International Journal of Otolaryngology and Head & Neck Surgery
Vol.06 No.04(2017), Article ID:77967,20 pages
10.4236/ijohns.2017.64007
Parathyroid Embryology, Anatomy, and Pathophysiology of Primary Hyperparathyroidism
Rodrigo Arrangoiz*, Fernando Cordera, David Caba, Manuel Muñoz Juárez, Eduardo Moreno, Enrique Luque
American British Cowdray Medical Center, México City, Mexico

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: June 1, 2017; Accepted: July 24, 2017; Published: July 27, 2017
ABSTRACT
Unregulated overproduction of parathyroid hormone (PTH) from an abnormal parathyroid gland is the origin of primary hyperparathyroidism (PHPT). Patients who have an elevated serum calcium concentration have a problem in one or more of their parathyroid glands. To understand this disease state adequately and provide appropriate treatment, a thorough understanding of parathyroid embryology, anatomy, physiology, and pathophysiology is essential. In this manuscript, we review our current understanding of parathyroid gland embryology, anatomy, histology, physiology, and pathophysiology.
Keywords:
Parathyroid Anatomy, Parathyroid Histology, Parathyroid Pathophysiology

1. Embryology of the Parathyroid Glands
During the fifth to sixth week of intrauterine development, the embryonic pharynx is marked externally by four branchial clefts of ectoderm origin and internally by five branchial pouches of endoderm origin [1] . The branchial apparatus is made up by the branchial clefts and branchial pouches, together with the branchial arches of mesoderm origin, found in between them [2] . This apparatus undergoes normal involution leaving behind some derivatives which include the thyroid gland, parathyroid glands, thymus, ultimobranchial body, Eustachian tube, middle ear, and external auditory canal [3] .
The parathyroid glands develop as epithelial thickenings of the dorsal endoderm of the third and fourth branchial pouches [2] . The superior parathyroid glands are derived from the fourth branchial pouch, which also gives rise to the thyroid gland [4] . The third branchial pouch gives rise to the inferior parathyroid glands and the thymus [2] [5] . The parathyroid glands remain intimately connected with their respective branchial pouch derivatives.
The normal anatomic location of the superior parathyroid glands is more constant than the inferior parathyroid glands, with 80% of the superior glands being found near the posterior aspect of the thyroid gland at the junction of the upper and middle portion of the thyroid lobes, at the level of the cricoid cartilage (each gland with its own capsule of connective tissue) [6] . Roughly one percent of the superior parathyroid glands may be found in the paraesophageal or retroesophageal space [7] [8] . Enlarged superior glands may descend in the tracheoesophageal groove and come to lie below the inferior parathyroid glands [8] . Truly ectopic superior parathyroid glands are extremely rare, but may be localized to the middle or posterior mediastinum or in the aortopulmonary window [6] .
During intrauterine development, the thymus and the inferior parathyroid glands migrate caudally in the neck. The most common location for the inferior parathyroid glands is within a distance of 1 cm from a point centered where the inferior thyroid artery and the recurrent laryngeal nerve (RLN) cross [4] . Approximately 15% to 50% of the inferior glands are found in the thymus [6] [9] . The position of the inferior parathyroid glands, however, tends to be more variable due to their longer migratory route. Undescended inferior glands may be found near the skull base, angle of the mandible, or above the superior parathyroid glands along with an undescended thymus. The frequency of intrathyroidal glands is approximately 2% [4] [6] [10] .
2. Anatomy of the Parathyroid Glands
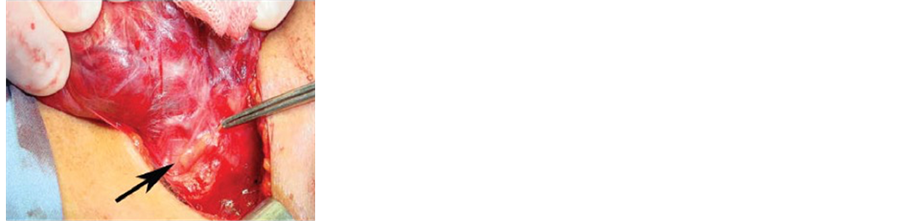
There are normally two pairs of parathyroid glands (inferior and superior). The parathyroid gland is oval or bean-shaped (Figure 1).
It typically measures 6 mm × 4 mm × 2 mm and weighs 40 mg to 60 mg [4] [6] [11] . Most people have four parathyroid glands. Akerström et al. [6] , in a series of 503 autopsies, identified four parathyroid glands in 84% of the cases. Supernumerary glands were found in 13% of the cases, most commonly in the thymus. In the literature, the incidence of supernumerary glands is anywhere between 3% and 13% [6] [12] . Only in three percent of the cases less than four parathyroid glands are identified [6] . The superior glands usually are dorsal to the
Figure 1. Arrow point to normal parathyroid gland.
RLN at the level of the cricoid cartilage, whereas the inferior parathyroid glands are located ventral to the nerve [4] [13] . The normal parathyroid glands are semitransparent and gray in color in newborns but appear golden yellow to light brown in adults [11] . The color of the parathyroid glands depends on several factors such as the cellularity, fat content, and vascularity. Also, they often are surrounded in and sometimes difficult to discriminate from surrounding fat.
The blood supply of the parathyroid glands is usually derived from branches of the inferior thyroid artery, although branches of the superior thyroid artery can supply at least 10% to 45% of the superior parathyroid glands [14] [15] . In a study of 354 autopsy specimens, Alverd, observed that both the superior and inferior parathyroid glands derive their blood supply from the inferior thyroid artery (86% on the right side and 77% from the left side) [16] . When the inferior thyroid artery was absent both the superior and inferior parathyroid glands were supplied by the superior thyroid artery [16] . Branches from the thyroidea ima, and vessels to the trachea, esophagus, larynx, and mediastinum may also contribute to the irrigation of the parathyroid glands [13] . Wang et al., in a study of 160 autopsy specimens showed that a low lying inferior parathyroid gland could be identified by following the vascular pedicle of the inferior thyroid artery [17] . The parathyroid glands drain ipsilaterally by the superior, middle, and inferior thyroid veins [6] [13] .
The innervation of the parathyroid glands occurs via the superior or middle cervical ganglia, or through a plexus in the fascia on the posterior aspect of the thyroid lobe [13] .
3. Histology of the Parathyroid Glands
The vast majority of the parathyroid gland parenchyma is composed of chief cells (also known the parathyroid gland principal cells) and oxyphil cells arranged in trabeculae, within a stroma composed primarily of adipose cells (Figure 2) [13] [18] . The parathyroid glands are surrounded by a thin fibrous capsule dividing the glands into lobules. The stromal fat around the parathyroid glands increases gradually with age up to 30% by age 25. The percentage of fat is related to the constitutional fat percentage, but can be reduced in dying individuals; mean is 17% with wide variation [19] .
Figure 2. Normal parathyroid gland.
In preadolescence the parathyroid glands are made uplargely by chief cells, which produce parathyroid hormone (PTH) (Figure 3) [20] . Acidophilic oxyphil cells which are rich in mitochondria, developed from parathyroid principal cells, can be identified after puberty, and increase in numbers during adulthood (Figure 4) [18] . The water-clear cells, also appear to come from the chief cells. They appear in small numbers, and have abundant glycogen (Figure 5). While most oxyphil and water-clear cells retain the ability to secrete PTH, their functional significance is not known.
