Open Journal of Pediatrics
Vol. 2 No. 2 (2012) , Article ID: 19868 , 11 pages DOI:10.4236/ojped.2012.22025
Mealtime feeding behaviors and gastrointestinal dysfunction in children with classic autism compared with normal sibling controls
![]()
Department of Pediatrics, Inova Fairfax Hospital for Children, Falls Church, USA
Email: *Rhs738@aol.com
Received 1 December 2011; revised 2 March 2012; accepted 20 March s2012
Keywords: Classic Autism; Feeding Behaviors; GI Dysfunction
ABSTRACT
Introduction: We compared the frequency and duration of specific mealtime behaviors and GI dysfunction in children with classic autism to typically-developing siblings. Survey Method: A 41-item on-line parent survey. Statistics: Chi square and binomial logistical regression. Results: 79 children with classic autism matched with a normally-developing sibling. Logistic Regression Analysis Revealed: Dislike of new foods and bizarre mealtime mannerisms, were more frequent in those with classic autism (p < 0.01). They also had higher odds ratio of constipation and fecal incontinence (p < 0.01). 40% of children with classic autism had been on GFCF diets (p < 0.01). Only 1% of those children on a gluten-free diet had a biopsy-proven diagnosis of celiac disease. Conclusion: Children with classic autism had more frequent dislike of new foods, bizarre mealtime behaviors, constipation, and fecal incontinence.
1. INTRODUCTION
Autistic spectrum disorder (ASD) is a group of neurodevelopmental disorders that includes three major subgroups: Asperger syndrome, pervasive developmental disordernot otherwise specified (PDD-NOS) which is the most common and has the least precise diagnostic criteria, and, classical autism [1,2]. It is estimated that 1 in 110 children in the U. S. and Canada has a diagnosis of ASD [3].
Although opinions differ, a majority of published studies on the subject of childhood autism and gastrointestinal problems report higher rates of feeding problems and GI dysfunction in children with ASD [4-13]. A recent study comparing 48 children (3 to 12 years old) with ASD, to their matched siblings found that the ASD group had a mean of 13 eating problems, with lack of food variety predomination while the sibling group had a mean of 5 eating problems [11]. Older children tended to have fewer problems than younger children.
Feeding problems include selective food avoidance behaviors and idiosyncratic and entrenched food preferences (selective eating) based on food texture, color, smell, and presentation. These problems, if unchecked in children with ASD, sometimes lead to unbalanced diets, dietary deficiencies, poor weight gain, and inferquently, failure to thrive [6]. The Brief Autism Mealtime Behavior Inventory (BAMBI) [14] and the Screening Tool of Feeding Problems applied to children (STEP-CHILD) [15] were designed to measure mealtime behavior problems observed in children.
GI dysfunction disorders include dysphagia, gastrointestinal reflux (GER), constipation, withholding stool, and fecal incontinence [9]
In 2011, investigators from the University of California in Sacramento and Los Angeles reported that 249 children on the autism spectrum had significantly more GI problems (42%) than 163 siblings 12%). This study was registry-based and the investigators conducted inhome structured medical history interviews by parent recall. Those children with classic autism had increased odds of having GI problems compared to less severely affected children with ASD [12].
Only a few studies provided important semi-quantitative data on the duration and frequency of GI complaints.
In contradistinction to those studies that found a positive relationship between children diagnosed with ASD and gastrointestinal dysfunction, analysis of a database of 211,480 children from the United Kingdom found no difference in gastrointestinal complaints in 96 children diagnosed with ASD compared with 449 nested controls [4]. Except for an increase in symptoms of constipation and unusual feeding behaviors such as food selectivity, investigators from the Mayo Clinic also found no significant associations were found between autism case status and overall incidence of gastrointestinal symptoms or any other gastrointestinal symptom category [17]. A recent Australian study concluded that children with early gastrointestinal problems were no more likely to be represented in the upper quartile of scores on the Autism Spectrum Quotient (AQ) scales [18].
The purpose of this investigational survey was to compare the prevalence of feeding difficulties and GI dysfunction in children with classic autism with their typically-developing siblings.
