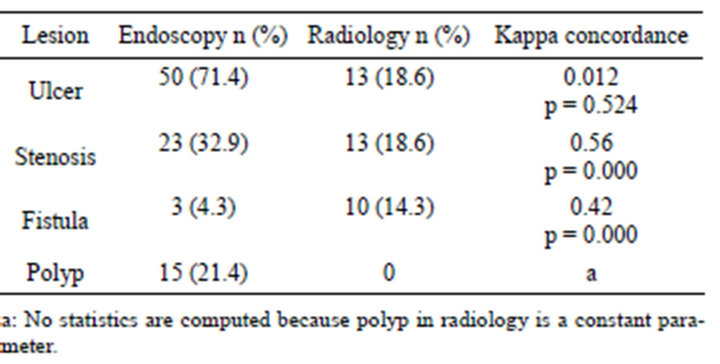
Figure 1. Concordance between various lesions found in endoscopy and radiology estimated by kappa.
With the recent advances in endoscopic techniques and radiology imaging, considerable progress has been made in the diagnosis of Crohn’s disease, that not only look to confirm the diagnosis but also to monitor and detect suspicious lesions [6,10-12].
Most studies [13-21] have evaluated the contribution of radiology or endoscopy in the diagnosis of Crohn’s disease. However, our study has focused on the comparative study of the ability of each of these two diagnostic methods for the detection of lesions suggestive of Crohn’s disease.
In the CD, endoscopy guide the diagnosis, assess the disease activity, and avoid surgery through endoscopic management and long-term follow up of lesions [22,23]. In our series, endoscopy has done for diagnosis but it has also been proposed as a monitoring and a screening tool for complications.
The four lesions studied (including ulceration and pseudopolyps or polyps as a specific anatomic lesion; and stenosis and fistulae as complications) were found with different frequencies, reflecting the high prevalence of complications during the CD. Ulcerations were the most common lesions followed by polyps, stenosis and fistulas.
Today radiology plays also an important role in the diagnostic of the CD. Multi-technique imaging approaches have been developed to explore all radiologic features of gastrointestinal tract lesions.
The development of immune-modulating biologic agents creates a need for the increasing availability and use of advanced imaging methods to identify the degree of disease activity, to look for early complications such fistulae, to choose the most appropriate therapy and to reduce the complication rate [24].
The sensitivity of detection and characterization of the different lesions differs from one technique to the other. The radiological study of various lesions has shown a high frequency of ulceration and stenosis followed by fistulas. However, the sensitivity of the imaging technique for detecting fistula is much more important than endoscopy.
In our patients, the comparative study of the sensitivity of each diagnostic method of CD (endoscopy and imaging) showed that the concordance of these two diagnostic tools varies depending on the lesion studied.
Endoscopy for ulceration is much more sensitive than imaging with a mismatch in favor of endoscopy (Kappa: 0.012 and p: 0524). This could be explained by the mode that ulcers are superficial lesions and the capability of the imaging method for detecting the mucosal lesions (ulcers and earlier damage) is generally low [25]. However, this concordance rate is average when it concerns the study of stenosis and fistulas (Kappa 0.56 and 0.42 with p = 0.000 for both lesions). This is due to the fact that these two lesions infiltrate the intestinal wall through the different layers: mucosa, submucosa, muscular layer and serosa (causing fistula) and extend intra luminally, destroying parietal folds (causing luminal stenosis), that allow them to be better detected by both endoscopy and imaging. Polyps and pseudo-polyps are significant lesions in the CD, although endoscopy is the most sensitive diagnostic method for detection.
In our study, the imaging has revealed a failure to detect polyps found endoscopically, with an impossible concordance to specify. In addition, the bowel wall thickening is the most common radiological sign found, but less sensitive because it can be associated with various lesions mentioned above.
5. CONCLUSION
The diagnosis of Crohn’s disease is sometimes difficult. Endoscopy and imaging are two main pillars that complemented information for the diagnosis. Neither of these two methods alone can identify the different components of this inflammatory disease. The concordance of each of these diagnostic methods is average for stenoses and fistulas but low for ulcers and polyps. However, the radiological sign of bowel wall thickening is sensitive but not specific.
6. ACKNOWLEDGEMENTS
All authors have made significant contributions to the work presented in this paper. IC and ME carried out the study, collected and analyzed the data and drafted the manuscript, MA, DB and AI took part in the planning and designing of the study and revised the draft of the manuscript. OA has revised the English language to the manuscript. IK and ST have revised the imaging data. AB and CN carried out the statistical analysis.
REFERENCES
- Louis, E., Belaiche, J. and Reenaers, C. (2010) Nouveautés dans la stratégiethérapeutique des maladies inflammatoires chroniques de l’intestin. Journées Françaises d’Hé- patologie et d’Oncologie Digestive.
- Louis, E., Collard, A., Oger, A.F., Degroote, E., El Yafi, F. and Belaiche, J. (2001) Behaviour of Crohn’s disease according to the Vienna classification: Changing pattern over the course of the disease. Gut, 49, 777-782. doi:10.1136/gut.49.6.777
- Cosnes, J., Cattan, S., Blain, A., et al. (2002) Long term evolution of disease behavior of Crohn’s disease. Inflammatory Bowel Diseases, 8, 244-250. doi:10.1097/00054725-200207000-00002
- Bouhnic, Y. (2007) Endoscopie interventionnelle et MICI. Journées Françaises d’Hépatologie et d’Oncologie Digestive.