The chief cells play a critical role in calcium homeostasis by sensing changes inextracellular calcium concentration and releasing the appropriate amount of PTH to correct or maintain normal blood calcium levels [21] . The chief cells (parathyroid gland principal cells) measure approximately six to eight microns, they are polygonal in shape, have a centrally located round nuclei, and have secretory granules containing PTH [18] . The chief cells appear dark purple in a hematoxylin and eosin stain [20] . Approximately 80% of the chief cells have
Figure 3. Chief cell or principal cell.
Figure 4. Oxyphil cell.
Figure 5. Water clear cell.
intracellular fat [22] . The chief cell is the most sensitive of all the parathyroid gland cells to changes in the serum ionized calcium concentrations. The chief cells spend most of their time inactive due to normal calcium hemostasis [22] . These inactive cells are categorized as cuboidal [21] . They have low levels of secretory granules, as opposed to active chief cells. These granules can contain acid phosphatase. Acid phosphatase is only found in larger secretory granules, and is less prevalent in smaller secretory granules. This acid phosphatase is also present in the Golgi apparatus of the chief cell [23] . However, the Golgi apparatus areas associated with PTH packaging contained little or no acid phosphatase [23] . The chief cells become active in response to low calcium serum concentrations. The low serum calcium concentrations are sensed by the calcium-sensing receptor [24] . These active cells have a greater electron density than the inactive chief cells that is thought to be caused by the secretory granules containing PTH [18] . The oxyphil cells are slightly larger than the chief cells, measuring approximately 12 microns, they have an acidophilic cytoplasm due to abundance of mitochondria, and they have no secretory granules [25] . On hematoxylin and eosin staining they appear lighter than the chief cells [20] . The mitochondrion of the oxyphil cells is the site for vitamin D metabolism. Vitamin D 1 hydroxylase is highly expressed in oxyphil cells [20] . The rough endoplasmic reticulum is scarce and the Golgi complex associated with few pro-secretory granules is poorly developed. They first appear during puberty as single cells, then pairs, then nodules by age 40 [26] . The oxyphil cells release PTH in a regulated fashion, and can also have the potential to produce autocrine/paracrine factors, such as parathyroid hormone related peptide (PTHrP) and calcitriol [20] .
The parathyroid gland water clear cells are extremely rare. Their presence is associated with parathyroid gland hyperplasia or even parathyroid adenoma formation [27] . The water clear cells have an abundant clear cytoplasm with sharply defined cell membranes, and have excessive cytoplasmic glycogen [21] . The water clear cells have an oval or round nucleus with occasional indentations. The cytoplasm is filled, for the most part, with membrane-limited vacuoles [27] . Most vacuoles appear empty or contain finely particulate substance and thread- like materials.
4. Parathyroid Gland Physiology, Calcium and Phosphate Homeostasis
Calcium homeostasis is a complex process involving the following four key components: serum calcium, serum phosphate, 1,25-dihydroxyvitamin D-3, and parathyroid hormone (PTH). The most abundant cation in the human body is calcium and it has many essential functions. The total body calcium concentration in a normal adult is approximately 1000 to 1200 grams [28] . Approximately 99% of the bodies calcium resides in the skeletal system and less than 1% of the soluble calcium is found in the intracellular and extracellular compartments [28] [29] . More than 99% of the total body calcium is found as the bone crystal structure of hydroxyapatite [29] . Calcium found at the bone crystal surface is exchangeable (1% of the calcium in the skeleton is freely exchangeable with calcium in the extracellular compartment) [29] . Extracellular calcium concentrations are 10,000-fold greater than the intracellular calcium concentrations [30] .
The main functions of extracellular calcium are for excitation-contraction coupling in muscle tissues, synaptic transmission in the nervous system, coagulation cascade, and secretion of other hormones [29] . Calcium found in the intracellular compartment act as a second messenger regulating cell division, motility, membrane trafficking, secretion, and intercellular adhesion [29] [31] [32] [33] .
In normal adults, approximately 800 to 1000 mg of calcium should be ingested daily. This amount will fluctuate depending on the amount of dairy product consumed. When 1000 mg of calcium are ingested in the diet, approximately 800 mg are excreted in the feces, and 200 mg in the urine [28] . Approximately 400 mg of the 1000 mg of dietary calcium are absorbed by the small intestines, and calcium loss by way of intestinal secretions is approximately 200 mg a day. Therefore, a net absorption of calcium is approximately 200 mg day [34] .
Calcium is absorbed throughout the entire small intestine, although it is more efficient in the duodenum and proximal jejunum secondary to the higher concentration of vitamin D dependent calcium binding proteins compared to other sites within the small intestines [35] . Another reason for the better absorption of calcium in the duodenum and proximal jejunum is the lower luminal pH in this segments that promote dissociation of calcium from food complexes. Larger proportions of total calcium are absorbed in the distal jejunum and ileum due to the longer contact times with the intestinal mucosa [35] [36] . Calcium absorption in the small intestine is mediated by two mechanisms: a transcellular active transport process, located mainly in the duodenum and proximal jejunum; and a paracellular, passive process that functions throughout the entire length of the small intestine, and it is the principal route of calcium absorption when serum calcium concentrations are high [34] [36] .
The active transcellular process comprises three major steps: entry of calcium across the intestinal brush border (mediated by a molecular structure termed CaT), intracellular diffusion (mediated by the cytosolic calcium-binding protein―calbindin D); and extrusion (mediated chiefly by the calcium ATPase) [35] [36] [37] [38] . Chyme travels through the lumen of the small intestine in approximately three hours, spending only a few minutes in the duodenum and proximal jejunum, but over two hours in the distal half of the small intestine [36] . When calcium consumption is low, active transcellular calcium transport accounts for a substantial fraction of the absorbed calcium [36] [37] . When calcium consumption is high, active transcellular transport accounts for only a small fraction of the absorbed calcium, because of the short transit time across the duodenum and proximal jejunum and because CaT1 and calbindin D, which are both rate-limiting, are down regulated when calcium intake is high [36] [37] [38] . The synthesis of calbindin D and CaT1 function is vitamin D-dependent in approximately 90% of the cases [37] . Many different factors affect intestinal calcium absorption and they are depicted on Table 1.
As mentioned previously extracellular compartment calcium (1000 mg) accounts for only 1% of the body’s calcium stores, the preponderance of which is found in the skeletal system. Roughly 50% of the serum calcium is in the ionized active form [40] . The remainder is bound to albumin (40%) and organic anions such as phosphate and citrate (10%) [40] [41] . The total serum calcium levels range from 8.5 to 10.5 mg/dL (2.1 to 2.6 mmol/L), and ionized calcium levels range from 4.4 to 5.2 mg/dL (1.17 to 1.33 mmol/L), but vary depending the laboratory used. The total serum calcium concentration must always be considered in its association to plasma protein concentrations, especially serum albumin. For each gram per deciliter of alteration of serum albumin above or below 4.0 mg/dL, there is a 0.8 mg/dL increase or decrease in protein-bound calcium and, thus, in total serum calcium levels [42] . For each 1.0 g/dl decrease in serum globulin fraction, total serum calcium decreases by 0.12 mg/dl [28] . For every 0.1 change in pH, ionized calcium changes by 0.12 mg/dl [28] [43] .