2. METHODS
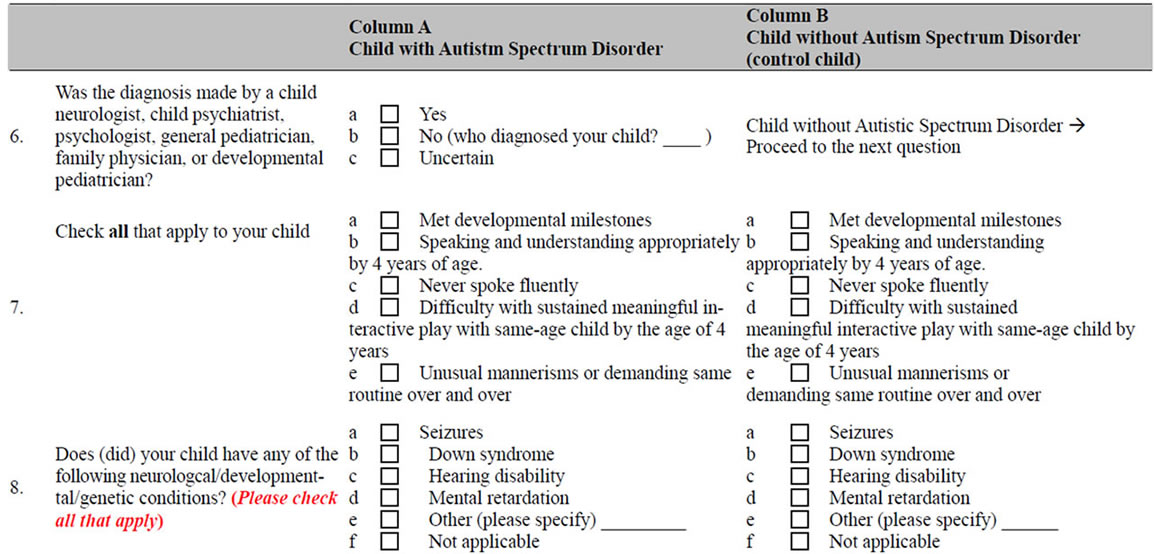
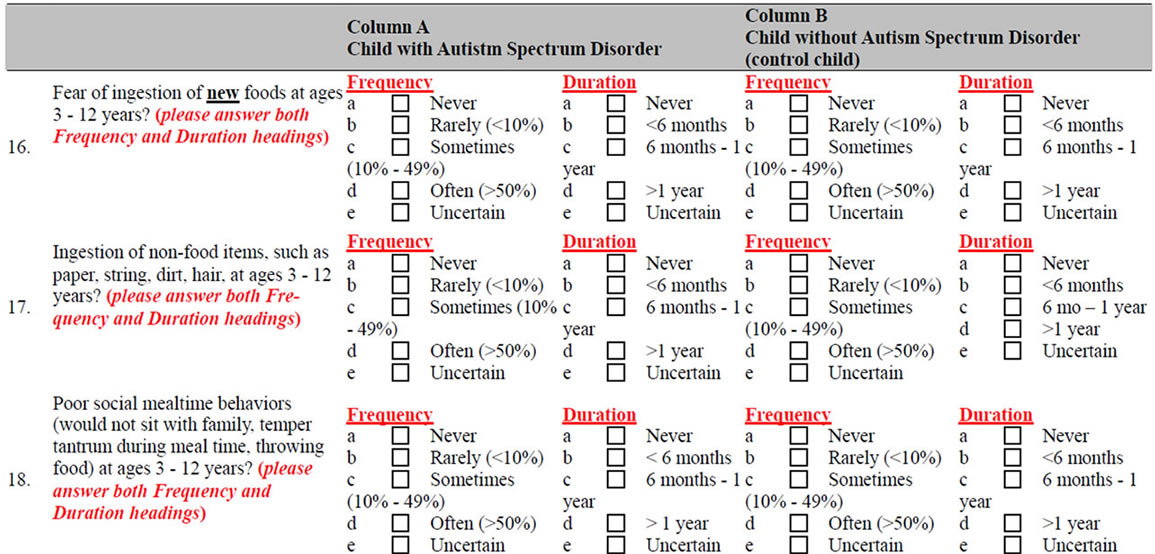
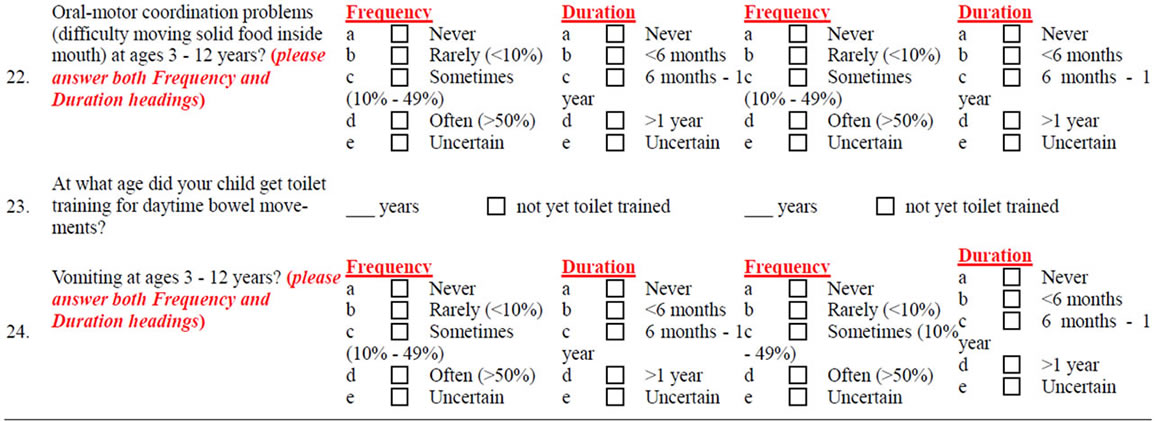
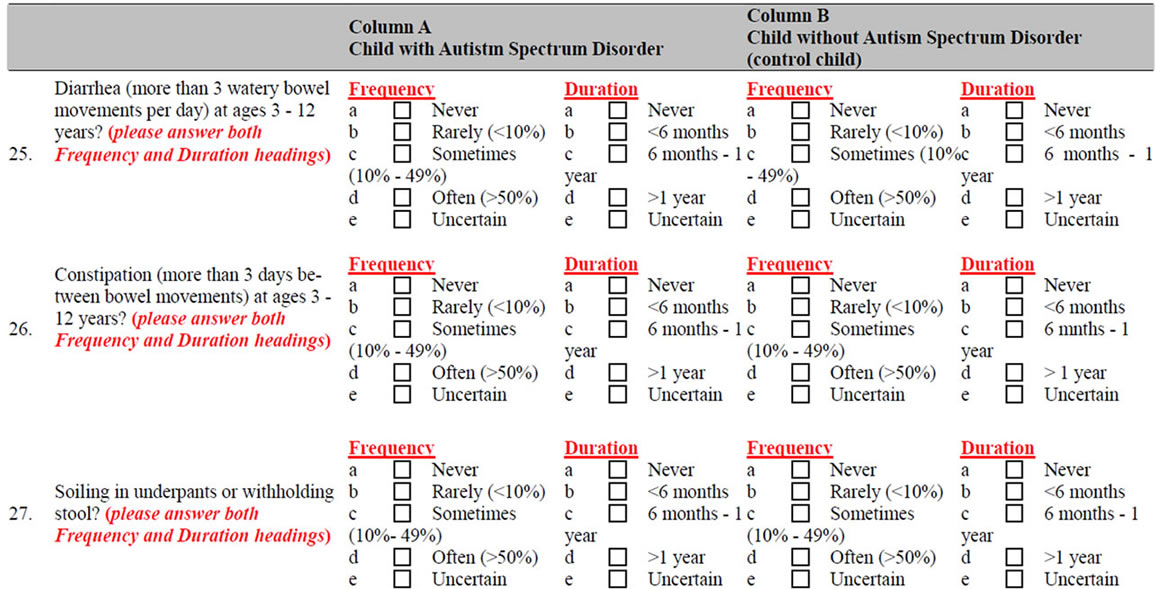
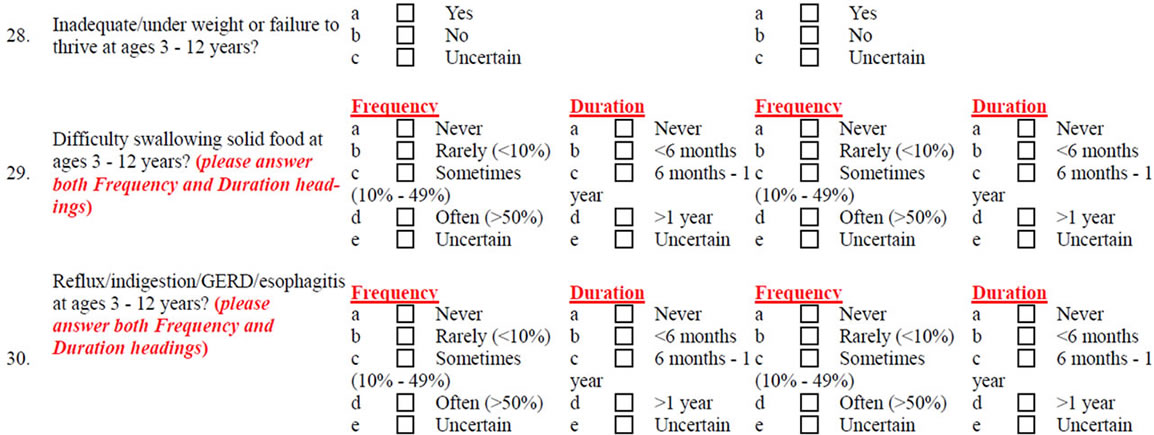
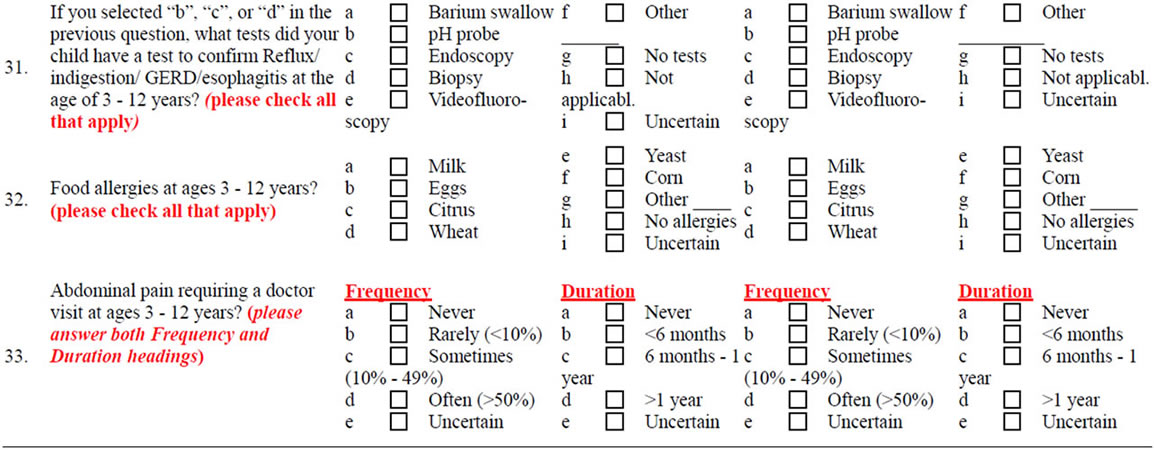
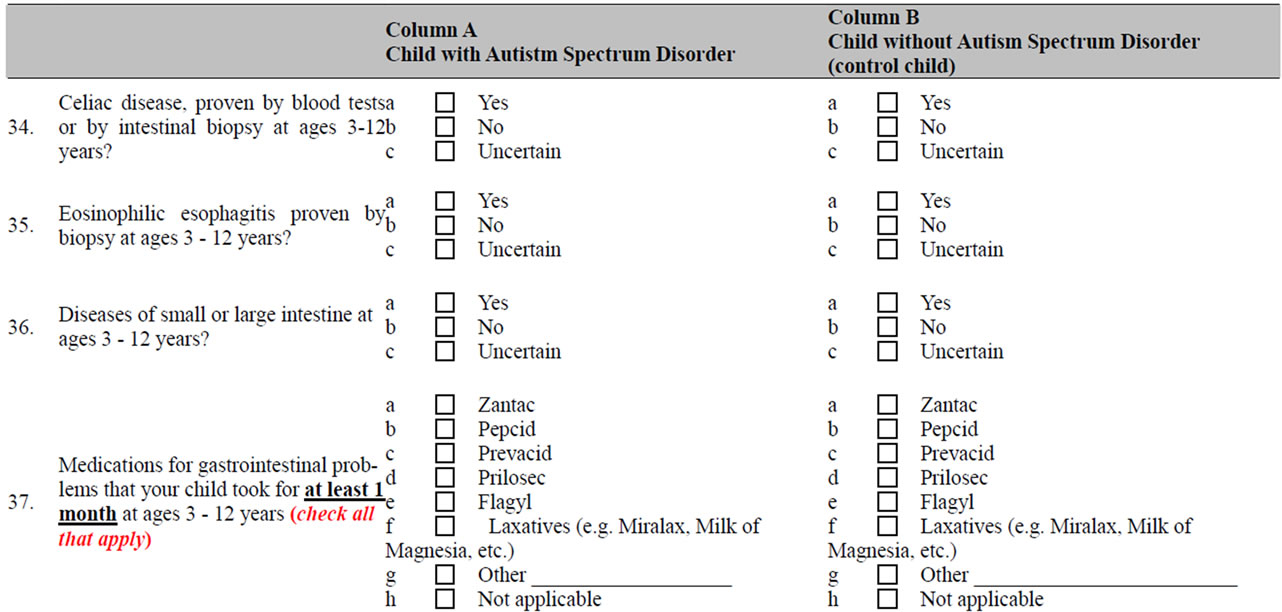
This was a cross-sectional online survey recruiting parents predominantly from the United States and Canada. The survey instrument was designed by authors and included 41 questions pertaining to demographics, family income, developmental milestones, feeding behavior, meal preferences, and GI dysfunction at the time when the child was between ages of 3 and 12 years (see appendix for copy of survey). The survey contained two mirror-image questions displayed side-by-side—the lefthand questions for the child with ASD, and the mirror image right-hand questions for a typically developing sibling. Both parts contained the same 41 questions, with the exception of the question pertaining to ASD diagnosis. The anonymous and confidential survey was securely posted online at a commercial survey website http://www.formsite.com (Vroman Systems Inc., Chicago, IL). For this manuscript we eliminated completed surveys from parents of children with Asperger syndrome or PDD-NOS and those with dual diagnosis of