Journal of Biomedical Science and Engineering
Vol.5 No.12A(2012), Article ID:26189,4 pages DOI:10.4236/jbise.2012.512A095
Fatal liver abscess caused by Clostridium perfringens complicated with transarterial chemoembolization
![]()
Department of Radiology and Center for Endovascular Therapy, Kobe University Hospital, Kobe City, Japan
Email: nosakamoto@hotmail.co.jp
Received 2 October 2012; revised 9 November 2012; accepted 19 November 2012
Keywords: Liver; Hepatocellular Carcinoma; Transarterial Chemoembolization; Clostridium perfringens
ABSTRACT
A 77-year-old man who received transarterial chemoembolization for large hepatocellular carcinomas complained of acute pain in the upper abdomen and suddenly developed severe jaundice, anemia, and massive hematuria. Abdominal computed tomography demonstrated gas gangrene at the tumor site. Clostridium perfringens was identified from blood samples and drainage cultures from the liver abscess. Despite intensive treatment, the patient died 55 hours after chemoembolization due to multiple organ failure. When treating patients with large tumors, such as in our case, this rare but fatal complication that causes sepsis and hemolysis with lightning-like rapidity should be considered.
1. INTRODUCTION
Transarterial chemoembolization (TACE) is an indispensable treatment option for patients with unresectable hepatocellular carcinoma (HCC) [1]. However, TACE has been associated with several complications, including critical complications such as hepatic infarction, and liver abscess [2,3]. Herein, we present an extremingly rare but fatal complication caused by Clostridium perfringens after TACE for large HCC.
2. CASE REPORT
A 77-year-old man with a previous history of chronic hepatitis type C and diabetes mellitus was referred to our institution for the treatment of two large HCCs with the maximum diameter 6 cm in the right lobe with no evidence of portal venous tumor thrombus. Laboratory data was as follows: hemoglobin (15.9 g/dl); total leukocyte count (6100 μ1); platelets (8.1 × 104/μl); a slight elevation in total bilirubin (1.9 mg/dL), a significant elevation in alpha-fetoprotein (AFP) (206 U/mL) were also noted. The degree of hepatic dysfunction using Child’s classification was A. The surgery was not considered due to the age and tumor size; thus, we opted for fractionated TACE to reduce the side effects in the light of the tumor size. The first selective TACE for treating the tumor in segment seven was performed without use of antibiotic prohylaxsis. Intra-arterial infusion of a suspension of 6 mL iodized oil (Lipiodol ultra fluid; Laboratoires Guerbet, Aulnay-sous-Bois France) and 120 mg of SM-11355 (Miriplatin; Dainippon Sumitomo Pharma Co., Ltd., Osaka, Japan) was followed by embolization using 30 mg of Gelpart (Nipponn Kayaku Co., Ltd. Tokyo, Japan) until the tumor stain was imperceptible.
High fever continued for 10 days after the procedure, which was indicating a post-embolization syndrome; the patient gradually recovered without requiring antibiotics . The second selective TACE for treating the tumor in segment six was performed one month later. Computed tomography (CT) showed good accumulation of the iodized oil in the both tumors (Figure 1). One day after the second treatment, the patient was feeling well during the day time despite high fever (39.1˚C) and chromaturia. For chromaturia, we performed only a dipstick test, which resulted negative. The inflammatory index was not elevated (total leukocyte count: 4000 μL). Other Laboratory data were within normal limit except for a slight elevated aspartate aminotransferase (AST) (171 IU/L) and alanine aminotransferase (ALT) (181 IU/L). However, by midnight, the patient complained of acute pain in the upper abdomen, and suddenly developed severe jaundice and anemia, with massive hematuria. The patient soon became disoriented and fell into a lifethreatening state of shock, with blood pressure (81 mmHg) and heart rate (149 beats/min). A standard laboratory analysis was impossible due to massive intravascular hemolysis. Blood gas analysis suggested acute hyperkalemia and metabolic acidosis; the he-


Figure 1. CT images of a large hepatocellular carcinoma in a 77-year-old man after a second TACE; CT images demonstrate almost complete filling of the tumor in segment 7 (the left image) and segment 6 (the right image) with deposition of lipiodol suggesting therapeutic effect of the treatment.
moglobin level was 9.7 g/dL; total leukocyte count, 21,400 μL; platelet count, 5.2 × 104 μL; and potassium, 6.3 mmol/L (pH 7.319, base excess: –13.6 mmol/L). Fluid resuscitation and intravenous antibiotic (Meropenem Hydrate; Meropen; Dainippon Sumitomo Pharma Corporate, Tokyo, Japan) in addition to vasopressor administration (Dopamine; Kyowa Hakko Kogyo Co., Tokyo, Japan) was started immediately. Emergency CT demonstrated presence of free air at the liver surface and two large liver abscesses containing gas (Figure 2). We immediately performed continuous hemodiafiltration therapy and inserted a percutaneous drainage tube (BIOTEQ 8Fr Pigtail Drainage catheter; Bioteque Corporation, Taipei, Taiwan) into the larger liver abscess in segment six under ultrasonographic guidance. Samples of blood and abscess content revealed gram-positive rods; given this clinical course, Clostridium perfringens was the most likely diagnosis. Clinical improvements were, however, not observed, and the patient died 55 hours after the second TACE due to multiple organ failure. Autopsy confirmed two large liver abscess formations. Four days later, the laboratory reported blood and drainage cultures with gram-positive rods identified as Clostridium perfringens (Figure 3). It was concluded that the entire clinical course was caused by Clostridium perfringens septicemia.