Certain acid-base and serum protein concentration disorders may affect the serum calcium concentrations. Metabolic acidosis, malnutrition, and cirrhosis will decrease serum calcium concentrations [44] [45] . Dehydration and multiple myeloma with increase serum calcium concentrations [46] .
In humans who have a glomerular filtration rate (GFR) of 170 liters a day approximately 10,000 mg of calcium are filtered in 24 hours [28] . Urinary calcium excretion is approximately 100 to 200 mg per day, therefore, 98% to 99% of the filtered calcium load is reabsorbed by the renal tubules (only 1% to 2% of the filtered calcium is been excreted) [30] . Roughly 60% to 70% of the filtered calcium is reabsorbed in the proximal convoluted tubule (PCT), 20% in the loop of Henle, 10% by the distal convoluted tubule (DCT), and 5% by the collecting duct (CD) [28] [33] . Table 2 exemplifies how much calcium is absorbed in the different anatomical sites of the kidney.
Table 1. Factors that affect intestinal calcium absorption [39] .
Table 2. Calcium reabsorption in kidney [28] .
The terminal nephron (DCT and CD), although responsible for the reabsorption of only 5% to 10% of the filtered calcium load, is the main site for regulating of calcium excretion [33] .
Vitamin D3 (cholecalciferol) is taken in the diet, from fortified dairy products and fish oils, or it is synthesized in the skin from 7-dehydrocholesterol by ultraviolet irradiation [47] . Vitamin D is produced by the result of photolysis of naturally occurring sterol precursors. Pro-vitamin D3 (7-dehydrocholesterol) is found in the cell membranes of epidermal keratinocytes. Ultraviolet B (UVB) light converts pro-vitamin D3 to pre-vitamin D3 by breaking the B ring. Thermal energy isomerizes pre-vitamin D3 to Vitamin D3 in the cell membrane.
Vitamin D3 is released into the blood stream from the epidermal keratinocytes and then it is transported to the liver via a vitamin D binding protein (DBP, a specific binding protein for vitamin D and its metabolites) [47] [48] . In the liver vitamin D metabolism occurs thanks to the hydroxylation by one or more cytochrome P450 vitamin D 25 hydroxylases (including CYP2R1, CYP2D11 and CYP2D25), resulting in the formation of 25-hydroxyvitamin D3 (25(OH)D3). It has been suggested that CYP2R1 is the key enzyme required for 25 hydroxylation of vitamin D since a homozygous mutation of the CYP2R1 gene was found in a patient with low circulating levels of 25(OH)D3 and classic symptoms of vitamin D deficiency [49] . The major circulating form of vitamin D, 25 hydroxy-vitamin D 3 (25(OH)D3), is transported by the DBP to the kidney [47] .
In the kidney, a member of the LDL receptor superfamily called Magalin, plays a critical role in endocytic internalization of 25(OH)D3 [50] . Proximal renal tubular cell 25(OH)D3 hydroxylase converts 25-hydroxyvitamin D3 (25(OH)D3) to active 1,25 (OH)2D3 (calcitriol) [47] . The cytochrome P450 monooxygenase 25(OH)D 1α hydroxylase (CYP27B1; 1α(OH)ase) which metabolizes 25(OH)D3 to 1,25(OH)2D3 is present predominantly in the kidney although it can be found in extra-renal sites including placenta, monocytes and macrophages [47] [51] [52] [53] . 25(OH)D3 hydroxylase is inhibited by1,25(OH)2D3 (calcitriol), phosphate, and elevated serum calcium concentrations. PTH stimulates 25(OH)D3 hydroxylase. Vitamin D stimulates the absorption of calcium and phosphate from the small intestine and the resorption of calcium from the bone, Table 3 depicts the actions of 1,25(OH)2D3 [47] .
The parathyroid gland cells depend on a G-protein?coupled membrane receptor (which is a 1078 amino acid glycosylated protein), designated the calcium- sensing receptor (CASR), to help regulate PTH secretion by sensing extracellular calcium concentrations [54] [55] . The CASR has seven large extracellular
Table 3. Actions of 1,25(OH)2D3 [47] .
transmembrane domains with a long cytoplasmic tail [54] . The ligand for the CASR is the calcium ion that when it binds to the receptor it inhibits PTH secretion [54] . PTH secretion is stimulated by low levels of 1,25(OH)2D3, catecholamine’s, and hypomagnesemia [56] .
The PTH gene is located on chromosome 11p15 that consists of three exons in the parathyroid gland cell nucleus [57] [58] . Exon 1 is untranslated, exon 2 encodes a 25-amino acid signal peptide and is part of the prohormone, and exon 3 encodes the remaining part of the prohormone (6 amino acids) and the whole PTH molecule (84 amino acids). In humans, the terminal region of exon 3 consisting of 351 nucleotides remains untranslated [59] .
PTH is synthesized in the parathyroid gland cell as a precursor hormone pre- pro-PTH (containing 115 amino acids), which is cleaved within the parathyroid gland cells at the N-terminal portion to pro-PTH (90 amino acids) and then to intact PTH (84 amino acids). The intact PTH molecule is the major storage, secreted, and biologically active form of the hormone [56] [60] . PTH synthesis and release is continuous, with about six to seven superimposed pulses each hour [60] .
Pre-pro-PTH DNA is transcribed from the PTH gene found in the parathyroid gland cell nucleus after which it passes into the cytoplasm and is translated in the rough endoplasmatic reticulum (RER) to form pre-pro-PTH (115 amino acids) [60] . The pre-peptide is cleaved across RER membrane and the pro- peptide is cleaved in Golgi Apparatus. The intact PTH is concentrated in secretory vesicles and granules [60] . Within the vesicles and granules, the PTH remains intact or is cleaved to form an inactive C-terminal PTH fragment. The intact PTH and C-terminal PTH fragments are released from the parathyroid cell by exocytosis [61] , this occurs within seconds after induction of hypocalcemia [60] . No N-terminal PTH fragments are released from the parathyroid gland cell [61] . The biosynthetic process is estimated to take less than one hour [60] . The N-terminal cleaved pre-sequence is rich in hydrophobic amino acids that are necessary for transport into the RER, while the basic pro-peptide directs accurate cleavage of pro-PTH into the mature 1 - 84 molecule [56] . The serum calcium concentration not only regulates the release but also the synthesis and degradation of PTH, in all its molecular forms as described latter on in the text [62] .
Secreted PTH has a half-life of approximately 2 to 4 minutes. In the liver, PTH is metabolized into the active N-terminal component and the relatively inactive C-terminal component. Approximately 70% of the PTH is metabolized in the liver by the Kupffer cells. The PTH is cleaved between AA 33 - 34 or 36 - 37 to form inactive C-terminal PTH fragments. The C-terminal component is excreted by the kidneys and accumulates in chronic renal failure. Less than 1% of the PTH reaches target organ receptors. The concentration of the C-terminal PTH fragment exceeds that of the intact PTH [61] . The N-terminal fragments constitute approximately 10% of circulating PTH fragments (Table 4) [63] . They are biologically active but have a short half-life (4 to 20 minutes) [60] . In con-
Table 4. N-terminal fragments [63] [64] .
