Surgical Science
Vol.09 No.09(2018), Article ID:87256,6 pages
10.4236/ss.2018.99034
OPCAB (Off Pump Coronary Artery Bypass) for Kawasaki Disease
Murali P. Vettath1, Madhu Ravisankar2, Kannan Arunachalam Veluchamy2, Nitin Gangadharan2
1Cardiovascular and Thoracic Centre, MEITRA Hospital, Kozhikode, India
2Department of Cardiovascular and Thoracic Surgery, MEITRA Hospital, Kozhikode, India

Copyright © 2018 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: May 28, 2018; Accepted: September 9, 2018; Published: September 12, 2018
ABSTRACT
We hereby report a case of Kawasaki disease in a 32 year old male, with giant aneurysm of both coronary arteries and severe LV (left ventricular) dysfunction who underwent OPCAB (off pump coronary artery bypass grafting) two years ago. He presented with acute myocardial infarction of his anterior wall of left ventricle. He was stabilised with medical management and was taken up for surgery when his enzymes became normal. His LV function had improved over the time and now has a good ejection fraction.
Keywords:
Coronary Artery Disease, Coronary Artery Aneurysm, Kawasaki Disease, OPCAB (Off Pump Coronary Artery Bypass)

1. Introduction
Kawasaki disease, or mucocutaneous lymph node syndrome, occurs predominantly in children and rarely in adults. Symptoms include acute vasculitis, mucosal inflammation, rash, cervical adenopathy, hand and foot swelling, and late fingertip desquamation. In the most severe cases, aneurysms develop in one or more coronary arteries. Kawasaki disease involving the coronary arteries and causing acute myocardial infarction (AMI) is a rare entity. We report a rare case of Kawasaki disease associated with multiple coronary artery aneurysms in a young adult who presented with heart failure and acute myocardial infarction. He was first medically managed with decongestive therapy and then taken up for OPCAB. His post-operative period was uneventful. His left ventricular function improved gradually and is now back work, with a good ejection fraction.
2. Case Report
A 32 year old male presented with severe LV (left ventricular) dysfunction and a history of acute anterior wall myocardial infarction (AWMI), 10 days ago, in gulf. His coronary angiogram (CAG) done showed, multiple giant aneurysms in both his coronary arteries. That is, in the left main coronary artery (LMCA) at its bifurcation, and in the right coronary artery (RCA). His LMCA aneurysm was compressing the trunk of circumfllex coronary artery. The flow through the aneurysm and to the distal LAD was minimal (Figure 1). The aneurysm in the RCA was not causing any flow limitation in the distal RCA (Figure 2). In view of his coronary lesions on the left side and severe LV dysfunction, he was taken up for off pump coronary artery bypass grafting, after stabilizing his hemodynamics. Echocardiogram showed a dilated LV and an ejection fraction of 20%.
3. Surgical Procedure
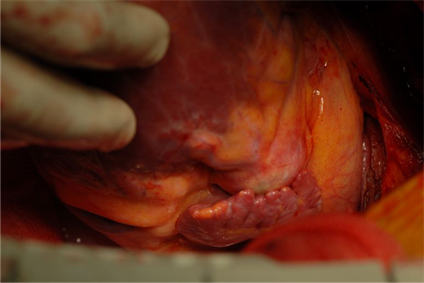
Along a midline sternotomy incision, the chest was opened. The coronary aneurysm was seen adjacent to the pulmonary artery (Figure 3), which was about 20 × 18 × 18 mm in size. OPCAB was performed using saphenous vein grafts (SVG), as the left internal mammary was atretic. He had a SVG to LAD, Diagonal and obtuse marginal coronary artery. The top ends of the vein grafts were anastamosed to the aorta using a side clamp. No IABP (intra-aortic balloon pump) was used. As the CAG showed an ante grade flow into the aneurysmal sac, we decided to ligate the left main to prevent further aneurysmal dilatation (Figure 4) the patient was stable all through surgery. His post operative course was unevenful. One year later his review showed an LV improvement to an ejection fraction of 35% - 40%. He was active and working. We recently reviewed him after two yearsand his LV had improved significantly and had an EF of 50%.
4. Discussion
Kawasaki disease, or mucocutaneous lymph node syndrome, occurs predominantly in children and rarely in adults [1] . Signs include acute vasculitis, mucosal inflammation, rash, cervical adenopathy, hand and foot swelling [2] and in the most severe cases, aneurysms develop in one or more coronary arteries [3] .
Congenital coronary artery aneurysms are rare. The most common etiology is atherosclerosis, present in 50% - 80% of cases [3] [4] [5] . Histologic examinations of coronary aneurysms have revealed findings of arteriosclerosis, such as hyalinization and lipid deposition of the intima, intramural hemorrhage, and inflammatory reactions consistent with the arteriosclerotic process. Patients with Kawasaki disease-related aneurysms generally remain asymptomatic. They display normal findings on electrocardiograms and stress tests and are at low risk of subsequent myocardial infarction or sudden death. Sometimes, aneurysms persist and become occlusive, thereby increasing the risk of myocardial infarction or sudden death. Myocardial infarction can occur early or late after the acute phase; therefore, patients should be counselled to avoid atherosclerotic risk
Figure 1. Coronary angiogram showing the anuerysmal sac in the bifurcation of left main coronary artery.
