Forensic Medicine and Anatomy Research
Vol.1 No.2(2013), Article ID:29895,9 pages DOI:10.4236/fmar.2013.12002
Artefact in forensic medicine: The jigsaw piece in a thanatopsy puzzle
![]()
Greater London Forensic Medical Practice, London, UK; glfmp@btinternet.com
Copyright © 2013 Freddy Patel. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 2 January 2013; revised 4 February 2013; accepted 23 February 2013
Keywords: Thanatopsy; Coronary Syndrome; Resuscitation Trauma; Pulseless Electrical Activity; Medical Expert Witness
ABSTRACT
The case presented involved a middle aged male who suffered a witnessed collapse on the street near a violent public demonstration. Bystanders gave first-aid before cardiopulmonary resuscitation (CPR) was initiated by police officers and continued by paramedics and at the hospital. The death was regarded as non-suspicious by the local crime scene investigators who nonetheless were in attendance at the mortuary in case there was evidence of assault or crush injury associated with public disorder. A relatively minor hepatic injury with blood stained ascites was found during the postmortem examination and attributed to CPR. A cause of death ascertained provisionally as coronary artery disease was disputed by exclusive pathologists and medical experts who instead favoured abdominal haemorrhage without having observed the bloodstained ascites. This case illustrates that in reality a cause of death is a clinical opinion rather than a medical fact and conflicting opinions may be held by medical experts. Some medical opinions may be a product of clinical bias with subconscious weighting of signs and symptoms that suits a diagnosis. Forensic pathologists in a court room sometimes may sense overrated medical opinions reinforced by muchness of medical experts inhibit less popular evidence-based opinions. Something akin to a court order for pre-trial discussion of polemic medical opinions may address a fundamental problem of communication between medical experts. It would assist the court if conflicting medical evidence and evidential limitations of the expert witnesses can be resolved constructively.
1. INTRODUCTION
A postmortem examination was performed to ascertain a cause of death at the request of the Coroner under S. 20 of the Coroners Act 1988 (England & Wales) where it has been predetermined that an inquest is necessary and additional skills and/or special ancillary examination may be required to find a registrable cause of death and fulfil a statutory requirement [1,2]. There is a legal requirement of pathologists to report to the coroner but there is no legal definition of a postmortem examination and the expectation is mooted in the postmortem report designed for the unwashed to understand as set out in the format of Schedule 2 of the Coroners Rules 1984 (England & Wales) [1,2].
The thanatopsy findings and ancillary investigations were duly conveyed to the coroner. A provisional cause of death was ascertained as coronary artery disease on balance of probability, which may or may not have been causally related to a stressful situation depending on the prevailing temporal circumstances. The death as a result of acute coronary syndrome was disputed by other pathologists after re-examination of the body, and favoured abdominal haemorrhage as the immediate cause of death without having observed or enquired about the misconstrued evidence of bloodstained ascites. A pathologist excluded a coronary event as a possible etiology but could not be certain about lethal cardiac arrhythmia caused by alcoholic cardiac disease.
The death was regarded as non-suspicious by local crime scene investigators who nonetheless were in attendance at the mortuary in case there was evidence of assault or crush injury associated with public disorder. It had been reported that there were sticks and poles and glass bottles thrown as missiles by unruly protesters at the scene.
A few days later, video footage emerged that showed a police officer in riot gear strike the subject on the left thigh from behind with a baton before forcefully pushing him to the ground in a contralateral forward fall and semisupine roll onto the right arm. He was able to sit up straight away and talk to bystanders who helped him on to his feet. The video showed police dogs held on leash in the background but there was no sign of canine contact.
Thereafter, he can be seen ambling away unconcerned and with no obvious indication of trauma to the right torso or a dog bite to the lower leg. A moment later he was seen moving along with the crowd and appeared to be jogging before jokingly running into a pillar and falling to the ground a few more paces away where he was found collapsed. It was reported that he had an earlier fall to the ground several minutes before the videoed incident and had been moved on along with protesters.