Table 5. C-terminal fragments [63] .
Table 6. Circulating forms of PTH.
trast, the C-terminal fragments, which constitute 80% of the circulating PTH fragments, they have no biologic activity, and have a longer half-life, which is several fold-greater than the intact PTH (they are easier to measure in the plasma) (Table 5) [61] .
Overall, the intact hormone accounts for 10% of the circulating PTH-related peptides. Because multiple peptide products of PTH breakdown are present in the circulation (Table 6) [63] , determination of the intact molecule is the only reliable index of PTH levels.
In the normocalcemic patient, the PTH 1 - 84 (intact PTH) comprises 20% of the total circulating PTH molecules. This number increases to 33% in hypocalcemic patients, and decreases to 4% in the hypercalcemic patient [62] . During hypocalcemia, intracellular degradation of PTH decreases, and mostly intact PTH (1 - 84) is secreted; in comparison, during hypercalcemia mostly biologically inactive C-terminal fragments of PTH are secreted [62] [65] .
PTH acts by binding to and activating one of several types of PTH receptors [62] . In 1991, the PTH/PTH-related protein (PTHrP) receptor, otherwise known as PTH1R, was replicated [66] . This receptor is localized in the bone and kidney, and is also found in other tissues such as the skin, heart, breast, blood vessels, pancreas, and other organs that are not regarded as PTH target tissues [56] . The PTH1R binds intact PTH and biologically active N-terminal hormone fragments of PTH, such as PTH 1 - 34. The receptor recognizes both PTH and PTHrP due to the substantial degree of homology in the N-terminal parts of these two moieties.
The next PTH receptor that was identified was the PTH2 receptor (PTH2R), which selectively binds PTH but not PTHrP [56] . The PTH2R is found in the central nervous system, cardiovascular and gastrointestinal systems, as well as lung and testes, and may be implicated in the perception of pain [56] .
PTH1R activation triggers multiple cellular signaling pathways including cAMP, the PLC pathway, PKC, and release of intracellular calcium stores [56] [67] [68] [69] . The exact mechanism of action of how these intracellular signal transduction pathways ultimately stimulate bone resorption, renal tubular calcium reabsorption, or hydroxylation of vitamin D remains to be clarified.
The small intestine has no PTH/PTHrP receptors but it indirectly stimulates intestinal absorption of calcium and phosphate via the stimulation of renal synthesis of 1,25(OH)2D3 [35] [36] [47] .
The skeletal system is formed through the action of bone cells that are distributed sparsely throughout the bone tissue. The two main types of bone cells found in the human body are: osteoblasts and osteoclasts. These cells have opposite actions and the number of these cells is directly determined by the actions of certain 1 - 84 PTH, 7 - 84 PTH, vitamin D and estrogen [70] [71] .
Osteoblasts are expressed on the surfaces of all newly forming trabecular bone [72] . They are cuboidal cells that are located along the bone surface comprising 4% to 6% of the total resident bone cells and are largely known for their bone forming function [72] . When they are completely embedded in the osteoid, they are called osteocytes [73] . Osteocytes, which comprise 90% to 95% of the total bone cells, are the most abundant and long-lived cells, with a lifespan of approximately 25 years [73] . The osteoid is the collagen like scaffolding to which calcium and phosphorus deposit in the mineralization process. The function of the osteoblasts is to build bone and synthesize and secrete collagen fibrils [72] . The collagen strands combine to form osteoid. They also cause calcium salts and phosphorus to precipitate from the blood and bond with the newly formed osteoid to mineralize the bone tissueand is secreted during osteoblastic activity (bone formation) [74] .
Osteoclasts consume bone by producing enzymes which break down, or resorb mineralized bone [75] . Osteoclasts are located at the sites of bone formation where bone resorption occurs throughout the trabecular portion of bone. The only cells in the human body that can release calcium are the osteoclasts but they do not express PTH/PTHrP receptors [71] . PTH stimulates osteoblasts leading to an increase in the number and activity of the osteoclasts. PTH stimulates net bone resorption and the release of calcium from bone [76] .
Renal proximal convoluted tubular cell 1 alpha-hydroxylase converts 25(OH)D3 to 1,25(OH)2D3. PTH induces 1 alpha-hydroxylase synthesis by its action on the tubular cell PTH/PTHrP receptor. The PTH induced synthesis requires several hours and is blocked by 1,25(OH)2D3 [28] [42] [47] .
Approximately 90% to 95% of the inorganic phosphorus (Pi) in the circulation is filtered at the level of the glomerulus. Around seven grams of phosphorus are filtered by the kidney in 24 hours, of which 80% to 90% is reabsorbed by the renal tubules and the remainder is excreted in the urine (roughly 700 mg) equivalent to intestinal absorption [77] . Evidence has demonstrated that 60% to 70% of the filtered phosphorus is reabsorbed in the proximal tubule and there is also some evidence that a substantial amount of filtered phosphorus is reabsorbed in distal segments as well [78] . Increased bone resorption, stimulated by PTH, releases phosphate into the circulation. PTH reduces phosphate reabsorption in the proximal tubules more that the distal tubules [79] . PTH inhibits renal tubular cell sodium dependent phosphate cotransporter NPT-2 [80] .
5. Pathophysiology
Adverse clinical effects of PTH over production may be secondary to the hypercalcemia and/or hypophosphatemia caused by the hormone itself PTH or the additional effects of having an elevated hormone. Normal cellular function depends on tightly regulated serum ionized calcium concentration and, to a lesser extent, serum phosphate concentration. Increased levels of serum calcium in symptomatic PHPT may cause a wide range of organ dysfunctions. Symptoms include emotional lability, fatigue, irritability, depression, muscle pain, joint pain, bone pain, anorexia, nausea, vomiting, constipation, polydipsia, polyuria, nocturia, lethargy, headaches, insomnia, loss of memory, decrease concentration and, with extreme hypercalcemia, coma and death [81] . Severe elevations of circulating PTH dramatically increase osteoclastic bone resorption, culminating in “osteitis fibrosacystica”, the classic presentation of the disease, rarely seen today [82] .
Decrease levels in the extracellular calcium concentration normally lead to the secretion PTH from the parathyroid glands cells. PTH subsequently increases renal calcium reabsorption [28] [30] . It stimulates the hydroxylation of 25-hy- droxy-vitamin D at the proximal convoluted tubule in the kidney and increases bone resorption through stimulation of osteoclast-activating factors such as interleukin-6 from the osteoblasts [28] [83] . Through these actions PTH helps to restore calcium serum concentrations.
Our knowledge of calcium homeostasis has been advanced by the finding of the calcium sensing receptor that permits calcium to act with PTH and 1,25(OH)2D3 in maintaining calcium homeostasis [47] [84] . When extracellular calcium binds to the calcium sensing receptor in the parathyroid gland cell, PTH secretion and parathyroid cell growth are inhibited [18] . At the level of the kidneys this interaction between calcium and the calcium sensing receptor inhibits the 1-alfahy- droxylation of 25-hydroxy-vitamin D [33] . Serum calcium concentrations affect the thyroid parafolicullarcells, stimulating calcitonin release, and in bone may potentially regulate bone resorption [72] [85] [86] .
