Surgical Science
Vol.06 No.10(2015), Article ID:60448,4 pages
10.4236/ss.2015.610062
Right Internal Jugular Vein Ectasia in African Woman: A Report of 2 Cases
Seydou Togo1, Moussa Abdoulaye Ouattara1, Sékou Koumaré2, Mody Abdoulaye Camara3, Sadio Yena1
1Thoracic and Vascular Surgery Department, Hospital of Mali, Bamako, Mali
2Surgery “A” Department, Point G Hospital, Bamako, Mali
3Radiology Department, Hospital of Mali, Bamako, Mali
Email: drseydoutg@yahoo.fr
Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 14 September 2015; accepted 18 October 2015; published 21 October 2015
ABSTRACT
Internal jugular vein (IJV) ectasia is a rare benign disease. It commonly presents as a unilateral, soft, compressible neck swelling that mostly involves the right side. It is usually a childhood disease and believed to be of congenital origin. Accurate diagnosis from careful history, physical examination and radiological study can be made. We report here two cases of IJV ectasia in African adults with right lateral neck mass dilating when increase intrathoracic pressure. Because of its rarity, this entity is frequently ignored or misdiagnosed. This case report intends to stress the importance of keeping IJV ectasia as differential diagnosis in mind in case of lateral neck swellings to avoid invasive investigations and inappropriate treatment. The asymptomatic case management of IJV ectasia is conservative with long-term surveillance.
Keywords:
Jugular Vein, Ectasia, Adults, Management

1. Introduction
Internal jugular vein (IJV) ectasia is a rare benign disease, which mostly involves the right side. IJV commonly appears as a unilateral, a soft, compressible mass in the neck which typically increases in size on straining attributable to increased intrathoracic pressure with breath-holding or may be triggered by the Valsalva maneuver [1] [2] . It can occur at any age and affect both genders but it is usually described as a childhood disease [2] , although the exact etiology is still controversial [1] . Due to the rarity of this condition, a high index of suspicion is required and the possibility of IJV should always be borne in mind. Complications are rare, such as thrombosis and Horner’s syndrome [3] [4] and the main complaint is essentially cosmetic. However, recent long-term observational studies have documented numerous asymptomatic patients with favorable courses. The disease is frequently misdiagnosed and managed inappropriately. To our knowledge, a single case has been reported in an African adult. [3] Our cases are being reported in view of its clinical rarity and to highlight the management strategies with the literature review.
2. Cases Report
2.1. Case 1 Presentation
A 77-year-old woman presented to us with complaints of a painless swelling appearing in the neck on coughing or sneezing and disappearing at rest since last 1 year. It was gradual in onset and slowly progressive in nature. It was associated with hoarseness of voice for the same duration. She had a history of hypertension, for which she was taking antihypertensive agents. However, there was no history of pain, fever, facial puffiness, difficulty in breathing, or swallowing. She had no history also of trauma to the neck region or any previous neck infection. On physical examination, she looked healthy. On initial examination of the neck, no identifiable mass was seen; no masses were detected on palpation of the neck and no neck swelling was observed. A 1 × 2 cm mass appeared on her right side of the neck on straining (coughing). The mass emerged from the upper right anterior triangle of the neck (Figure 1). The swelling was soft, cystic, and non-tender; skin over cervical lymph nodes was normal. No bruit or pulsation over the swelling was present. The mass was not transilluminant. Oropharyngeal examination revealed no abnormality. Other systemic examinations were unremarkable. Color Doppler ultrasound showed distension of the lumens but there was no thrombus formation measuring 4 cm in its transverse diameter. A contrast enhanced computed tomography (CECT) confirmed the diagnosis of IJV ectasia and revealed significant fusiform distension of the right internal jugular vein with a maximum diameter of 35 mm at rest (Figure 2). The patient was reassured and no surgical treatment was advised. Voice therapy was conducted, leading to symptomatic improvement. The patient was free of any symptoms after 6 months follow up.
2.2. Case 2 Presentation
A 57-year-old woman presented with complaints of painless, intermittent right neck swelling noticed initially about 2 years prior to presentation. The swelling was insidious in onset, gradually progressive with prominence of the swelling seen on coughing, learning forward or straining. There was no history of change in voice, no difficulty in swallowing or breathing. She was diagnosed hypertensive about 4 years earlier but non-compliant with antihypertensives. She had no other significant past history of illness. Physical examination revealed a soft,
Figure 1. Normal appearance of neck at rest (a). Unilateral right-sided internal jugular ectasia on straining (coughing) (b).