2. CASE REPORT
2.1. History
The deceased was a middle aged Caucasian male who suffered a witnessed collapse on the street near a public disorder situation. A bystander who witnessed the collapse gave first-aid and thought that there was a palpable radial pulse before police medics initiated cardiopulmonary resuscitation (CPR). The paramedics who found him unresponsive with peripheral shut down and no peripheral venous access continued CPR and restored spontaneous respiration 15 per minute, and noted that an endotracheal tube was tolerated without sedation. A paramedic noted that there was no pulse palpable but another paramedic reported a spontaneous return of circulation with heart beats for about a minute some 25 minutes after the terminal collapse. However, it was decided that the poor quality defibrillator rhythm strips obtained to identify heart rhythm after a delay of some 15 minutes and which showed narrow complex electrical activity in sinus rhythm at 70 beats per minute, and 15 minutes thereafter at about 50 beats per minute evinced pulseless electrical activity (PEA) caused by possible internal haemorrhage but could not rule out coronary thrombosis.
The first-aider who was with him for about five minutes described him as smelling of alcohol, smiling and laughing and not in distress or complaining of any pain. He was not ashen and spoke to say that he was okay before micturating and becoming rapidly unresponsive. His breathing had changed as if snoring, his legs went into brief spasm, he did not respond to commands to move the legs nor to a painful stimulus and remained unresponsive but his eyes stayed open. The description of his demeanour resembled anecdotes of silent coronary event rather than somebody dying of an internal haemorrhage amounting to 60% of the total blood volume. It would have been difficult for paramedics to differentiate car diogenic shock from hypovolaemic shock without a central venous pressure (CVP) which is constantly changing and would render a single static assessment of CVP unreliable.
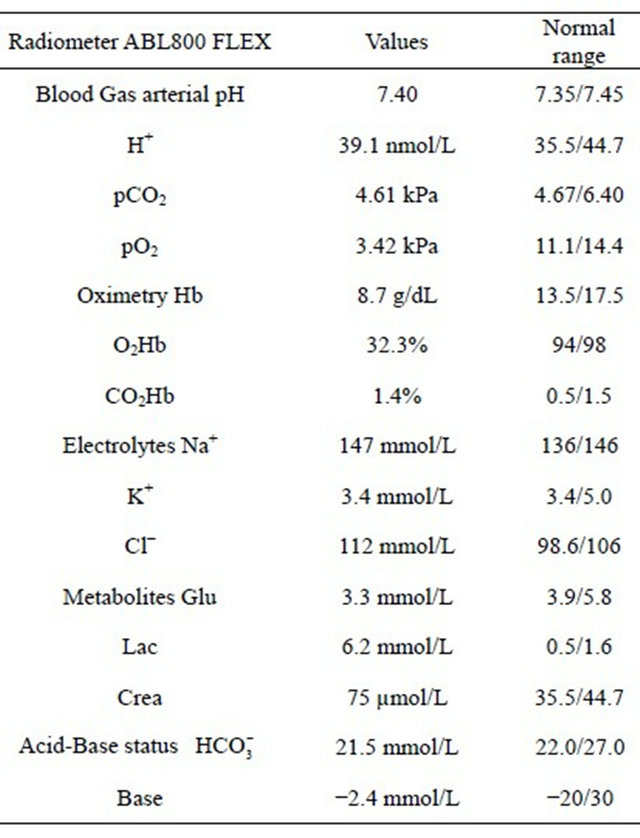
The basic life support was continued and he was taken to hospital where intravenous access was gained but no fluids were infused. His vital signs were narrow complex PEA with a heart rate 30 per minute; dilated pupils, body temperature 36.1˚C and Glasgow Coma Scale (GCS) 3/15. The correct positioning of endotracheal tube was confirmed by auscultation and end tidal capnograph monitor. A cardiac ultrasound scan showed no cardiac activity and chest compressions with mechanical cardiopulmonary assist system was unsuccessful. Life was pronounced extinct after several minutes of emergency therapeutic intervention and around 45 minutes past his terminal collapse. The hospital biochemical parameters are shown in Table 1.
His pre-existing medical conditions included ethanolic chronic liver disease with hepatomegaly, ascites, paraumbilical hernia, portal hypertension, oesophageal varices and haematemesis; hypotension [BP 90/50 - 110/70 mmHg]; echocardiogram with regional mural hypokinesia; hypersplenism; anaemia [Hb 11.2 - 12.1 g/dL]; mild thrombocytopenia; international normalised ratio (INR) 1.1; peripheral neuropathy; right hemiparesis with an unremarkable brain scan; multiple drunken falls, chronic left shoulder dislocation and heavy smoking.
Table 1. Radiometer values on admission to hospital.
