Case Reports in Clinical Medicine
Vol. 2 No. 4 (2013) , Article ID: 34066 , 3 pages DOI:10.4236/crcm.2013.24063
A case of botulinum toxin injections for the management of chronic 3rd and 4th nerve palsies
![]()
Department of Ophthalmology, School of Medicine, Kyungpook National University, Daegu, South Korea; *Corresponding Author: byjun424@hotmail.com
Copyright © 2013 Kyoung Min Kang, Bo Young Chun. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 7 April 2013; revised 7 May 2013; accepted 10 June 2013
Keywords: Botulinum Toxin Injection; Oculomotor Nerve Palsy; Trochlear Nerve Palsy
ABSTRACT
A 66-year-old female presented with exotropia and hypertropia of her left eye. She had a previous history of lateral rectus recession and medial rectus resection of her left eye 20 years prior to old oculomotor and trochlear nerve pareses. She was treated with a botulinum toxin injection in the inferior oblique and lateral rectus muscles of her affected eye. In this case, the patient’s exotropia and hypertropia of her affected eye were greatly reduced after injections. Botulinum toxin chemodenervation can be considered as a subsidiary treatment option to the ultimate surgery not only for acute paralytic strabismus but also for chronic paralytic strabismus and further study may be necessary.
1. INTRODUCTION
Botulinum toxin injections have been used for the treatment of oculomotor and abducens pareses if the deficit is of recent origin [1], and research investigating the use of this toxin for trochlear nerve palsy treatment is limited [2-5]. In this case, the patient’s exotropia and hypertropia of her affected eye due to her chronic oculomotor and trochlear nerve palsies improved greatly after the botulinum toxin injections.
2. CASE REPORT
A 66-year-old female was referred to our clinic for the management of residual exotropia and hypertropia following a surgery in her left eye at the age of 46. She had been diagnosed with oculomotor and trochlear nerve palsies of the left eye after a traffic accident at the age of 45. One year later, she underwent 10 mm of lateral rectus (LR) recession and 8 mm of medial rectus (MR) resection of the left eye at another clinic. The details of her ocular deviation after the surgery were not known because her medical records were unavailable.
Visual acuity was 20/20 in both eyes. In the primary position, the patient showed 50 PD of exotropia and 35 PD of hypertropia in the left eye by Krimsky test (Figure 1). Hypertropia was present in every field of gaze due to the spread of comitance. Adduction of the left eye was limited (−2) on the duction test. Depression of the eye was limited (−4) in the primary position, adduction and abduction. There was secondary overaction of the inferior oblique (IO) (+1 ~ +2) and LR (+2) muscles. The Bielshowsky test was positive with left tilting and she was tilting her head slightly to right. During fundus exam, excyclotorsion (+2) of her left eye was observed. The patient was diagnosed with old oculomotor and trochlear nerve palsies with a previous history of unilateral LR recession and MR resection of her left eye.
After her informed consent, botulinum toxin (Botox® Allergan, USA) was injected into her IO and LR muscles. Author injected 2 ml of normal saline into the one bottle of botulinum toxin to make the concentration of 5 unit/0.1ml. After topical anesthesia, author made the traction suture to expose inferolateral part of the eyeball. After measuring 10 mm from the limbus using calipers,

Figure 1. The preoperative 9-cardinal pictures of the patient are shown.
author injected 5 units of botulinum toxin into the muscle belly of the IO according to the method described by Bagheri and Eshaghi [5]. The patient was instructed to look superiorly in adduction. With the bevel of the needle toward the sclera, the needle was introduced into the conjunctiva 10 mm from the limbus and advanced 10 mm inferotemporally to reach the belly of the inferior oblique muscle. The body of the syringe was then rotated approximately 30 degrees upward to move the needle away from the sclera and toward the belly of the muscle. To decrease hemorrhaging from the injection site, author used a 30-gauge needle and removed the needle slowly.
Then, author made a conjunctival incision at the site of the previous insertion of the LR. Author explored and found the stump of the previously recessed LR and conducted a forced duction test to make sure the grasped tissue was the previously recessed LR. An injection of 5 units of botulinum toxin to the LR and the conjunctival closure was conducted. All procedures were done without using electromyogram (EMG) localization due to the fact that our clinic was not equipped with EMG. The patient was told to sit instead of lying down after injection. One hour later, a fundus examination was performed, intraocular pressure was measured, and there was no sign of scleral perforation or retrobulbar hemorrhage.
After 2 weeks, the patient’s head tilt disappeared. In the primary position, she showed 15 PD of exotropia and 10 PD of hypertropia in the left eye by Krimsky method (Figure 2). Secondary overaction of the IO and LR muscles had disappeared. However, depression was still limited in the primary position, adduction and abduction in the affected eye. The patient had intermittent diplopia, which disappeared at postoperative 1 month. Alignment of her eyes after botulinum toxin injection was maintained for six months after injection. In the primary position, she showed 20 PD of exotropia and 10 PD of hypertropia in the left eye by Krimsky test (Figure 3).