3. DISCUSSION
Clostridium perfringens is a gram-positive anaerobic saprophytic bacterium, which can produce extracellular toxins and heat-resistant spores [4-7]. It is difficult to make a rapid diagnosis of clostridial infection, because the initial symptoms are non-specific. However once the patient has become septic, the toxin damages the structural integrity of the red cell membrane inducing intravascular


Figure 2. CT findings at the time of patient’s sudden deterioration. The tumor in segment 6 (arrow) has been replaced by gas gangrene (the left image). The caudal liver parenchyma (arrow) also demonstrates an emphysematous appearance (right image). Some free air is also seen near the liver surface (arrow heads).
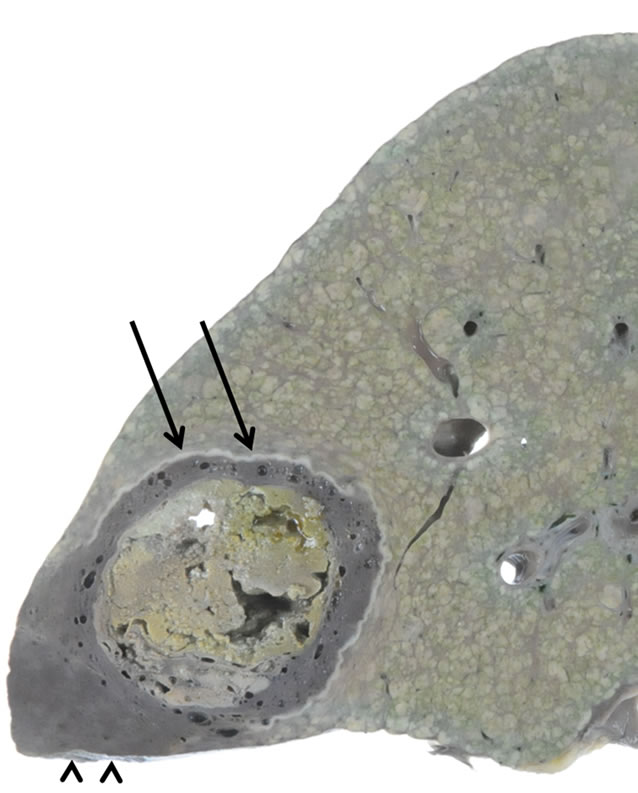
Figure 3. Gross specimen of the liver on post-mortem; Abscess with gas gangrene (arrows) were seen at the site corresponding to the large tumor in segment 6. The caudal liver parenchyma (arrow heads) also demonstrates an emphysematous appearance with dark color, which is also caused by Clostridium perfringens infection.
hemolysis, resulting in anemia and jaundice shortly after [4]. Immediately after intravascular hemolysis, patient descends into a state of shock, and multiple organ failure and death typically follow within several hours. In the reviewed cases, the patient had already gone into shock
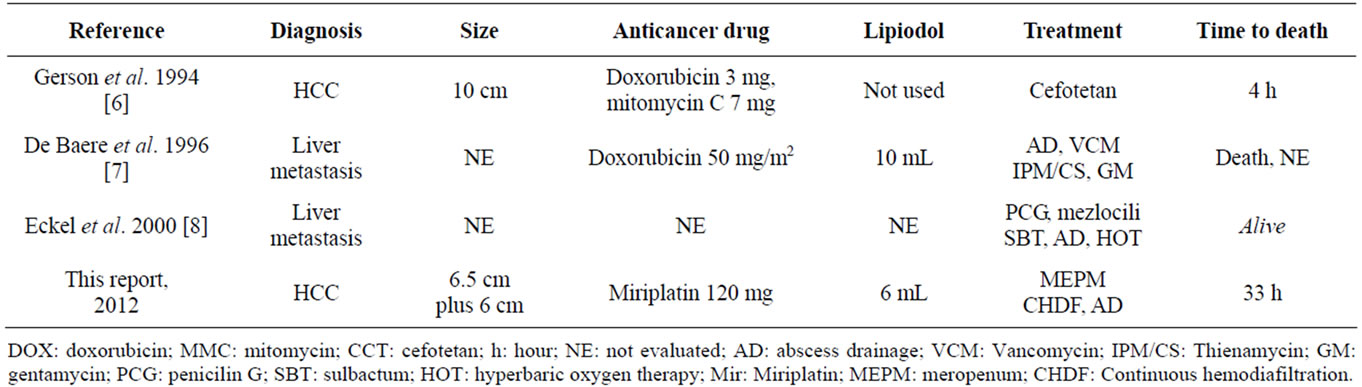
Table 1. Reports of patients with liver tumors who have developed liver abscesses caused by Clostridium perfringens after TACE.
