Case Reports in Clinical Medicine
Vol.1 No.2(2012), Article ID:25508,3 pages DOI:10.4236/crcm.2012.12002
Laser vision correction for patients with atypical topography of cornea, LASIK vs. PRK: A review
![]()
Clinical Associate Professor, University of Hawaii, Honolulu, USA; mingchen@hawaii.rr.com
Received 19 October 2012; revised 22 November 2012; accepted 1 December 2012
Keywords: Refractive Laser Surgery; PRK; LASIK; Atypical Topography; Cornea Ectasia; Keratoconus
ABSTRACT
Purpose: To search evidence and determine whether PRK (Photo Refractive Keratectomy) or LASIK (Laser in Situ Keratomileusis) produce a better outcome of laser vision correction for patients with atypical topography of cornea. Setting: Electronic search of laser vision correction related studies on Cochrane Library, Medline and PubMed. Method: The search was conducted over Cochrane Library, Embase, PubMed and Medline using the key words of refractive laser surgery, PRK, LASIK, Atypical topography, cornea ectasia and Keratoconus from 1980 to 2012. Boolean operators were used to search in electronic data bases of related studies. The combining words used here were And, OR. Result: The best corrected vision decreased for those eyes with atypical topography that were treated with either PRK or LASIK. However, in the comparison of the outcomes of vision and ectasia, PRK outperformed LASIK. Conclusion: There is possible risk of developing corneal ectasia in those patients who desire laser vision correction with atypical topographic cornea. PRK may be a safer procedure when compare to LASIK for those patients.
1. INTRODUCTION
Laser vision correction of refractive errors for glasses independence is one of the most effective surgical procedures today. Most surgeon and patients prefer laser in situ Keratomileusis (LASIK) over photorefractive keratectomy (PRK) due to a faster recovery rate. Topographic examinations usually use the Pentacam (Oculus, German). If eyes show an elevation (float) in the posterior cornea, this is referred as atypical topography, which is a risk factor for corneal ectasia [1]. Corneal ectasia is a serious complication similar to Keratoconus which cause decreasing corrected distance visual acuity (CDVA). This complication can occur after PRK or LASIK and is more common in eyes with certain risk factors, such as inferior topographic steepening and posterior cornea float. This study aims to search evidence and determine whether PRK or LASIK produce a better outcome of laser vision correction for patients with atypical topography of cornea.
However, corneal ectasia can occur in eyes without known risk factors [1]. There is lack of a clear understanding of whether atypical topography of cornea represents irregularity of cornea or is one of the early signs that the cornea may be progressively worsening.
Keratoconus is a bilateral, nonsymmetrical corneal disorder associated with loss of tensile strength and thinning and protrusion of the central or paracentral cornea. The prevalence of Keratoconus in the general population is estimated to be about 4 to 600 per 100,000.
A major concern about refractive surgery in patients with corneal atypical topography is that it will cause more rapid progression of the ectasia or Keratoconus.
Preoperative topographic abnormalities, especially in younger patients as, are believed to be major determinants of stability in corneal curvature after corneal refractive surgicalprocedures [2].
Many eyes developed ectasia without any corneal surgery. There were also eyes with atypical topography had laser refractive surgeries showed no progression of corneal ectasia [3]. Conclusive diagnostic criteria are difficult to define. Nevertheless, topographic abnormalities such as low central corneal thickness, significant difference in corneal thickness between the two eyes, and corneal thinning in the mid or far periphery are considered warning signs.
Retrospective case control studies of patients with ectasia suggest the following risk factors for progression of ectasia after laser vision surgery:
1) Abnormal preoperative topography, 2) low residual bed thickness, 3) young age, 4) low preoperative corneal thickness, and 5) high myopia.
There were 4% to 8% of eyes that developed ectasia even though they were not identified as high risk while 6% to 9% of eyes had successful LASIK even though they were identified as high risk [2]. Therefore, patients can develop ectasia without having any proposed risk factors. LASIK in eyes with Keratoconus were reported to lead to progressive ectasia in a small percentage of cases. Of 208 eyes with high-risk characteristics for ectasia, 0.96% developed ectasia after LASIK (H.K. Wu, MD, “Safety and Efficacy of LASIK in Patients with Forme Fruste Keratoconus and Other High-Risk Criteria”, presented at the joint meeting of the International Society of Refractive Surgery and the American Academy of Ophthalmology, Las Vegas, Nevada, USA, November 2006). However, ectasia has also been reported after PRK [4].
2. METHOD
The search was conducted over Cochrane Library, Embase, PubMed and Medline using the key words of refractive laser surgery, PRK, LASIK, Atypical topography, cornea ectasia and Keratoconus from 1980 to 2012. Boolean operators were used to search in electronic data bases of related studies. The combining words used here were And, OR.
3. RESULTS
There were no results from Cochrane Library and Embase. PubMed had 1651 articles and Medline had 554 articles.
There were three case control studies to demonstrate the risk factors and outcome measurements of treatment as shown in Table 1.