2.2. Thanatopsy
The deceased was a well nourished male 1.75 m in height and weighed 70 kg. His clothing had been removed and he was dressed in a hospital gown. There were defibrillator pad marks on the chest and other signs of emergency therapeutic intervention. Hypostasis was intense and posterior (Figure 1).
There were no significant external marks of violence other than:
• a minor abrasion on the right elbow point (Figures 2 and 3) and a small blue bruise on the right wrist, with corresponding small subcutaneous contusion and small subcutaneous contusion on the left elbow and shoulder point, with no external injury;
• a blue bruise 14 cm × 6 cm angled at 45˚ and incorporating parallel linear bruises 1cm and lower 6cm long with a 1cm pallid gap on the left anterolateral mid thigh (Figure 4), with corresponding 14 cm × 3 - 5 cm subcutaneous contusion and no deeper tissue injury;
• an abrasion over the right kneecap and a pale red bruise on the left kneecap, with corresponding subcuta neous contusion on the right knee;

Figure 1. Intense posterior hypostasis, and note the injury suspected to be from a dog bite to the right lower leg depicted in Figure 6.

Figure 2. Minor external injury on the right elbow to the same side of the fall to the ground.
• full skin-thickness punctured laceration 0.5 cm in the lower end of a red bruise 3 cm × 1 cm angled at 45˚ and adjacent lower parallel linear small red intradermal bruises up to 1cm apart on the right inside shin (Figure 5) and lower similar marks with partial skinthickness punctured skin flap laceration in the upper end of a blue/red bruise 2 cm × 1 cm on the right calf and spanning 5 cm × 3 m (Figure 6), with corresponding subcutaneous contusion and probed wound tracks of the two punctured wounds were directed outwards in opposite directions There was about three litres of heavily blood stained ascitic fluid and a small blood clot about 10 - 20 ml which lay free within the small bowel loops (Figure 7). There was no evidential 3 l loss of blood and a meticulous

Figure 4. Bruised injury on the left thigh.

Figure 5. Punctured injury of the upper shin on right lower leg.

Figure 7. Extraperitoneal perimortem small blood clot.
exploration of the abdominal contents showed no source for a large blood loss. The oesophageal varices were intact and showed no sign of haemorrhage. The spleen was enlarged and congested but there was no sign of any abdominal varices. The kidneys were unremarkable and showed no sign of exsanguination.
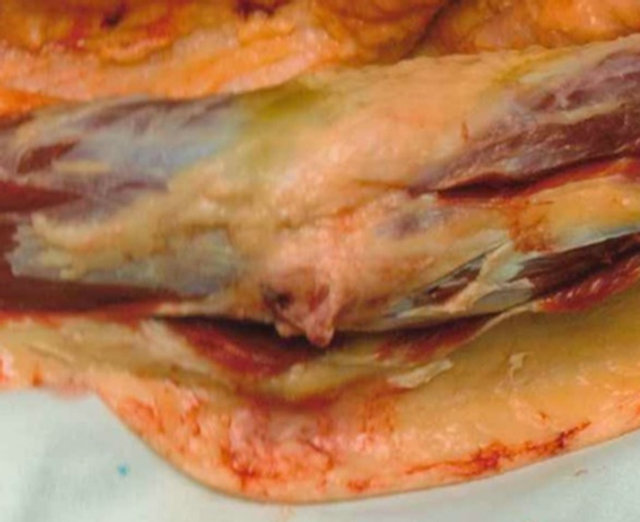
The liver weighed 2500 g and was markedly enlarged with severe steatosis and cirrhosis. There was a localised 3 cm2 area of congealed acute punctate haemorrhages up to 5 mm corresponding to the intrahepatic nodularity and reached a subcapsular parenchymal depth of 2 cm, with no sign of capsular tears or subcapsular haematoma (Figures 8 and 9). There were fine punctate congealed haemorrhages in the central omentum (Figure 9). There were transverse sternal and stable left anterior and right anterolateral rib fractures with bilateral soft tissue contusions overlying the fifth ribs and apical pericardial fat (Figure 9). There was no sign of peripheral bone injury.