Increased urinary calcium excretion in PHPT can lead to nephrolithiasis [81] [82] . Why certain patients with PHPT develop hypercalciuria and nephrolithiasis and others with equivalent hypercalcemia do not, is not clearly understood. Some authors suggested that patients with nephrolithiasis represented a subgroup with higher serum 1,25(OH)2D3 causing increase intestinal calcium absorption have recently been questioned [82] [87] . Silverberg et al. [87] , showed evidence of cortical bone demineralization in patients with and without nephrolithiasis. Serum 1,25(OH)2D3, moreover, was not significantly higher in the subgroup with nephrolithiasis. Nephrocalcinosis, or ectopic calcification in other sites, appears to be uncommon in uncomplicated PHPT, and progressive reduction in renal function due to mild hypercalcemia has been documented in some studies [81] .
Two clinical diseases caused by mutations in the calcium sensing receptor gene have resulted in the confirmation of the key role that the calcium sensing receptor plays in calcium homeostasis [88] [89] . The first disease is benign familial hypocalciuric hypercalcemia, a heterozygous disease caused by an inactivating mutation of the calcium sensing receptor that results in a mild hypercalcemia and hypocalciuria [90] . The pathophysiology is a recalibration of the calcium sensing receptor leading to a higher set point required for inhibition of PTH secretion by the serum calcium concentrations, as well as impaired urinary calcium secretion. The renal abnormality persists following parathyroidectomy. The serum concentration of PTH tends to be normal or only slightly elevated in this condition [88] . The second disease state is that of an autosomal dominant activating mutation of the calcium sensing receptor [89] . The calcium sensing receptor is unusually sensitive to the serum calcium concentrations, leading to suppression of PTH secretion at hypocalcemic levels. This is a form of hypoparathyroidism with relative hypercalciuria.
In patients with PHPT mutations of the calcium sensing receptor gene have not yet been detected. Nonetheless, in parathyroid adenomas, a substantial fall in the calcium sensing receptor mRNA levels has been detected [91] . The exact pathophysiological significance of this observation is uncertain because the decreases in the mRA could be secondary to the hypercalcemia and not the primary etiology.
Approximately 5% to 10% of the cases of PHPT are family/hereditary [92] . These family forms are usually due to multiple endocrine neoplasia type I (MEN I) or to MEN type II. Isolated familial PHTP in the absence of other endocrine diseases also occurs. It has been shown recently that as many as 25% to 30% of people with sporadic PHPT can have abnormalities in the gene responsible for MEN I [93] [94] .
The pathophysiology PHPT can be summarized as a disorder of the cellular proliferation rate secondary to alterations of several genetic mechanisms with clonal loss or gain of function mutations, as clearly demonstrated by molecular genetic studies, and disorders of the extracellular calcium-dependent set-point that causes the loss of the normal feedback mechanism on PTH production and secretion by extracellular calcium concentrations [95] . Finally, a past medical history of external beam irradiation to the neck in childhood should also be taken into consideration [96] .
6. Conclusion
To understand PHPT and adequately treat it, a thorough knowledge of parathyroid embryology, anatomy, physiology, and pathophysiology is required. The clear majority of patients who have an elevated serum calcium level have a problem in one or more of their parathyroid glands. PHPT is becoming almost a 100% surgically treated disease so understanding of the basic science of the disease is essential for adequate outcomes.
Declaration of Interest
All authors have no special interest or conflict of interest to declare.
Funding
No funding was required for elaboration of the manuscript.
Cite this paper
Arrangoiz, R., Cordera, F., Caba, D., Juárez, M.M., Moreno, E. and Luque, E. (2017) Parathyroid Embryology, Anatomy, and Pathophysiology of Primary Hyperparathyroidism. International Journal of Otolaryngology and Head & Neck Surgery, 6, 39-58. https://doi.org/10.4236/ijohns.2017.64007
References
- 1. Frisdal, A. and Trainor, P.A. (2014) Development and Evolution of the Pharyngeal Apparatus. Wiley Interdisciplinary Reviews: Developmental Biology, 3, 403-418.
https://doi.org/10.1002/wdev.147 - 2. Grevellec, A. and Tucker, A.S. (2010) The Pharyngeal Pouches and Clefts: Development, Evolution, Structure and Derivatives. Seminars in Cell and Developmental Biology, 21, 325-332.
https://doi.org/10.1016/j.semcdb.2010.01.022 - 3. Mirilas, P. (2011) Lateral Congenital Anomalies of the Pharyngeal Apparatus: Part I. Normal Developmental Anatomy (Embryogenesis) for the Surgeon. American Journal of Surgery, 77, 1230-1242.
- 4. Fancy, T., Gallagher, D. 3rd, Hornig, J.D. (2010) Surgical Anatomy of the Thyroid and Parathyroid Glands. Otolaryngologic Clinics of North America, 43, 221-227.
https://doi.org/10.1016/j.otc.2010.01.001 - 5. Zou, D., Silvius, D., Davenport, J., et al. (2006) Patterning of the Third Pharyngeal Pouch into Thymus/Parathyroid by Six and Eya1. Developmental Biology, 293, 499-512.
https://doi.org/10.1016/j.ydbio.2005.12.015 - 6. Akerstrom, G., Malmaeus, J. and Bergstrom, R. (1984) Surgical Anatomy of Human Parathyroid Glands. Surgery, 95, 14-21.
- 7. LoPinto, M., Rubio, G.A., Khan, Z.F., et al. (2017) Location of Abnormal Parathyroid Glands: Lessons from 810 Parathyroidectomies. Journal of Surgical Research, 207, 22-26.
https://doi.org/10.1016/j.jss.2016.08.045 - 8. Phitayakorn, R. and McHenry, C.R. (2006) Incidence and Location of Ectopic Abnormal Parathyroid Glands. American Journal of Surgery, 191, 418-423.
https://doi.org/10.1016/j.amjsurg.2005.10.049 - 9. Uno, N., Tominaga. Y., Matsuoka, S., et al. (2008) Incidence of Parathyroid Glands Located in Thymus in Patients with Renal Hyperparathyroidism. World Journal of Surgery, 32, 2516-2519.
https://doi.org/10.1007/s00268-008-9739-x - 10. Goodman, A., Politz, D., Lopez, J., et al. (2011) Intrathyroid Parathyroid Adenoma: Incidence and Location—The Case against Thyroid Lobectomy. Otolaryngology—Head and Neck Surgery, 144, 867-871.
https://doi.org/10.1177/0194599811400366 - 11. Arrangoiz RaR, J.A. (2012) Parathyroid Carcinoma. In: Textbook of Uncommon Cancer, John Wiley & Sons, Inc., Hoboken, NJ.
- 12. Gomes, E.M., Nunes, R.C., Lacativa, P.G., et al. (2007) Ectopic and Extranumerary Parathyroid Glands Location in Patients with Hyperparathyroidism Secondary to End Stage Renal Disease. Acta Cirúrgica Brasileira, 22, 105-109.
https://doi.org/10.1590/S0102-86502007000200005 - 13. Skandalakis, J.E. (2004) Neck—Parathyroid Glands. Paschalidis Medical Publications, Athens, Greece.