Down syndrome and ASD. Every child with classic autism was required to be diagnosed by a psychiatrist, neurologist, general pediatrician, developmental pediatrician, primary care family physician, or clinical psychologist. The link to the survey https://fs19.formsite.com/vbadalyan/form977322282/secure_index.html was emailed to a contact person at national, regional, state, and large city autism support groups. The survey link contained a statement about the purpose of the survey, assurance that participation was voluntary, information on risks and benefits, and contact information on study investigators and the IRB officer. If a parent had several typically developing children in addition to a child with ASD, he/she was asked to select the sibling closest by age to the ASD child and to complete the other part of the survey on the basis of that child’s experience.
The drafts of the survey were pre-tested on 10 parents who had a child on the autism spectrum. The purpose of our survey and the survey instrument itself were reviewed by a small group of specialists in developmental/ behavioral pediatrics, pediatric neurology, and pediatric gastroenterology. The study design and survey instrument were approved by Inova Fairfax Hospital Institutional Review Board (IRB).
2.1. Definitions Used for This Study
A child was defined as having autism if the parent indicated so in the survey and if the diagnosis had been made by a primary care physician, psychologist, or psychiatrist. All participating children had symptoms of serious developmental delay in language and communication, social interaction, and bizarre mannerisms representative of children with classic autism. We did not confirm the diagnosis of classic autism or feeding problems by further testing. We categorized the frequencies of feeding behavior and GI dysfunction into “Never,” “Rarely” (less than 10% of the time), “Sometimes” (10% - 50% of the time), and “Often” (more than 50% of the time).
“Diarrhea” was defined as passing at least three watery, unformed stools in a day. “Constipation” was defined as hard or painful stools passed less than three times per week. “Pica” was defined as the ingestion of unusual non-food items such as dirt or string.
2.2. Statistical Methods
Data were analyzed using SPSS version 16 (SPSS Inc. Chicago, IL). Pearson’s chi square test was conducted for nominal variables, and t-test was used for numerical variables. Binomial logistic regression was conducted, with socio-demographic, autism, and developmental milestones as independent variables and feeding and GI variables substituted one-by-one for the dependent variable.
3. RESULTS
Completed evaluable survey responses were received for 79 children with classical autism and their 79 typically developing siblings. Seventy-three percent of responses were from the United States, 11% were from Canada, and 10% were from New Zealand.
Boys comprised 90% of the autism group and 56% of the sibling group. The mean age at time of diagnosis was 3.1 years for the autism group (Table 1). The child’s average age at the time the survey was completed was 8.2 years in the autism group and 8.9 years in the control group.
Sixty-three percent of the parent responders reported that their household income in 2008 exceeded $50,000 per year.
The case and control groups differed significantly with respect to prevalence of frequent problematic feeding behaviors, including unusual food preferences (e.g., specific food colors, shapes, textures, presentation, or specific arrangement of food on the plate), insistence on eating food with specific utensils/dishes, dislike of new foods, fear of new foods, poor mealtime social behavior, unusual posturing during meals, and oral motor problems. No statistically significant differences between the two groups were noted with respect to eating nonfood items (pica) or poor school mealtime behaviors (Table 2).