The examination of the heart [390 g] showed ischaemic discolouration and triple vessel coronary atherosclerosis with calcific stenosis estimated between 80% - 90% in the proximal left anterior descending artery and a first order branch (Figure 10). There was no identifiable acute infarct, coronary thrombus, plaque disruption or ischaemic scarring. The lungs [R 685g and L 610g] showed gross pulmonary oedema with basal consolidation. The brain [1420 g] showed intravascular blood filled cerebral vessels and not exsanguination (Figure 11).
2.3. Ancillary Examinations
Tissue samples retained for microscopy confirmed severe atherosclerosis with comparable stenosis (Figure 12). A heart section showed right ventricular adiposity with no sign of arrhythmogenic dysplasia. A kidney section showed acute tubular necrosis.
Toxicology showed alcohol concentrations of 410 mg% and 368 mg% in the femoral venous blood and 400 mg%

Figure 8. Cut-section of localised hepatic haemorrhages, with no capsular or hepatic lacerations or subcapsular haematoma.

Figure 9. Thoraco-abdominal contents with pericostal and epicardial contusions, liver cirrhosis, fine omental contusions and pool of blood stained ascites, with no varices from portal hypertension.
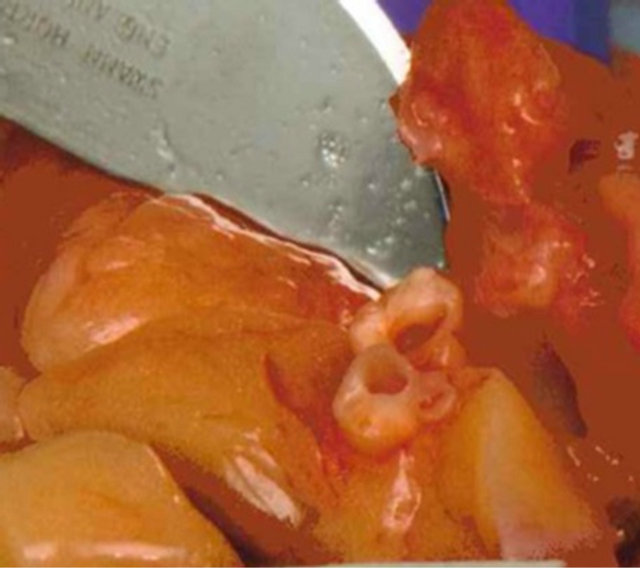
Figure 10. Cut-section of eccentric coronary stenosis in atherosclerotic left anterior descending branch with slit-hole lumen in calcified first order branch [×2].
and 425 mg% in the urine. There was no indication of alcoholic ketoacidosis.
3. DISCUSSION
An estimation of the actual volume of abdominal blood loss, its source and rate and whether it was antemortem and caused by trauma or sustained in the perimortem
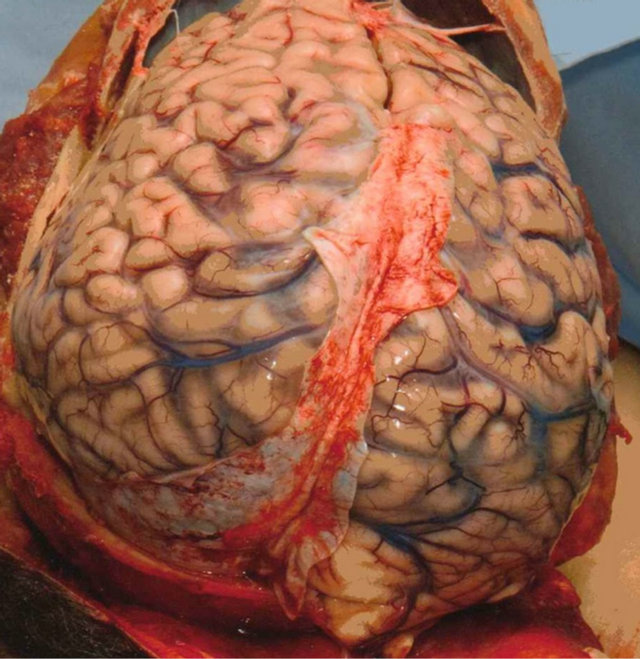
Figure 11. Brain in-situ with blood-filled cerebral vasculature.
period due to CPR became highly contentious. The fact that a cause of death had already been attributed to acute coronary syndrome did not flag up a heuristic ambiguity about 3 l of blood loss, i.e. 60% of the total blood volume. An opportunity for professional communication when pathologists discover important discrepancy was not prompted in the spirit of the guidelines for forensic pathologist, although a pathologist stated the need to enquire of the initial pathologist about the ambiguity over the volume of haemorrhage [3]. There were no signs of exsanguinations such as pale or absent hypostasis and renal pallor or major trauma to abdominal organs and blood vessels with peripheral vascular blood depletion. The timeline interval of a minute and half or two would have been insufficient for manifestation of a substantial blood loss from the hepatic and omental sites or produce lethal hypovolaemia before the terminal collapse.