- 14. Nobori, M., Saiki, S., Tanaka, N., et al. (1994) Blood Supply of the Parathyroid Gland from the Superior Thyroid Artery. Surgery, 115, 417-423.
- 15. Delattre, J.F., Flament, J.B., Palot, J.P., et al. (1982) [Variations in the Parathyroid Glands. Number, Situation and Arterial Vascularization. Anatomical Study and Surgical Application]. Journal de Chirurgie (Paris), 119, 633-641.
- 16. Alveryd, A. (1968) Parathyroid Glands in Thyroid Surgery. I. Anatomy of Parathyroid Glands. II. Postoperative Hypoparathyroidism—Identification and Autotransplantation of Parathyroid Glands. Acta Chirurgica Scandinavica, 389, 1-120.
- 17. Wang, C. (1976) The Anatomic Basis of Parathyroid Surgery. Annals of Surgery, 183, 271-275.
https://doi.org/10.1097/00000658-197603000-00010 - 18. Bilezikian, J. (2015) The Parathyroids: Basic and Clinical Concepts. Academic Press, San Diego.
- 19. Dufour, D.R. and Wilkerson, S.Y. (1982) The Normal Parathyroid Revisited: Percentage of Stromal Fat. Human Pathology, 13, 717-721.
https://doi.org/10.1016/S0046-8177(82)80293-1 - 20. Ritter, C.S., Haughey, B.H., Miller, B., et al. (2012) Differential Gene Expression by Oxyphil and Chief Cells of Human Parathyroid Glands. The Journal of Clinical Endocrinology and Metabolism, 97, E1499-E1505.
https://doi.org/10.1210/jc.2011-3366 - 21. Chen, H., Senda, T., Emura, S. and Kubo, K. (2013) An Update on the Structure of the Parathyroid Gland. The Open Anatomy Journal, 5, 1-9.
https://doi.org/10.2174/1877609401305010001 - 22. Rosai, J. (2004) Parathyroid Glands. Mosby, New York.
- 23. Shannon Jr., W.A. and Roth, S.I. (1974) An Ultrastructural Study of Acid Phosphatase Activity in Normal, Adenomatous and Hyperplastic (Chief Cell Type) Human Parathyroid Glands. The American Journal of Pathology, 77, 493-506.
- 24. Thomas, J. (1997) Endocrine Toxicology. CRC Press, Washington DC.
- 25. Altenahr, E. (1972) Ultrastructural Pathology of Parathyroid Glands. In: Altmann, H.W., et al., Eds., Current Topics in Pathology / Ergebnisse der Pathologie, Vol. 56, Springer, Berlin, Heidelberg, 1-54.
https://doi.org/10.1007/978-3-642-65324-7_1 - 26. Isono, H., Shoumura, S. and Emura, S. (1990) Ultrastructure of the Parathyroid Gland. Histology and Histopathology, 5, 95-112.
- 27. Roth, S.I. (1970) The Ultrastructure of Primary Water-Clear Cell Hyperplasia of the Parathyroid Glands. The American Journal of Pathology, 61, 233-248.
- 28. Blaine, J., Chonchol, M. and Levi, M. (2015) Renal Control of Calcium, Phosphate, and Magnesium Homeostasis. Clinical Journal of the American Society of Nephrology, 10, 1257-1272.
https://doi.org/10.2215/CJN.09750913 - 29. Neer, R., Berman, M., Fisher, L., et al. (1967) Multicompartmental Analysis of Calcium Kinetics in Normal Adult Males. The Journal of Clinical Investigation, 46, 1364-1379.
https://doi.org/10.1172/JCI105629 - 30. Bruder, J. (2001) Mineral Metabolism. McGraw-Hill Publishers, Inc., New York.
- 31. Bronner, F. (1994) Calcium and Osteoporosis. The American Journal of Clinical Nutrition, 60, 831-836.
- 32. Hebert, S.C. and Brown, E.M. (1996) The Scent of an Ion: Calcium-Sensing and Its Roles in Health and Disease. Current Opinion in Nephrology & Hypertension, 5, 45-53.
https://doi.org/10.1097/00041552-199601000-00009 - 33. Kumar, R. (1995) Calcium Metabolism. In: Jacobson, H.R., Striker, G.E. and Klahr, S., Eds., The Principles and Practice of Nephrology, Mosby-Year Book, St. Louis, MO, 964-971.
- 34. Johnson, J.A. and Kumar, R. (1994) Renal and Intestinal Calcium Transport: Roles of Vitamin D and Vitamin D-Dependent Calcium Binding Proteins. Seminars in Nephrology, 14, 119-128.
- 35. Bronner, F. (1987) Calcium Absorption. In: Johnson, L.R., Ed., Physiology of the Gastrointestinal Tract, 2nd Edition, Raven Press, New York, 1419-1435.
- 36. Bronner, F. (2003) Mechanisms of Intestinal Calcium Absorption. Journal of Cellular Biochemistry, 88, 387-393.
https://doi.org/10.1002/jcb.10330 - 37. Bronner, F. (2009) Recent Developments in Intestinal Calcium Absorption. Nutrition Reviews, 67, 109-113.
https://doi.org/10.1111/j.1753-4887.2008.00147.x - 38. Wasserman, R.H. (2010) Comments on the Essentiality of Calbindin-D9k and Calcium Channel TRPV6 for Optimal Active Intestinal Calcium Transport in Vitro. Annals of the New York Academy of Sciences, 1192, 365-366.
https://doi.org/10.1111/j.1749-6632.2009.05316.x - 39. Favus, M.J. (1985) Factors That Influence Absorption and Secretion of Calcium in the Small Intestine and Colon. American Journal of Physiology, 248, G147-G157.
- 40. Carr, M.H. and Frank, H.A. (1956) Improved Method for Determination of Calcium and Magnesium in Biologic Fluids by EDTA Titration. American Journal of Clinical Pathology, 26, 1157-1168.
https://doi.org/10.1093/ajcp/26.10.1157 - 41. Horner, W.H. (1955) The Determination of Calcium in Biologic Material. Journal of Laboratory and Clinical Medicine, 45, 951-957.
- 42. Bushinsky, D.A. and Monk, R.D. (1998) Electrolyte Quintet: Calcium. The Lancet, 352, 306-311.
https://doi.org/10.1016/S0140-6736(97)12331-5 - 43. Friedman, P.A. and Gesek, F.A. (1995) Cellular Calcium Transport in Renal Epithelia: Measurement, Mechanisms, and Regulation. Physiological Reviews, 75, 429-471.
- 44. Oberleithner, H., Greger, R. and Lang, F. (1982) The Effect of Respiratory and Metabolic Acid-Base Changes on Ionized Calcium Concentration: In Vivo and in Vitro Experiments in Man and Rat. European Journal of Clinical Investigation, 12, 451-455.
https://doi.org/10.1111/j.1365-2362.1982.tb02223.x - 45. Schafer, A.L. and Shoback, D.M. (2016) Hypocalcemia: Diagnosis and Treatment. In: De Groot, L.J., Chrousos, G., Dungan, K., et al., Eds., Endotext [Internet], MDText.com, Inc., South Dartmouth, MA.