3. DISCUSSION
Botulinum toxin chemodenervation is widely used for the treatment of acute paralytic strabismus, however, studies using botulinum toxin for the treatment of chronic paralytic strabismus are rare [1,6]. In this case,
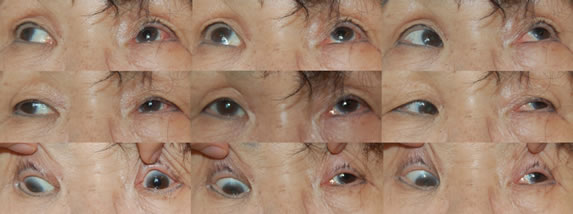
Figure 2. The postoperative 9-cardinal pictures of the patient two weeks after the botulinum toxin injections.

Figure 3. The postoperative pictures of the patient 6 months later after the botulinum toxin injections.
the author administrated botulinum toxin to a patient with old oculomotor and trochlear palsies, who had already undergone unilateral LR recession and MR resection, instead of planning surgery.
To correct her exotropia and hypertropia, botulinum toxin injection of the IO and LR muscles of her affected eye was determined to be the most favorable treatment for her oculomotor and trochlear nerve pareses. To prevent upper lid ptosis, we injected the botulinum toxin to the IO muscle instead of the SR muscle of the affected eye.
The amount of deviation corrected by a single injection of botulinum toxin (5 units/0.1ml to each muscle) into the IO and LR muscles was 35 PD of exotropia and 25 PD of hypertropia. In this case, considering her oculomotor and trochlear nerve palsies have existed for 20 years, the patient and the author were satisfied with the effect of botulinum toxin for her chronic paralytic strabismus.
The effect of botulinum toxin in acute paralytic strabismus is caused by avoiding the contracture of the antagonist muscle until the function of the paralyzed muscle returns [1]. However, this cannot explain the therapeutic effect of botulinum toxin in chronic strabismus. It is likely that the therapeutic effect of botulinum toxin in cases of chronic strabismus is produced by the simultaneous influence on both the peripheral and central nervous system [7].
This patient responded well to a botulinum toxin injection to her IO and LR muscles and an acceptable cosmetic result was attainable. No adverse effects attributable to botulinum toxin injection, such as retrobulbar hemorrhage, scleral perforation or ptosis of upper lid, were encountered in this case. The patient’s exotropia and hypertropia improvement began one week after injection and was maintained for six months after the injection.
This is the first case report which evaluated the effect of botulinum toxin injection to IO muscle to the patient with chronic trochlear nerve palsy without EMG guidance.
In conclusion, botulinum toxin chemodenervation can be considered as a subsidiary treatment option to the ultimate surgery not only for acute paralytic strabismus but also for chronic paralytic strabismus and further study may be necessary.
![]()
![]()
REFERENCES
- Von Noorden, G.K. and Campos, E.C. (2002) Binocular vision and ocular motility. 6th Edition, CV Mosby, St. Louis, 562-563.
- Lozano-Pratt, A. and Estanol, B. (1994) Treatment of acute paralysis of the fourth cranial nerve by botulinum toxin A chemodenervation. Binocul Vis Strabismus Q, 9, 155-158.
- Buonsanti, J.L., Riverosanchez-Covisa, M.E., Scarfone, H. and Lynch, J. (1996) Botulinum toxin chemodenervation of the inferior oblique muscle for chronic and acute IV nerve palsies; results in 15 cases. Binocul Vis Strabismus Q, 11, 119-124.
- Merino, P., Gomez, L.P., Garcia, C., Bartolome, G., Rodriguez, C. and De Juan, L. (2004) Bilateral superior oblique palsy and botulinum toxin. Archivos de la Sociedad Española de Oftalmología, 79, 119-124.
- Bagheri, A. and Eshaghi, M. (2006) Botulinum tosin injection of the inferior oblique muscle for the treatment of superior oblique muscle palsy. Journal of AAPOS, 10, 385-388. doi:10.1016/j.jaapos.2006.06.014
- Han, S.H., Jung, J.G. and Lew, H. (2000) The effect of botulinum toxin denervation in chronic paralytic strabismus. Journal of the Korean Ophthalmological Society, 41, 751-757.
- Ashton, A.C. and Dolly, J.O. (1988) Characterization of the inhibitory action of botulinum neurotoxin type A on the release of several transmitters from rat cerebrocortical synaptosomes. Journal of Neurochemistry, 50, 1808-1816. doi:10.1111/j.1471-4159.1988.tb02482.x