- Leighton, J.A., Shen, B., Baron, T.H., et al. (2006) ASGE guideline: Endoscopy in the diagnosis and treatment of inflammatory bowel disease. Gastrointestinal Endoscopy, 63, 558-565. doi:10.1016/j.gie.2006.02.005
- Nikolaus, S. and Schreiber, S. (2007)Diagnostics of inflammatory bowel disease. Gastroenterology, 133, 1670- 1689. doi:10.1053/j.gastro.2007.09.001
- Neumann, H., Mönkemüller, K., Günther, C., Atreya, R., Vieth, M. and Neurath, M.F. (2012) Advanced endoscopic imaging for diagnosis of Crohn’s disease. Gastroenterology Research and Practice, 2012, 8 p.
- Vernier, G., Cortot, A., Gower-Rousseau, C., Salomez, J.L. and Colombel, J.F. (2005) Epidemiologie et facteurs de risques au cours des MICI. Revue du Praticien, 55, 949-961.
- Loftus, E.V. (2004) Clinical epidemiology of inflammatory bowel diseases: Incidence, prevalence, and environmental influences. Gatsroenterology, 126, 1507-1517.
- Mary, J.Y., Lémann, M., Colombel, J.F., Lerebours, E., Soulé, J.C., Gendre, J.P. and Modigliani, R. (The GETAID) Endoscopic remission and response in Crohn’s disease an objective definition using the CDEIS. Gut, 54, A54.
- Rutgeerts, P., Colombel, J.F., van Deventer, S., Vatn, M., Loftberg, R., Schreiber, S., Campieri, M., Malchow, H., Scholmerich, J., Cornillie, F., Olson, A., Bao, W., Katz, S. and Lochs, H. (2002) Endoscopic healing induced by infliximab maintenance therapy correlates with long-term clinical response in patients with active Crohn’s disease. Results of endoscopic substudy of accent I. American Journal of Gastroenterology, 97, S260. doi:10.1016/S0002-9270(02)05275-9
- Friedman, S., Rubin, P.H., Bodian, C., Goldstein, E., Harpaz, N. and Present, D.H. (2001) Screening and surveillance colonoscopy in chronic Crohn’s colitis. Gastroenterology, 120, 820-826. doi:10.1053/gast.2001.22449
- Neumann, H., Neurath, M.F. and Mudter, J. (2011) New endoscopic approaches in IBD. World Journal of Gastroenterology, 17, 63-68. doi:10.3748/wjg.v17.i1.63
- Lemann, M. and Pariente, B. (2008) Intérêt de l’imagerie radiologique et endoscopique dans le suivi des MICI. Journées Françaises d’Hépatologie et d’Oncologie Digestive.
- Kwon, R.S., Sahani, D.V. and Brugge, W.R. (2005) Gastrointestinal cancer imaging: Deeper than the eye can see. Gastroenterology, 128, 1538-1553. doi:10.1053/j.gastro.2005.03.034
- Mako, E.K., Mester, A.R., Tarjan, A., et al. (2000) Enteroclysis and spiral CT examination in diagnosis and evaluation of small bowel Crohn disease. European Journal of Radiology, 35, 168-175. doi:10.1016/S0720-048X(00)00239-4
- Mazzeo, S., Caramella, D., Battolla, L., et al. (2001) Crohn disease of the small bowel: Spiral CT evaluation after oral hyperhydration with iosotonic solution. Journal of Computer Assisted Tomography, 24, 612-616. doi:10.1097/00004728-200107000-00017
- Lee, S.S., Kim, A.Y., Yang, S.K., et al. (2009) Crohn disease of the small bowel: Comparison of CT enterography, MR enterography, and small-bowel follow through as diagnostic techniques. Radiology, 251, 751-761. doi:10.1148/radiol.2513081184
- Siddiki, H.A., Fidler, J.L., Fletcher, J.G., et al. (2009) Prospective comparison of state-of the-art MR enterography and CT enterography in smallbowel Crohn’s disease. American Journal of Roentgenology, 193, 113-121. doi:10.2214/AJR.08.2027
- Pera, A., Bellando, P., Caldera, D., Ponti, V., Astegiano, M., Barletti, C., David, E., Arrigoni, A., Rocca, G. and Verme, G. (1987) Colonoscopy in inflammatory bowel disease. Diagnostic accuracy and proposal of an endoscopic score. Gastroenterology, 92, 181-185.
- Witte, A.M., Veenendaal, R.A., Van Hogezand, R.A., Verspaget, H.W. and Lamers, C.B. (1998) Crohn’s disease of the upper gastrointestinal tract: The value of endoscopic examination. Scandinavian Journal of Gastroenterology, 225, 100-105.
- Hamilton, M.J. (2012) The valuable role of endoscopy in inflammatory bowel disease. Diagnostic and Therapeutic Endoscopy, 2012, Article ID: 467979.
- Hommes, D.W. and Van Deventer, S.J.H. (2004) Endoscopy in inflammatory bowel diseases. Gastroenterology, 126, 1561-1573. doi:10.1053/j.gastro.2004.03.023
- Fletcher, J.G., Fidler, J.L., Bruining, D.H. and Huprich, J.E. (2011) New concepts in intestinal imaging for inflammatory bowel diseases. Gastroenterology, 140, 1795- 1806. doi:10.1053/j.gastro.2011.02.013
- Oudjit, A., et al. (2005) Imagerie de la maladie de Crohn. Elsevier SAS, Paris.
NOTES
*The authors have no conflict of interest. The authors alone are responsible for the content and writing of the manuscript.
#Corresponding author.