The clinical effect of hypovolaemia is known to depend not only on the volume of blood loss itself but also on the rate of haemorrhage and potential for the source to bleed freely to the extent that a given volume of blood loss which ordinarily might be fatal may not cause death if the seepage of blood is slowed over a prolonged period. The timeline of a couple of minutes would have been insufficient to produce a fatal internal haemorrhage from a pathologically disproportionate hepatic damage with an apparent intact capsule. The volume of blood loss could have been artefactually large because of the chronic liver disease interfering with haemostasis although a recent INR was normal. There was no discernible source for 3l blood loss as had been inferred by medical experts opting for an internal haemorrhage as alternate cause death. It
Figure 12. Microscope slide corresponding to life-size end-on eccentric coronary stenosis in levels of atherosclerotic left anterior descending branch, and distorted slit hole lumen in calcified first order branch, visible in Figure 10.
was claimed by pathologists that bleeding from the injury to the liver (Figure 8) would have been profuse and brisk because of an abnormal vasculature in portal hypertension, and the small blood clot found in the abdomen (Figure 7) was a sign of a substantial haemorrhage. As a matter of fact, a relatively minor internal liver injury, without back pressure effect of portal hypertension found in the extrahepatic venous circulation, would be expected to manifest as a slow bleed.
It has been noticed during post-mortem eviscerations that a relatively small volume of freed blood may blend with effusions or ascites and mimic frank blood. In a similar way, it would not be difficult after a CPR induced bleed for ascites to become heavily blood stained artefactually from handling during resuscitation attempts in the street and at the hospital, then the removal of the body by undertakers and further log-rolling in the mortuary. An opinion of a surgical expert that the dilution factor in blood mixed ascitic fluid could be derived by a haemoglobin test prompted a literature search for anecdotal cases, including a haematocrit test but no match was found where the proportions had been determined after death. Forensic pathologists may be deterred from requesting these laboratory tests since collection of an entire volume of vast quantity of body fluid would not be feasible generally and a small sample may not be representative. It is noteworthy that in clinical practice the value of haemoglobin concentration is considered to be a poor indicator of the volume of whole blood deficit and haematocrit test may be unreliable due to modification by compensatory mechanisms in the early stages of hypovolaemia.
The hepatic damage was agreed by pathologists to be the main source of haemorrhage. However, the mechanism of the trauma—whether it was CPR induced or not— was robustly challenged. The liver injury was relatively minor (Figure 8) and situated in close proximity to an undisplaced anterolateral fracture of the right 5th rib associated with bilateral rib cage fractures which were typical of CPR. The site of trauma in resuscitation compression of normal pliable livers against the spine is usually in the midline but it could be atypical in a cirrhotic rigid liver that is enlarged and encroaching the right thorax vulnerable to blunt trauma from CPR. The pathologists dismissed a resuscitation injury because the hepatic damage was off midline.
A presupposition of 3 l of abdominal haemorrhage, which was unobserved by the pathologists, may have unduly influenced a conclusion that the hepatic damage could only be antemortem and inflicted at the time of the police altercation when the blood circulation was functional. Therefore, CPR induced hepatic trauma was deemed to be untenable because a perimortem blood loss associated with circulatory collapse should be minimal. It is important to be mindful that primary therapeutic intervention may introduce pseudoevidence of trauma and compromise evidence of forensic significance. To consolidate the argument that hepatic trauma was not CPR induced, the pathologists suggested that a lack of bruising or bleeding in the fractured ribs was another sign of significant antemortem abdominal haemorrhage that preceded the terminal collapse, and ignored evidence of overlying pectoral, pericostal and substernal soft tissue contusions (Figure 9). A pH 7.4 and lactate value of 6.2 mmol/L measured at the hospital indicated existence of a significant circulating blood volume and cardiac output maintained by an effective CPR capable of inducing the liver injury, albeit with blood loss at a much delayed rate in the perimortem interval.