There were significant differences between the two groups in with respect to the frequency of GI dysfunction, including constipation, soiling, diarrhea, and failure to thrive. Children with classic autism did not differ significantly from their sibling controls in rates of vomiting, abdominal pain, reflux, or dysphagia (Table 3).
Significant differences were reported between the two groups with respect to rates of food allergies (most of which were not confirmed by skin prick tests, ImmunoCAP-RAST serological tests, or food challenge tests) and special diets (Table 4).
Controlling for key variables, including age, gender, developmental milestones (spoon-fed before age of 3, toilet-trained before age of 4), presence of a medical problem, food allergies, and being on a special diet (gluten-free, Feingold, carbohydrate-free, soy-free), a logistic regression was conducted to estimate the association of autism with increased frequency of feeding problems (defined as problems occurring >50% of the time). Having autism was statistically significantly associated with an increased frequency of unusual food preferences (Table 5).

Table 1. Demographic Characteristics of cases and controls.

Table 2. Prevalence of problematic feeding behavior among cases and controls.

Table 3. Prevalence of gastrointestinal problems among cases and controls.

Table 4. Prevalence of food allergies and restricted diets among cases and controls.

Table 5. Odds ratios of exhibiting problematic mealtime behavior among children with autism compared to their typically developing siblings.
Using similar models, we substituted the dependent variable with each of the problematic feeding behaviors. We determined that some abnormal feeding behaviors were associated with autism (Table 5). After we had controlled for other variables, differences in insistence on specific food presentation, oral motor problems, posturing, and poor mealtime behavior ceased to achieve statistical significance.
We controlled for age, gender, and dietary restriction, to identify the impact of autism on differences in GI dysfunction between the two groups (Table 6).
4. DISCUSSION
The survey is based on a convenience sample of parents who were members of varied national, regional, state, and large city parent autism support groups. We agree that on-line surveys tend to capture respondents who have strong opinions on the subject, those with higher socioeconomic status, and those who are computer literate. Parents who responded to the survey may have been the most motivated by concerns about feeding issues or GI dysfunction with their children on the autism spectrum which can bias the results of a survey-based study. The strength of such a study is the greater geographic representation of survey participants, including capture of children with classic autism from small towns throughout the USA.
Is the diagnosis of classic autism accurate? The ratio of 9:1, boys:girls in our study is consistent with the expected sex ratio range of autistic children to their normally developing siblings. We are convinced that middle-class parents of children with autism, such as those that we included in our survey, consulted large city and state resources. Specialists in pediatric psychiatry, neurology, and developmental medicine were consulted by the majority of parents who responded to our survey. Parents also joined local, state, and national autism support groups. Children with classic autism had more severe disabilities in communication, language, socialization, compared to their sibling control and to children with less severe manifestations of autism such as Asperger syndrome [10]. We chose to exclude a standardized diagnostic test for classic autism in order to limit the time required to complete the questionnaire to less than 30 minutes. The inclusion of such a questionnaire such as Gilliam would have lengthened the survey to one hour. We recognize that some researchers in autism are likely to criticize this study because the diagnosis of autism may not have been made by standardized testing.
Some advantages of our study include 1) inclusion of specific questions on specific developmental and social milestones and bizarre behaviors and insistence on professionally-diagnosed ASD; 2) age-matched sibling controls; 3) geographic distribution (no state contributed more than 30% of the US total); and 4) large number of responses from families in small towns and cities in the United States and Canada.
We included questions about mealtime mannerisms and behaviors and specific G.I. dysfunction when children were between age 3 and 12 years. This age range was chosen by us for two reasons. Prior to the child’s third birthday, classic autism may be initially classified as pervasive developmental disorder-NOS. Feeding patterns and behaviors of children change often before the age of 3 but afterward remain relatively stable until adolescence.