- 46. Oyajobi, B.O. (2007) Multiple Myeloma/Hypercalcemia. Arthritis Research & Therapy, 9, S4.
https://doi.org/10.1186/ar2168 - 47. Christakos, S., Ajibade, D.V., Dhawan, P., et al. (2010) Vitamin D: Metabolism. Endocrinology and Metabolism Clinics of North America, 39, 243-253.
https://doi.org/10.1016/j.ecl.2010.02.002 - 48. Bikle, D.D., Siiteri, P.K., Ryzen, E., et al. (1985) Serum Protein Binding of 1,25-Dihydroxyvitamin D: A Reevaluation by Direct Measurement of Free Metabolite Levels. The Journal of Clinical Endocrinology and Metabolism, 61, 969-975.
https://doi.org/10.1210/jcem-61-5-969 - 49. Cheng, J.B., Levine, M.A., Bell, N.H., et al. (2004) Genetic Evidence That the Human CYP2R1 Enzyme Is a Key Vitamin D 25-Hydroxylase. Proceedings of the National Academy of Sciences of the United States of America, 101, 7711-7715.
https://doi.org/10.1073/pnas.0402490101 - 50. Nykjaer, A., Dragun, D., Walther, D., et al. (1999) An Endocytic Pathway Essential for Renal Uptake and Activation of the Steroid 25-(OH) Vitamin D3. Cell, 96, 507-515.
https://doi.org/10.1016/S0092-8674(00)80655-8 - 51. Weisman, Y., Harell, A., Edelstein, S., et al. (1979) 1α, 25-Dihydroxyvitamin D3 and 24,25-Dihydroxyvitamin D3 in Vitro Synthesis by Human Decidua and Placenta. Nature, 281, 317-319.
https://doi.org/10.1038/281317a0 - 52. Gray, T.K., Lester, G.E. and Lorenc, R.S. (1979) Evidence for Extra-Renal 1 Alpha-Hydroxylation of 25-Hydroxyvitamin D3 in Pregnancy. Science, 204, 1311-1313.
https://doi.org/10.1126/science.451538 - 53. Stoffels, K., Overbergh, L., Bouillon, R., et al. (2007) Immune Regulation of 1α-Hydroxylase in Murine Peritoneal Macrophages: Unravelling the IFNγ Pathway. The Journal of Steroid Biochemistry and Molecular Biology, 103, 567-571.
- 54. Nemeth, E.F., Steffey, M.E., Hammerland, L.G., et al. (1998) Calcimimetics with Potent and Selective Activity on the Parathyroid Calcium Receptor. Proceedings of the National Academy of Sciences of the United States of America, 95, 4040-4045.
https://doi.org/10.1073/pnas.95.7.4040 - 55. Ward, B.K., Magno, A.L., Walsh, J.P., et al. (2012) The Role of the Calcium-Sensing Receptor in Human Disease. Clinical Biochemistry, 45, 943-953.
- 56. Murray, T.M., Rao, L.G., Divieti, P., et al. (2005) Parathyroid Hormone Secretion and Action: Evidence for Discrete Receptors for the Carboxyl-Terminal Region and Related Biological Actions of Carboxyl-Terminal Ligands. Endocrine Reviews, 26, 78-113.
https://doi.org/10.1210/er.2003-0024 - 57. Levine, M.A., Morrow, P.P., Kronenberg, H.M., et al. (1986) Tissue and Gene Specific Hypomethylation of the Human Parathyroid Hormone Gene: Association with Parathyroid Hormone Gene Expression in Parathyroid Glands. Endocrinology, 119, 1618-1624.
https://doi.org/10.1210/endo-119-4-1618 - 58. Antonarakis, S.E., Phillips 3rd, J.A., Mallonee, R.L., et al. (1983) Beta-Globin Locus Is Linked to the Parathyroid Hormone (PTH) Locus and Lies between the Insulin and PTH Loci in Man. Proceedings of the National Academy of Sciences of the United States of America, 80, 6615-6619.
https://doi.org/10.1073/pnas.80.21.6615 - 59. Goswami, R., Mohapatra, T., Gupta, N., et al. (2004) Parathyroid Hormone Gene Polymorphism and Sporadic Idiopathic Hypoparathyroidism. The Journal of Clinical Endocrinology and Metabolism, 89, 4840-4845.
https://doi.org/10.1210/jc.2004-0273 - 60. Habener, J.F., Kemper, B.W., Rich, A., et al. (1976) Biosynthesis of Parathyroid Hormone. Recent Progress in Hormone Research, 33, 249-308.
- 61. MacGregor, R.R., Hamilton, J.W., Kent, G.N., et al. (1979) The Degradation of Proparathormone and Parathormone by Parathyroid and Liver Cathepsin B. Journal of Biological Chemistry, 254, 4428-4433.
- 62. D’Amour, P., Rakel, A., Brossard, J.H., et al. (2006) Acute Regulation of Circulating Parathyroid Hormone (PTH) Molecular Forms by Calcium: Utility of PTH Fragments/PTH(1-84) Ratios Derived from Three Generations of PTH Assays. The Journal of Clinical Endocrinology and Metabolism, 91, 283-289.
https://doi.org/10.1210/jc.2005-1628 - 63. D’Amour, P. (2006) Circulating PTH Molecular Forms: What We Know and What We Don’t. Kidney International, 70, S29-S33.
- 64. Shimizu, M., Potts Jr., J.T. and Gardella, T.J. (2000) Minimization of Parathyroid Hormone. Novel Amino-Terminal Parathyroid Hormone Fragments with Enhanced Potency in Activating the Type-1 Parathyroid Hormone Receptor. Journal of Biological Chemistry, 275, 21836-21843.
https://doi.org/10.1074/jbc.M909861199 - 65. Potts, J.T. and Juppner, H. (1996) Parathyroid Hormone: Molecular Biology and Regulation. In: Bilezikian, J.P., Raisz, L.G. and Rodan, G.A., Eds., Principles of Bone Biology, Academic Press, San Diego, 325.
- 66. Juppner, H., Abou-Samra, A.B., Freeman, M., et al. (1991) A G Protein-Linked Receptor for Parathyroid Hormone and Parathyroid Hormone-Related Peptide. Science, 254, 1024-1026.
https://doi.org/10.1126/science.1658941 - 67. Dunlay, R. and Hruska, K. (1990) PTH Receptor Coupling to Phospholipase C Is an Alternate Pathway of Signal Transduction in Bone and Kidney. American Journal of Physiology, 258, F223-F231.