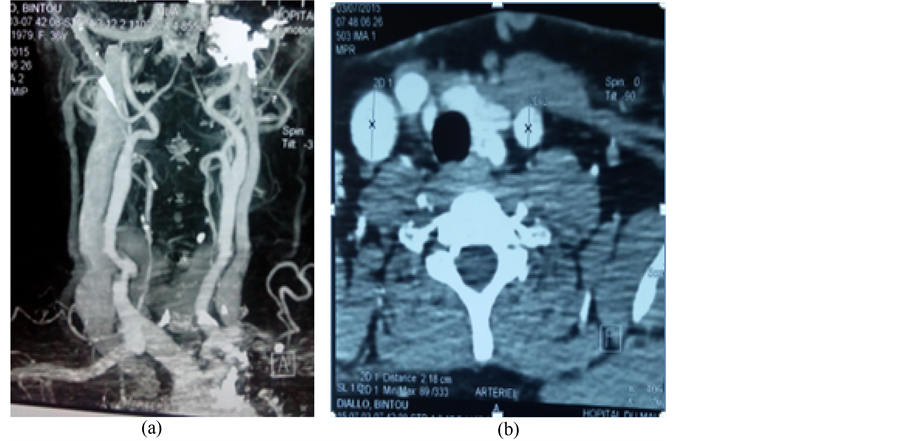
pulsatile, fusiform right lower neck swelling anteromedial to the sternocleidomastoid muscle (Figure 3) and was non-tender but compressible. Ultrasound of the mass showed a fusiform dilatation of the right internal jugular vein measuring 3 cm in its widest transverse diameter at the level of the thyroid gland. It showed normal venous spectral wave form on Doppler investigation and was completely compressible. No thrombus was seen but turbulent flow was noted. The left IJV was normal in size measuring 1.1 cm in diameter at the corresponding level. Contrast-enhanced computed tomography (CECT) of the neck showed the extent of the dilatation to be progressively increasing from the jugular foramen to the clavicular region caudally with a maximum diameter of 30 mm at rest (Figure 4). However, there was no mediastinal mass demonstrated in the CECT. There were no symptoms found during the follow-up. The patient was reassured and she is presently scheduled for yearly follow-up clinic visits.
Figure 2. Contrast-enhanced computed tomography revealed significant fusiform distension of the right internal jugular vein (IJV) (a). IJV with a maximum diameter of 35 mm (b).
Figure 3. Unilateral right-sided internal jugular vein ectasia in a woman at rest (a). Unilateral right-sided IJV ectasia on profile (b).
Figure 4. Contrast-enhanced computed tomography of the neck showed dilated right internal jugular vein (IJV) at rest (a). IJV with the diameter measuring 30 mm (b).
3. Discussion
IJV ectasia in the neck is a rare entity, especially in adult [4] . It is a benign vascular abnormality but may be under-reported possibly due to its benign nature [5] . Anatomically, Jugular vein ectasia have been described in the following sequence in frequency: internal jugular, external jugular, anterior jugular and superficial communicans [6] . In our cases the IJV was affected which is more common [2] [6] . There is no known sex predilection. It is reported that males are more commonly affected than females [3] [6] . Our cases were females. Although cases of internal and external jugular vein ectasia have been reported mostly in children and non-African adults, as far as we are aware very few cases has been previously reported in the electronic literature in an African adult especially in woman [3] . The cause of venous ectasia is unknown. It may be congenital, although this has not been proved. Because jugular vein ectasia frequently develops in childhood, congenital thinning of the carotid sheaths and the presence of anatomic venous perfusion impairment have been suggested [2] [5] . Although rare, there are reports of this disease in adults [1] [7] . Acquired factors such as inflammation, injury, and the state of Valsalva strain are considered to contribute to its development in adults [2] . It is also known that IJV ectasia develops more frequently in the right jugular vein because this vessel is more subject to the effects of increased intrathoracic pressure than the left jugular vein [1] [3] . The left being placed more medially was not subject to this stress. Our patients presented with right sided swelling. Clinically, the mass appears as a soft, cystic, and fusiform mass on straining and sometime completely disappears at rest. In our patients one case was associated with hoarseness of voice. There are very few case reports reporting this complication [1] . The differential diagnosis for similar neck swelling includes a laryngocele, branchial cyst, cystic hygroma, cavernous hemangioma and superior mediastinal cyst [8] . Laryngocele is most common among these. The thyroglossal duct cyst, dermoid cyst, bronchogenic cyst, cervical adenitis and metastatic adenopathy also need exclusion. In our cases, absence of mediastinal widening or air in the mass excludes mediastinal tumor and laryngocele. In many cases with jugular vein ectasia, imaging tests such as computed tomography, MRI, and ultrasound show characteristic findings leading to a definitive diagnosis. The swelling is not known to progress rapidly and there have been no instances of spontaneous rupture of the swelling [9] . Complications reported in general are thrombosis and Horner’s syndrome [10] [11] . In this cases authors suggested surgical removal of the involved segment without delay, because of some other potential complications [8] . Our case had no such complications. Unless complications occur or the lesions are cosmetically deforming, most authors recommend conservative management [9] [11] . Surgery is indicated for cosmetic reasons and in symptomatic patients only [6] . This type of operation is associated with a high surgical risk: vessel or nerve injury (vagus nerve injury, phrenic nerve injury or brachial plexus injury), air embolism or venous thrombosis [1] . In the past, jugular vein ectasia was generally resected surgically for fear of possible increases in size and exacerbation of the condition. However, recent long-term observational studies have documented numerous asymptomatic patients with favorable courses, and conservative therapy has now become a mainstream treatment [1] [2] [7] . Surgery is considered only when there is evident thrombus formation, a tendency for an increase in the size of the distension with symptoms, or a cosmetic problem [1] [5] [10] . As our patients were asymptomatic, we counseled the patients and reassured them of good prognosis and no further steps were taken. Only voice therapy was advised for symptomatic management leading to improvement in the elderly woman. The spontaneous rupture of IJV has never been reported and the benign condition of jugular vein ectasia must be kept in mind to avoid unnecessary risky surgical procedures.