The Table 1 below demonstrates the results from the three case control studies according to PICO (Population, Intervention, Control, Outcome measure) for the question of whether PRK or LASIK produce better outcomes of laser vision correction for patients with atypical topography of cornea. It showed eyes that underwent LASIK procedures suffered more decreased vision and more ectasia compared to PRK.
4. DISCUSSION
The weakness of this study was that there were neither randomized control studies nor systematic review available for this study. There were only three case control studies and a few case series. Case reports were available through the search and they were selected because their results were contributory.
LASIK was more commonly performed than PRK and this may be a reason why more ectasia were reported after LASIK. There are fewer reported cases of ectasia after PRK than after LASIK. Therefore, it is unclear whether there was true lower frequency of PRK causing ectasia, or it was under reported. For example, some surgeons would consider performing PRK in eyes they might not perform LASIK. Several studies reported good intermediate and long-term refractive outcomes and corneal stability after PRK in these eyes [7]. One patient with abnormal topography had PRK in the right eye and LASIK in the left eye; only the left eye developed progressive ectasia [8]. This patient had atypical topography with inferior steepening in the right eye that was slightly greater than in the left eye. Recent studies also showed that customized photorefractive surgery is effective in improving topographic indices and vision in mild to moderate Keratoconus by customizing the ablation of the cornea [7]. These treatments also do not appear to worsen ectasia.
5. CONCLUSION
It is necessary to explain the risk of developing corneal ectasia and decreasing vision from either LASIK or PRN to those patients with atypical topography of cornea. PRK may be the preferred procedure for those patients. However, a long-term, large population, prospective control trial is needed to confirm that outcomes after
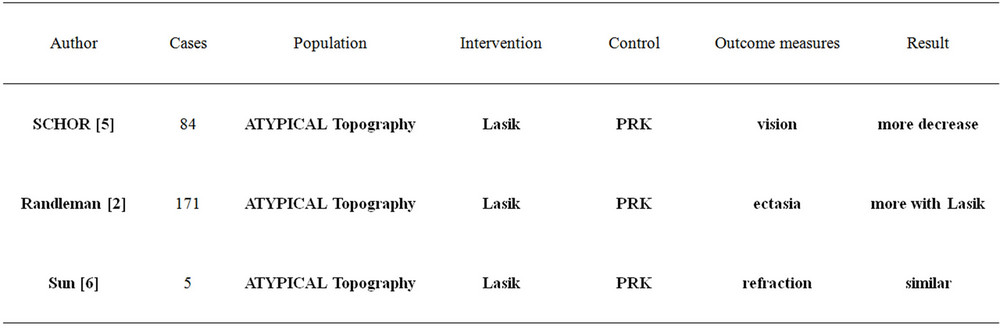
Table 1. Three case control studies according to PICO.
PRK are better than LASIK on those eyes with atypical topography.
REFERENCES
- Malecaze, F., Coullet, J., Calvas, P., Fournie, P., Arne, J.-L. and Brodaty, C. (2006) Corneal ectasia after photorefractive keratectomy for low myopia. Ophthalmology, 113, 742-746. doi:10.1016/j.ophtha.2005.11.023
- Randleman, J.B., Woodward, M., Lynn, M.J. and Stulting, R.D. (2008) Risk assessment for ectasia after corneal refractive surgery. Ophthalmology, 115, 37-50. doi:10.1016/j.ophtha.2007.03.073
- Li, X., Rabinowitz, Y.S., Rasheed, K. and Yang, H. (2004) Longitudinal study of the normal eyes in unilateral Keratoconus patients. Ophthalmology, 111, 440-446. doi:10.1016/j.ophtha.2003.06.020
- Parmar, D. and Claoue, C. (2004) Keratectasia following excimer laser photorefractive keratectomy. Acta Ophthalmologica Scandinavica, 82, 102-105. doi:10.1111/j.1395-3907.2003.0189b.x
- Schor, P., Beer, S.M.C., Da Silva, O., Takahashi, R. and Campos M. (2002) A clinical follow up of PRK and Lasik in eyes with preoperative abnormal corneal topographies. British Journal of Ophthalmology, 87, 682-685. doi:10.1136/bjo.87.6.682
- Sun, R., Gimbel, H.V. and Kaye, G.B. (1999) Photorefractive keratectomy in Keratoconus suspects. Journal of Cataract & Refractive Surgery, 25, 1461-1466. doi:10.1016/S0886-3350(99)00234-5
- Bahar, I., Levinger, S. and Kremer, I. (2006) Wavefrontsupported photorefractive keratectomy with the Bausch & Lomb Zyoptix in patients with myopic astigmatism and suspected Keratoconus. Journal of Refractive Surgery, 22, 533-538.
- Rao, S.K., Srinivasan, B., Sitalakshmi, G. and Padmanabhan, P. (2004) Photorefractive keratectomy versus laser in situ Keratomileusis to prevent Keratectasia after corneal ablation. Journal of Cataract & Refractive Surgery, 30, 2623-2628. doi:10.1016/j.jcrs.2004.09.037