The hepatic damage, contrary to assertions by pathologists, was also too remote to have been produced by the right arm compressing the ribcage upon a fall to the ground at the time of the altercation with police. Furthermore, the injury on the unprotected right elbow point was minimal (Figures 2 and 3) and there were no other marks to substantiate a hard fall that could generate a blunt force impact sufficient to inflict trauma to the liver. The effect of alcohol intoxication and a neuropathic right hemiparesis may confound a proper assessment of the force generated by a hard push as captured on video. An impact to the abdomen during his terminal collapse [not captured on video] could not be ruled out completely and a surgical expert gave consideration to an earlier fall to the ground several minutes preceding the altercation with police.
The easy availability of postmortem peripheral blood samples as a sign of significant residual intravascular volume discounting exsanguination was not accepted by a pathologist who invoked intravenous fluid replacement as the explanation for it even though no fluids were infused. The lowered haemoglobin value compared to previous values was attributed to an acute 3 l blood loss by a pathologist even though the timeline was insufficient for such haematological shift and haemodilution could be ruled out. After medical records confirmed ascites in association with paraumbilical hernia, an initial ambiguity about 3 l of internal haemorrhage was downgraded by pathologists from exsanguinations to a lesser substantial volume causing hypovolaemic shock. Yet there was no evidence of autoregulatory increase in heart rate to maintain blood pressure and cardiac output in response to a hypovolaemic shock.
The congregation of experts reinforcing internal haemorrhage as an alternate cause of death rejected coronary stenosis as a proximate contributing factor in the death. An estimation of the coronary stenosis as 60% - 70% based on postmortem photographs (Figure 10) by pathologists and as 50% by a cardiac expert after examining microscopy slides (Figure 12) were considered very unlikely to have caused a cardiac death in the absence of an acute ischaemic event such as plaque disruption, coronary thrombosis or acute infarction or past myocardial scarring. However, it is known that a developing infarct may take 12 to 24 hours before it is identifiable and no acute myocardial infarct is discerned in 19%, no coronary thrombus in 30% and no plaque disruption, which is quite common in patients who die from unrelated causes, in 8% of cases [4].
In view of considerable controversy over the mechanism of a heart condition with so many variable clinicopathological presentations, a 75% coronary cross-sectional stenosis is generally accepted to affect cardiac perfusion and under normal circumstance defines sudden cardiac death from coronary artery disease [5]. It is well recognised that estimation of coronary stenosis is subjective and noted to be discrepant by as much as 30% among pathologists. It may be that coronary stenosis per se is not as important as a situational lethal mismatch between decreased perfusion of the heart and increased metabolic demand for oxygen and nutrients, and the effect of “steal syndrome” during vasodilatory response to myocardial ischemia. It is also well known that many elderly people with death defying coronary stenosis are able go about their daily life but then there are also individuals with mild coronary stenosis who succumb to an acute coronary event.
There is some misperception that pathologists who assess the cross-sectional lumen overestimate coronary stenosis while cardiologists who look at quantitative angiographic diameter tend to underestimate. Although both methods are valid and comparable, the confusion may stem from not realising how the percentage coronary stenosis is derived. An occlusion of the coronary lumen by 50% to 75% in diameter is equivalent to 75% to 95% narrowing in the cross-section respectively. A reasonable estimation of the degree of coronary stenosis during thanatopsy is possible by comparing with unaffected coronary lumen and take into consideration any scaffolding provided by coronary atherosclerosis. Pathologists routinely examine coronary arteries which have decreased intraluminal pressure after death and are aware of the artefactual collapse and coronary spasm undetectable after death. The estimation of coronary stenosis is later affected by artefacts introduced during formalin fixation and laboratory preparation of microscopy slides (Figure 12).
A narrow complex electrocardiogram (ECG) tracing in association with PEA was not factored in by pathologists when determining the cause of death. A return of spontaneous pulse had been reported and it was debatable whether there was a true absent pulse or pseudo PEA with a weak electromechanical activity. A roadside scene would be less than ideal for palpation of a weak pulse in a patient who might be in cardiogenic shock or cardiac arrest and to complicate matters there may be no palpable pulse with cardiac arrhythmia or ventricular fibrillation. A delay of some 15 minutes for the first cardiac rhythm strip when CPR was already in progress would mean that ventricular tachycardia or transient ventricular fibrillation with spontaneous cardioversion at the time of the terminal collapse could not be excluded. Meanwhile, the mechanism of death from loss of cardiac output and circulatory collapse due to a coronary event would be confounded by cerebral ischaemic-hypoxic complications with seizure and rapid loss of consciousness as witnessed.