or died before a diagnosis could be made, and 70% - 100% patients did not survive; the median time between admission and death was only 8 hours [4]. Major complications of TACE, such as liver dysfunction, hepatic infarction, liver abscess, pulmonary oil embolism and tumor lysis syndrome have been well described [2,3]. To our knowledge, only 3 reports of liver abscess caused by Clostridium perfringens have been described to date [5- 7]. According to previous reports of clostridial infection complicating TACE, majority of the cases were associated with metastatic tumors with the past history of bilio enteric anastomosis [6,7]. There was only one patient with a large HCC (with the maximum diameter 10 cm) without a history of previous surgery, and our case was very similar and, to the best of our knowledge, was the second case in the English literature (Table 1). In our patient, the risk of infection was high due to advanced age, the presence of diabetes mellitus, and advanced malignancy. An anaerobic environment due to the second TACE might have allowed C. perfringes to grow at an explosive rate. During the procedure, we administered a lipophilic platinum derivate called Miriplatin, a new intraarterial chemotherapeutic agent for HCC approved by the Japanese government. The therapeutic principle is entirely the same as that for conventional TACE [1]; thus, it is unlikely that the agent was to blame for the Clostridium perfringens infection. Even though the initial symptoms are similar to those of severe post-TACE syndrome [5-7], to rescue the patient, we must always anticipate the possibility of serious infection including Clostridium perfringen. Blood samples should be taken and a diagnosis made from blood smear and Gram staining, because identification of Clostridium perfringens in blood culture is usually indispensable for making a correct diagnosis. Antibiotic treatment should commence without waiting for the culture test results, because early antibiotic treatment, and if possible, removing the focus of infection, can be the only possibly effective treatment [5-7]. In general, antibiotic prophylaxis is not necessary in patients with HCC undergoing chemoembolization [8]. When treating metastatic tumor with the past history of bilio enteric anastomosis or a large HCC, however, antibiotic prophylaxis might be justified.
In summary, this report describes a case of a fatal liver abscess caused by Clostridium perfringens infection as a complication of TACE. In severely ill patients with fever and hemolysis after TACE, this rare complication should always be considered, since early antibiotic treatment and removing the focus of infection is the only way to rescue such patients from an otherwise fatal outcome.
REFERENCES
- Yamada, R., Sato, M., Kawabata, M., et al. (1983) Hepatic artery embolization in 120 patients with unresectable hepatoma. Radiology, 148, 397-401.
- Sakamoto, N., Monzawa, S., Nagano, H., et al. (2007) Acute tumor lysis syndrome caused by transcatheter oily chemoembolization in a patient with a large hepatocellular carcinoma. Cardiovascular and Interventional Radiology, 30, 508-511. doi:10.1007/s00270-005-0240-8
- Song, S.Y., Chung, J.W., Han, J.K., et al. (2001) Liver abscess after transcatheter oily chemoembolization for hepatic tumors: Incidence, predisposing factors, and clinical outcome. Journal of Vascular and Interventional Radiology, 12, 313-320. doi:10.1016/S1051-0443(07)61910-1
- van Bunderen, C.C., Bomers, M.K., Wesdorp, E., et al. (2010) Clostridium perfringens septicemia with massive intravascular haemolysis: A case report and review of the literature. Netherlands Journal of Medicine, 68, 343-346.
- Gerson, L.B., Pont, A. and Cummins, R.T. (1994) Clostridial bacteremia and death following chemoembolization for hepatocellular carcinoma. Journal of Vascular and Interventional Radiology, 5, 167-170. doi:10.1016/S1051-0443(94)71477-9
- de Baere, T., Roche, A., Amenabar, J.M., et al. (1996) Liver abscess formation after local treatment of liver tumors. Hepatology, 23, 1436-1440. doi:10.1002/hep.510230620
- Eckel, F., Lersch, C., Huber, W., et al. (2000) Multimicrobial sepsis including Clostridium perfringens after chemoembolization of a single liver metastasis from common bile duct cancer. Digestion, 62, 208-212. doi:10.1159/000007815
- Shim, J.H., Park, J.W., Choi, J.I., et al. (2009) Does postembolization fever after chemoembolization have prognostic significance for survival in patients with unresectable hepatocellular carcinoma? Journal of Vascular and Interventional Radiology, 20, 209-216. doi:10.1016/j.jvir.2008.10.021