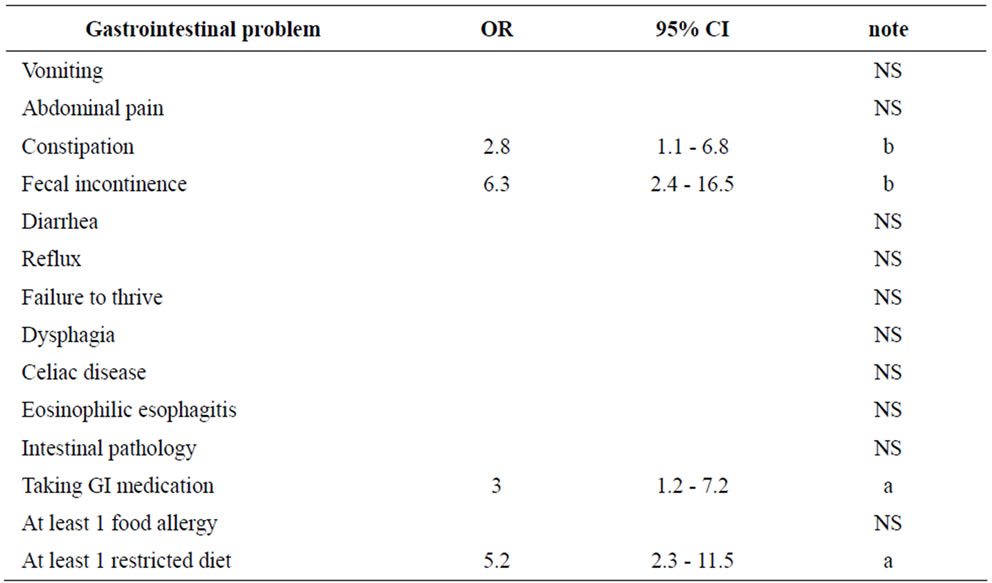
Table 6. Odds ratios of having gastrointestinal problems among children with autism compared to their typically developing siblings.
Previous surveys on this subject have limitations in study design. The well-regarded study from the Mayo Clinic was limited to children diagnosed with ASD who lived in Olmstead County, MN [17]. Information, culled from records of primary care physicians, was not provided whether the G.I. complaints of autistic children in the Mayo study were acute or chronic and we are not told if the problems were mild and transient or severe. Like those in the Mayo Clinic study, children with autism in our survey were more likely than their siblings to have feeding disorders, food selectivity, and constipation [17]. There was no increase in celiac disease in children with autism who resided in Rochester, MN and we also found no difference in this survey.
A multidisciplinary panel of experts recently reviewed the medical literature on the diagnostic evaluation and management of GI problems in children with ASD (20). Statement 12 of their consensus notes: “available research data do not support the use of a casein-free diet, a gluten-free diet, or combined gluten-free, casein-free (GFCF) diet as a primary treatment for individuals with ASDs” [19]. In our survey, more than 40% of children with classic autism had been on (or currently are on) casein-free, gluten-free, or GFCF diets, which is statistically significant (p < 0.01) compared to the sibling control group. Only 1% of those children on a gluten-free diet had a biopsy-proven diagnosis of celiac disease.
5. CONCLUSION
Children between the ages of 3 and 12 years with autism have a higher prevalence of selected abnormal feeding behaviors and GI problems compared with their typically-developing siblings. These behaviors include strange table mannerisms, fear of trying new foods, constipation, and fecal incontinence. More than 40% of children with classic autism had been on gluten-free, or GFCF diets. This is statistically significant (p < 0.01), compared to the sibling control group. Only 1% of those children on a gluten-free diet had a biopsy-proven diagnosis of celiac disease.
REFERENCES
- Mandy, W., Charman, T., Gilmour, J. and Skuse, D. (2011) Toward specifying pervasive developmental disorder-not otherwise specified. Autism Research, 4, 121-131. doi:10.1002/aur.178
- American Psychiatric Association. (2000) Diagnostic and statistical manual of mental disorders. 4th Edition, American Psychiatric Association, Washington.
- Prevalence of autism spectrum disorders. United States, 2006. Mortality Weekly Report, 18 December 2009, 1-20.