A cardiac expert asserted that a narrow complex ECG tracing associated with PEA was incompatible with a coronary event on the basis that ventricular tachycardia or transient ventricular fibrillation cannot return to sinus rhythm without a cardiac output, and therefore must be due to hypovolaemia from severe haemorrhage at the outset. Although PEA may not be differentiated clinically, a narrow complex sinus rhythm associated with hypovolaemia would be consistent with a perimortem haemorrhage, estimated to be around 500 ml and no more than 1l at the end of life, from a resuscitation liver injury. The narrow complex rhythm strip associated with PEA somehow enabled completion of an antemortem internal haemorrhage picture even though it did not reflect the situation 15 minutes earlier at the time of the terminal collapse and in the intervening perimortem interval. The PEA hypothesis would have served as a valid jigsaw piece in the thanatopsy puzzle if only it were true that there was indeed no perimortem cardiac output within the timeline of the terminal collapse and CPR. A noisy breathing described by the first-aider would be consistent with the gross pulmonary oedema and suggest acute left ventricular failure in association with coronary artery disease.
Although there was a temporal link to the incident, it would not be pathologically possible to be sure at a criminal standard of proof that stress contributed to a coronary event. Acute emotional stress has been strongly associated with sudden cardiac death but a causal link has not been proven [5]. A pathologist would not be able to measure the degree of stress an individual may have suffered nor the reaction to the stress and neither isolate a particular stressful incident in a death surrounded by complex circumstances. A stressful situation may be tampered by alcohol intoxication and concentrations associated with serous toxicity and fatal outcome could have an aggravating effect on pre-existing coronary disease or cryptogenic alcoholic cardiomyopathy with no microscopic morphological evidence. Factors that might protect susceptible individuals from stress related sudden death remain unknown [5].
The injuries from an assault were deemed not significant to have caused or contributed to his death. The bruised injury to the left thigh (Figure 4) was consistent with moderate force from or against a linear object and subsequently attributed to a police baton strike. The probed directions of the two skin puncture wounds within the patterned injuries on the right lower leg (Figures 5 and 6) were incorrect in apposition for a dog bite and were attributed to mild force impact with jagged object at the scene of terminal collapse. The knee injuries were typical of collapsing to the ground surface.
A cause of death is a clinical opinion rather than a medical fact and it is common knowledge that given a diagnostic dilemma there may be conflicting views held by medical experts. Some of the medical opinions may be a product of clinical bias introduced by misplaced confidence or subconscious weighting of signs and symptoms to suit a diagnosis. It must be remembered that medical expert opinions derived from a study of documentary evidence may not be reliable without a full discourse with the prosecting pathologist or comparing with a firsthand examination in the flesh [6]. The blood stained ascites and blood clot in the case presented were not available for self-examination by pathologists and led to speculation of ruptured subcapsular haematoma or ruptured abdominal varix as a source of substantial blood loss volume to justify a cause of death from internal haemorrhage. Similarly, the task of estimating coronary stenosis by comparing with postmortem images may have been compromised by not examining the coronary artery in situ. Example of such pitfall for medical experts reliant on postmortem photographic evidence has been reiterated [6].
There is a risk of over interpretation by pathologists focussing on the “gatekeeper” role with an inherent high index of suspicion in the management of forensic cases. An open mind approach is necessary in forensic medicine to prevent misinterpretation of preconceived pathognomonic postmortem findings, especially when the circumstantial history is sketchy. The importance of recognising artefacts in forensic medicine, including resuscitation injuries and considering alternate explanations have been reiterated to prevent misinterpretation [6,7]. There should be an active exclusion of an innocent explanation of an injury such as CPR to avoid it being overlooked or misconstrued as evidence of a non-accidental injury [7]. A mistaken diagnosis of a criminal action that culminates in criminal prosecution and miscarriage of justice can only be detrimental to good practice in forensic medicine [7].