Figure 2. Showing multiple aneurysms on the RCA, though not compromising the coronary flow.
factors, and the progress of these patients should be followed into adulthood [4] . The most important predictor of myocardial infarction and other chronic sequel is aneurysmal size [5] . Giant coronary artery aneurysms have a poor prognosis. They do not regress and usually result in ischemic heart disease. Affected arterial segments eventually calcify, thrombose, or become stenotic.
Phtoto 3. Surgical figure of the aneurysmal sac at the left main bifurcation.
Figure 4. Showing the dissection of left main and ligation of the same.
Coronary revascularization is recommended for patients with giant or multiple coronary artery aneurysms or significant stenosis [6] . Overall mortality is low for such operations, and graft target sites are easily accessible, since most coronary artery lesions occur in proximal segments with little distal involvement [7] . The unusual presentation of this case in adult hood and with severe LV dysfunction has made this an interesting case to be presented.
Kawasaki disease in adult is definitely a rare entity, and its cause has been always a mystery. One of the currently most accepted theories [8] suggests that the disease may be caused by an infectious agent, probably a virus, which is inhaled and infects medium-sized ciliated bronchial epithelial cells. This non-identified agent is then engulfed by tissue macrophages, and an innate immune response is initiated with subsequent infiltration of macrophages, antigen-specific T lymphocytes and IgA plasma cells. Monocytes and macrophages containing the KD agent enter the bloodstream so that the agent is able to infect specific susceptible tissues (vascular and ductal tissues). In the coronary tissue, the infection leads to the secretion of vascular endothelial growth factor, matrix metalloproteinase 9, tumour necrosis factor-α and other pro-inflammatory cytokines. This immune reaction destroys the intima, internal and external elastic laminae of the coronary artery which are fragmented, and ballooning occurs leading to an artery aneurysm [9] .
5. Conclusion
Adult Kawasaki disease has been a rare entity. And its presentation usually follows a definite symptom in these patients’ young age. These patients are usually symptomatic during their infancy or in adolescence. The absence of symptoms in this patients childhood and his presentation with just heart failure and acute myocardial infarction in his thirties, in fact prompted us to present this rare case.
Acknowledgements
We acknowledge the help of Ms. Nimmi Nanoo, Mr. Arun, Mr. Bipin and Mr. Jayaprakash in compiling and assisting in the data entry over the years.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Cite this paper
Vettath, M.P., Ravisankar, M., Veluchamy, K.A. and Gangadharan, N. (2018) OPCAB (Off Pump Coronary Artery Bypass) for Kawasaki Disease. Surgical Science, 9, 287-292. https://doi.org/10.4236/ss.2018.99034
References
- 1. Naoe, S., Takahashi, K., Masuda, H. and Tanaka, N. (1991) Kawasaki Disease. With Particular Emphasis on Arterial Lesions. Acta Pathologica Japonica, 41, 785-797.
- 2. Gersony, W.M. (1991) Diagnosis and Management of Kawasaki Disease. JAMA, 265, 2699-2703. https://doi.org/10.1001/jama.1991.03460200079040
- 3. Bradway, M.W. and Drezner, A.D. (1997) Popliteal Aneurysm Presenting as Acute Thrombosis and Ischemia in a Middle-Aged Man with a History of Kawasaki Disease. Journal of Vascular Surgery, 26, 884-887. https://doi.org/10.1016/S0741-5214(97)70104-6
- 4. Iemura, M., Ishii, M., Sugimura, T., Akagi, T. and Kato, H. (2000) Long Term Consequences of Regressed Coronary Aneurysms after Kawasaki Disease: Vascular Wall Morphology and Function. Heart, 83, 307-311. https://doi.org/10.1136/heart.83.3.307
- 5. Suzuki, A. and Kamiya, T. (1991) Visualization of Coronary Artery Lesions in Kawasaki Disease by Angiography. Cardiology in the Young, 1, 225-233. https://doi.org/10.1017/S1047951100000421
- 6. Rozo, J.C., Jefferies, J.L., Eidem, B.W. and Cook, P.J. (2004) Kawasaki Disease in the Adult: A Case Report and Review of the Literature. Texas Heart Institute Journal, 31, 160-164.
- 7. Kitamura, S., Kameda, Y., Seki, T., Kawachi, K., Endo, M., Takeuchi, Y., et al. (1994) Long-Term Outcome of Myocardial Revascularization in Patients with Kawasaki Coronary Artery Disease. The Journal of Thoracic and Cardiovascular Surgery, 107, 663-674.
- 8. Rowley, A.H., Baker, S.C., Orenstein, J.M. and Shulman, S.T. (2008) Searching for the Cause of Kawasaki Disease—Cytoplasmic Inclusion Bodies Provide New Insight. Nature Reviews Microbiology, 6, 394-401. https://doi.org/10.1038/nrmicro1853
- 9. Sánchez-Manubens, J., Bou, R. and Anton, J. (2014) Diagnosis and Classification of Kawasaki Disease. Journal of Autoimmunity, 48-49, 13-117. https://doi.org/10.1016/j.jaut.2014.01.010