- Martins, Y., Young, R.L. and Robson, D.C. (2008) Feeding and eating behaviors in children with autism and typically developing children. Journal of Autism and Developmental Disorders, 38, 1878-1887. doi:10.1007/s10803-008-0583-5
- Matson, J.L., Fodstad, J.C. and Dempsey, T. (2009) The relationship of children’s feeding problems to core symptoms of autism and PDD-NOS. Research in Autism Spectrum Disorders, 3, 759-766. doi:10.1016/j.rasd.2009.02.005
- Matson, J.L. and Fodstad, J.C. (2009) The treatment of food selectivity and other feeding problems in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 3, 455-461. doi:10.1016/j.rasd.2008.09.005
- Molloy, C.A. and Manning-Courtney, P. (2003) Prevalence of chronic gastrointestinal symptoms in children with autism and autistic spectrum disorders. Autism, 7, 165-171. doi:10.1177/1362361303007002004
- Smith, R.A., Farnworth, H., Wright, B. and Allgar, V. (2009) Are there more bowel symptoms in children with autism compared to normal children and children with other developmental and neurological disorders? A case control study. Autism, 13, 343-355. doi:10.1177/1362361309106418
- Schreck, K.A., Williams, K. and Smith, A.F. (2004) A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders, 34, 433-438. doi:10.1023/B:JADD.0000037419.78531.86
- Kodak, T. and Piazza, C.C. (2008) Assessment and behavioral treatment of feeding and sleeping disorders in children with autism spectrum disorders. Child & Adolescent Psychiatric Clinics of North America, 17, 887-890. doi:10.1016/j.chc.2008.06.005
- Nadon, G., Feldman, D.E., Dunn, W. and Gisel, E. (2011) Mealtime problems in children with autism spectrum disorder and their typically-developing siblings: A compareson study. Autism, 15, 98-113. doi:10.1177/1362361309348943
- Wang, L.W., Tancredi, D.J. and Thomas, D.W. (2011) The prevalence of gastrointestinal problems in children across the United States with autism spectrum disorders from families with multiple affected members. Journal of Developmental & Behavioral Pediatrics, 32, 351-360. doi:10.1097/DBP.0b013e31821bd06a
- Provost, B., Crowe, T.K., Osbourn, P.L., McClain, C. and Skipper, B.J. (2010) Mealtime behaviors of preschool children: Comparison of children with autism spectrum disorder and children with typical development. Physical & Occupational Therapy in Pediatrics, 30, 220-233. doi:10.3109/01942631003757669
- Lukens, C.T. and Linscheid, T.R. (2008) Development and validation of an inventory to assess mealtime behavior problems in children with autism. Journal of Autism and Developmental Disorders, 38, 342-352. doi:10.1007/s10803-007-0401-5
- Seiverling, L., Hendy, H.M. and Williams, K. (2011) The Screening Tool of Feeding Problems applied to children (STEP-CHILD): Psychometric characteristics and associations with child and parent variables. Research in Develop Disabilit, 32, 1122-1129. doi:10.1016/j.ridd.2011.01.012
- Black, C., Kaye, J.A. and Jick, H. (2002) Relation of childhood gastrointestinal disorders to autism: Nested case-control study using data from the UK General Practice Research Database. British Medical Journal, 325, 419-421. doi:10.1136/bmj.325.7361.419
- Ibrahim, S.H., Voigt, R.G., Katusic, S.K., Weaver, A.L. and Barbaresi, W.J. (2009) Incidence of gastrointestinal symptoms in children with autism: A population-based study. Pediatrics, 124, 680-686. doi:10.1542/peds.2008-2933
- Whitehouse, A.J., Mayberry, M., Wray, J.A. and Hickey, M. (2011) No association between early gastrointestinal problems and autistic-like traits in the general population. Developmental Medicine and Child Neurology, 53, 457-462. doi:10.1111/j.1469-8749.2011.03915.x
- Buie, T., Campbell, D.B., Fuchs, G.J., Furuta, G.T., Levy, J., Van de Water, J., et al. (2010) Evaluation, diagnosis, and treatment of gastrointestinal disorders in indiviuals with ASDs: A consensus report. Pediatrics, 125, S1-S18. doi:10.1542/peds.2009-1878C
APPENDIX
Survey Instrument

By filling out the following survey, you can help pediatricians and other health professionals learn more about certain problems in children with autism spectrum disorders (ASDs). Such problems include unusual food preferences; aversion to certain food colors, textures, and types; ingestion of non-food items; very restricted choices of foods; special diets; sensory processing disorders; oral-motor swallowing problems; vomiting, diarrhea, or constipation; and symptoms of gastroesophageal reflux (GERD) and its complications, such as erosive esophagitis, and food allergies.
Questions in Column “A” pertain to your child with ASD when he/she was ages 3 - 12 years, even if he/she is older now. In Column “B”, we ask the same questions for a sibling of your ASD child, closest to him/her in age. Please check the applicable box below and follow the instructions.

Please FILL IN the blanks or CHECK the best choice of the following questions:






NOTES
*Corresponding author.