Forensic pathologist may sense an impact on a jury who might be preconditioned to the adage that two heads are better than one when muchness of medical experts and overrated medical opinions undermine less popular evidence-based opinion [8]. It can be a sad reality that a medical opinion may be given validity on the basis of the reputation and performance of the expert witness. Something like a court order for a pre-trial discussion of polemic medical opinions or a joint statement issued by the expert witnesses to resolve evidential uncertainty in contentious medical opinions could overcome a fundamental problem of communication between medical experts.
There is now a potential threat to contend with in legal proceedings as the ancient legal immunity protecting medical experts from law suits brought by disgruntled clients has been abolished retrospectively by a Supreme Court judgement in Great Britain. There are ethical guidelines developed for medical expert witnesses to help counter criticisms such as giving misleading evidence or failure to disclose information [9]. There may remain a misunderstanding between doctors and lawyers regarding expectations from medical witnesses.
4. CONCLUSIONS
The alternate cause of death from internal haemorrhage favoured by congregation of medical experts may have been a product of esoteric inferences and speculations and not entirely evidence based. An internal haemorrhage from an assault causing death is bound to be classified as homicide and the burden of proof should be at a level of beyond reasonable doubt. A threshold of proof for medical experts has to be higher than 51% balance of probability applied in non-criminal cases to validate medical opinions and based on objective evidence for:
• the fall to the ground at the time of assault to cause antemortem trauma to the liver;
• a major hepatic trauma or indeed another cause for a fatal internal haemorrhage to occur within the restrictive time line;
• the hepatic trauma to be capable of a lesser volume of haemorrhage that would precipitate collapse within the restrictive time line;
• the volume of abdominal blood to be about 3 l;
• the free blood in the ascites to be antemortem;
• the coronary artery disease to be non-precipitant of the terminal collapse from an acute coronary event;
• the PEA with narrow complex rhythm to indicate hypovolaemia sustained in the restrictive time line before a CPR induced liver injury;
• stress to contribute morbidly to an acute coronary event because of a temporal link.
At the inquest, a jury was persuaded to reject acute coronary event and accept internal haemorrhage as a cause of death and returned a verdict of unlawful killing. There is perhaps a risk at inquisitorial hearings that evidence may be extracted on the sly for the purposes of an adversarial system and legal concept may not get at the whole truth based on scientific principles. Subsequently a manslaughter charge followed and the accused was acquitted after a criminal trial.
5. DISCLAIMER
The case is presented from a perspective of the author with expectation of insightful response from esoteric readers with interest in continuing professional development, and comparable photoimages of trauma in cirrhotic livers associated with ascites and intraabdominal haemorrhage.
6. ACKNOWLEDGEMENTS
The author thanks all past and present mentors, colleagues, coroners, coroners’ officers, pathologists and mortuary staff, crime scene investigators, bereaved family and friends for their unreserved good will and moral support.
![]()
![]()
REFERENCES
- Patel, F. (2008) Nobody wants a third-class thanatopsy in the Coroner’s jurisdiction. The Bulletin of the Royal College of Pathologists, 143, 216-272.
- Patel, F. (1991) Over my dead body: Coroner’s case. British Journal of Hospital Medicine, 46, 11.
- Home Office Policy Advisory Board for Forensic Pathology and the Royal College of Pathologists (2004) The pathologist and the defence. In: Code of Practice and Performance Standards for Forensic Pathologists, Home Office and the Royal College of Pathologists, London, 21.
- Norris, R. (2000) Coronary disease: The natural history of acute myocardial infarction. Heart, 83, 726-730. doi:10.1136/heart.83.6.726
- Lecomte, D., Fornes, P. and Nicolas, G. (1996) Stressful events as a trigger of sudden death: A study of 43 medicolegal autopsy cases. Forensic Science International, 79, 1-10. doi:10.1016/0379-0738(95)01873-5
- Patel, F. (2003) Artefact in forensic medicine: Pseudoscalloped gunshot wound. Journal of Clinical Forensic Medicine, 10, 17-20. doi:10.1016/S1353-1131(02)00161-X
- Patel, F. (1992) Childhood iatrogenic oral injury. Police Surgeon, 41, 8-9.
- Patel, F. (2000) Restraint asphyxia (CUSTOD syndrome). American Journal of Forensic Medicine and Pathology, 21, 196-197. doi:10.1097/00000433-200006000-00021
- General Medical Council (2008) Acting as an expert witness: Guidance for doctors. http://www.gmc-uk.org/guidance