- 68. Hruska, K.A., Moskowitz, D., Esbrit, P., et al. (1987) Stimulation of Inositol Trisphosphate and Diacylglycerol Production in Renal Tubular Cells by Parathyroid Hormone. The Journal of Clinical Investigation, 79, 230-239.
https://doi.org/10.1172/JCI112788 - 69. Abou-Samra, A.B., Jueppner, H., Westerberg, D., et al. (1989) Parathyroid Hormone Causes Translocation of Protein Kinase-C from Cytosol to Membranes in Rat Osteosarcoma Cells. Endocrinology, 124, 1107-1113.
https://doi.org/10.1210/endo-124-3-1107 - 70. Khosla, S., Oursler, M.J. and Monroe, D.G. (2012) Estrogen and the Skeleton. Trends in Endocrinology and Metabolism, 23, 576-581.
https://doi.org/10.1016/j.tem.2012.03.008 - 71. Calvi, L.M., Sims, N.A., Hunzelman, J.L., et al. (2001) Activated Parathyroid Hormone/Parathyroid Hormone-Related Protein Receptor in Osteoblastic Cells Differentially Affects Cortical and Trabecular Bone. The Journal of Clinical Investigation, 107, 277-286.
https://doi.org/10.1172/JCI11296 - 72. Capulli, M., Paone, R. and Rucci, N. (2014) Osteoblast and Osteocyte: Games without Frontiers. Archives of Biochemistry and Biophysics, 561, 3-12.
- 73. Franz-Odendaal, T.A., Hall, B.K. and Witten, P.E. (2006) Buried Alive: How Osteoblasts Become Osteocytes. Developmental Dynamics, 235, 176-190.
https://doi.org/10.1002/dvdy.20603 - 74. Anh, D.J., Dimai, H.P., Hall, S.L., et al. (1998) Skeletal Alkaline Phosphatase Activity Is Primarily Released from Human Osteoblasts in an Insoluble Form, and the Net Release Is Inhibited by Calcium and Skeletal Growth Factors. Calcified Tissue International, 62, 332-340.
https://doi.org/10.1007/s002239900441 - 75. Crockett, J.C., Mellis, D.J., Scott, D.I., et al. (2011) New Knowledge on Critical Osteoclast Formation and Activation Pathways from Study of Rare Genetic Diseases of Osteoclasts: Focus on the RANK/RANKL Axis. Osteoporosis International, 22, 1-20.
https://doi.org/10.1007/s00198-010-1272-8 - 76. Florencio-Silva, R., Sasso, G.R., Sasso-Cerri, E., et al. (2015) Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. BioMed Research International, 2015, Article ID: 421746.
https://doi.org/10.1155/2015/421746 - 77. Knox, F.G., Osswald, H., Marchand, G.R., et al. (1977) Phosphate Transport along the Nephron. American Journal of Physiology, 233, F261-F268.
- 78. Pastoriza-Munoz, E., Colindres, R.E., Lassiter, W.E., et al. (1978) Effect of Parathyroid Hormone on Phosphate Reabsorption in Rat Distal Convolution. American Journal of Physiology, 235, F321-F330.
- 79. Berndt, T. and Kumar, R. (2007) Phosphatonins and the Regulation of Phosphate Homeostasis. Annual Review of Physiology, 69, 341-359.
https://doi.org/10.1146/annurev.physiol.69.040705.141729 - 80. Caverzasio, J., Rizzoli, R. and Bonjour, J.P. (1986) Sodium-Dependent Phosphate Transport Inhibited by Parathyroid Hormone and Cyclic AMP Stimulation in an Opossum Kidney Cell Line. Journal of Biological Chemistry, 261, 3233-3237.
- 81. Arrangoiz, R., Cordera, F., Lamberton, F., Luque-de-Leon, E., Munoz-Juárez, M. and Moreno, E (2016) Current Thinking on Primary Hyperparathyroidism. JSM Head & Neck Cancer-Cases and Reviews, 1, 1002.
- 82. Broadus, A.E. (1982) Primary Hyperparathyroidism Viewed as a Bihormonal Disease Process. Mineral and Electrolyte Metabolism, 8, 199-214.
- 83. Grey, A., Mitnick, M.A., Shapses, S., et al. (1996) Circulating Levels of Interleukin-6 and Tumor Necrosis Factor-Alpha Are Elevated in Primary Hyperparathyroidism and Correlate with Markers of Bone Resorption—A Clinical Research Center Study. The Journal of Clinical Endocrinology and Metabolism, 81, 3450-3454.
- 84. Brown, E.M., Gamba, G., Riccardi, D., et al. (1993) Cloning and Characterization of an Extracellular Ca2+-Sensing Receptor from Bovine Parathyroid. Nature, 366, 575-580.
https://doi.org/10.1038/366575a0 - 85. Felsenfeld, A.J. and Levine, B.S. (2015) Calcitonin, the Forgotten Hormone: Does It Deserve to Be Forgotten? Clinical Kidney Journal, 8, 180-187.
https://doi.org/10.1093/ckj/sfv011 - 86. Brown, E.M., Pollak, M. and Hebert, S.C. (1998) The Extracellular Calcium-Sensing Receptor: Its Role in Health and Disease. Annual Review of Medicine, 49, 15-29.
https://doi.org/10.1146/annurev.med.49.1.15 - 87. Silverberg, S.J., Shane, E., Jacobs, T.P., et al. (1990) Nephrolithiasis and Bone Involvement in Primary Hyperparathyroidism. The American Journal of Medicine, 89, 327-334.
https://doi.org/10.1016/0002-9343(90)90346-F - 88. Attie, M.F., Gill Jr., J.R., Stock, J.L., et al. (1983) Urinary Calcium Excretion in Familial Hypocalciuric Hypercalcemia. Persistence of Relative Hypocalciuria after Induction of Hypoparathyroidism. The Journal of Clinical Investigation, 72, 667-676.
https://doi.org/10.1172/JCI111016 - 89. Baron, J., Winer, K.K., Yanovski, J.A., et al. (1996) Mutations in the Ca2+-Sensing Receptor Gene Cause Autosomal Dominant and Sporadic Hypoparathyroidism. Human Molecular Genetics, 5, 601-606.
https://doi.org/10.1093/hmg/5.5.601 - 90. Varghese, J., Rich, T. and Jimenez, C. (2011) Benign Familial Hypocalciuric Hypercalcemia. Endocrine Practice, 17, 13-17.
https://doi.org/10.4158/EP10308.RA - 91. Kifor, O., Moore Jr., F.D., Wang, P., et al. (1996) Reduced Immunostaining for the Extracellular Ca2+-Sensing Receptor in Primary and Uremic Secondary Hyperparathyroidism. The Journal of Clinical Endocrinology and Metabolism, 81, 1598-1606.
- 92. Pepe, J., Cipriani, C., Pilotto, R., et al. (2011) Sporadic and Hereditary Primary Hyperparathyroidism. Journal of Endocrinological Investigation, 34, 40-44.
- 93. Chandrasekharappa, S.C., Guru, S.C., Manickam, P., et al. (1997) Positional Cloning of the Gene for Multiple Endocrine Neoplasia-Type 1. Science, 276, 404-407.
https://doi.org/10.1126/science.276.5311.404 - 94. Mulligan, L.M., Kwok, J.B., Healey, C.S., et al. (1993) Germ-Line Mutations of the RET Proto-Oncogene in Multiple Endocrine Neoplasia Type 2A. Nature, 363, 458-460.
https://doi.org/10.1038/363458a0 - 95. Thakker, R.V. (2004) Diseases Associated with the Extracellular Calcium-Sensing Receptor. Cell Calcium, 35, 275-282.
- 96. Silverberg, S.J. and Bilezikian, J.P. (1997) Primary Hyperparathyroidism: Still Evolving? Journal of Bone and Mineral Research, 12, 856-862.
https://doi.org/10.1359/jbmr.1997.12.5.856