4. Conclusion
Internal jugular vein ectasia in adult is a rare disease and relatively uncommon in female. This rare benign vascular abnormality may be under-reported and frequently misdiagnosed possibly due to its benign nature. Treatment is mainly conservative in cases where there are no symptoms, complications or cosmetic concerns.
Cite this paper
SeydouTogo,Moussa AbdoulayeOuattara,SékouKoumaré,Mody AbdoulayeCamara,SadioYena, (2015) Right Internal Jugular Vein Ectasia in African Woman: A Report of 2 Cases. Surgical Science,06,437-441. doi: 10.4236/ss.2015.610062
References
- 1. Lubianca-Neto, J.F., Mauri, M. and Prati, C. (1999) Internal Jugular Phlebectasia in Children. American Journal of Otolaryngology, 20, 415-418.
http://dx.doi.org/10.1016/S0196-0709(99)90085-6 - 2. Price, D.J., Ravindranath, T. and Kaler, S.G. (2007) Internal Jugular Phlebectasia in Menkes Disease. International Journal of Pediatric Otorhinolaryngology, 71, 1145-1148.
http://dx.doi.org/10.1016/j.ijporl.2007.02.021 - 3. Ogbole, G.I., Irabor, A.E., Oladapo, A.P. and Bolutife, P.Y. (2010) Internal Jugular Phlebectasia in an African Adult. BMJ Case Reports, 10, 1136.
http://dx.doi.org/10.1136/bcr.02.2010.2724 - 4. Tanigawa, T., Shibata, R., Shiga, A. and Murohara, T. (2014) Left Jugular Phlebectasia in an Elderly Patient. Circulation, 130, 1416.
http://dx.doi.org/10.1161/CIRCULATIONAHA.114.012357 - 5. Sander, S., Elicevik, M., Unal, M. and Vural, O. (1999) Jugular Phlebectasia in Children: Is It Rare or Ignored? Journal of Pediatric Surgery, 34, 1829-1832.
http://dx.doi.org/10.1016/S0022-3468(99)90323-8 - 6. Abdulla, A.S. and Aldabagh, M.H. (2008) Congenital Phlebectasia of the Internal Jugular Vein (Case Report). Dohuk Med J, 2, 155-160.
- 7. Uzun, C., Taskinalp, O., Koten, M., Adali, M.K., Karasalihoglu, A.R. and Pekindil, G. (1999) Phlebectasia of Left Anterior Jugular Vein. Journal of Laryngology & Otology, 113, 858-860.
http://dx.doi.org/10.1017/S0022215100145426 - 8. Inci, S., Bertan, V., Kansu, T. and Cila, A. (1995) Horner’s Syndrome Due to Jugular Venous Ectasia. Child’s Nervous System, 11, 533-535.
http://dx.doi.org/10.1007/BF00822844 - 9. LaMonte, S.J., Walker, E.A. and Moran, W.B. (1976) Internal Jugular Phlebectasia. A Clinicoroentgenographic Diagnosis. Archives of Otolaryngology, 102, 706-708.
http://dx.doi.org/10.1001/archotol.1976.00780160102015 - 10. Balik, E., Erdener, A., Taneli, C., Mevsim, A., Sayan, A. and Yuce, G. (1993) Jugular Phlebectasia in Children. European Journal of Pediatric Surgery, 3, 46-47.
http://dx.doi.org/10.1055/s-2008-1063507 - 11. Shimizu, M., Takagi, Y., Yoshio, H., Takeda, R. and Matsui, O. (1992) Usefulness of Ultrasonography and Doppler Color Flow Imaging in the Diagnosis of Internal Jugular Phlebectasia. Heart and Vessels, 7, 95-98.
http://dx.doi.org/10.1007/BF01744455