Surgical Science
Vol.4 No.3(2013), Article ID:28589,3 pages DOI:10.4236/ss.2013.43035
Two Cases of Distal Anterolateral Thigh Flap
1Department of Plastic and Reconstructive Surgery, Shinyurigaoka General Hospital, Kawasaki, Japan
2Department of Tsukiji Dermatology Plastic and Hand Surgery, Department of Plastic and Reconstructive Surgery, Tokyo, Japan
3Tokyo Teishin Hospital, Tokyo, Japan
4Department of Oumu Municipal Hospital, Asahikawa, Japan
5Department of I-I and Tower Clinic, Tokyo, Japan
Email: aamnnty0418@gmail.com
Received January 11, 2013; revised February 19, 2013; accepted February 28, 2013
Keywords: Anterolateral Thigh Flap; Distal Thigh Flap; Thin Flap
ABSTRACT
We report our experience with two cases of anterolateral thigh flaps based on the musculocutaneous perforators arising from a more distal part of the descending branch than in the conventional anterolateral thigh flap. Case 1: A 53-year-old man with a skin ulcer over the anterior surface of the left tibia secondary to plate fixation for an open fracture. The perforator marked with preoperative Doppler was located 8 cm proximal to the superior border of the patella. Without thinning, the flap was 10 × 4 cm in size and 5 mm thick. Case 2: A 46-year-old man with necrosis of the right index finger after replantation. The flap was 5 × 3 cm in size and 3 mm in thickness. This “distal” anterolateral thigh flap can be raised as a quite thin flap with a long pedicle and, therefore, is considered useful in the reconstruction of various soft tissue defects.
1. Introduction
The anterolateral thigh (ALT) flap is supplied by the perforating vessels arising from the descending branch of the lateral femoral circumflex artery. The perforators come into the subcutaneous tissue under the middle third of the line connecting the anterior superior iliac spine and the lateral border of the patella [1]. In this article, we report our experience with two cases of anterolateral thigh flaps based on the musculocutaneous perforators arising from a more distal part of the descending branch than in the conventional anterolateral thigh flap. This “distal” anterolateral thigh flap can be raised as a quite thin flap with a long pedicle and, therefore, is considered useful in the reconstruction of various soft tissue defects.
2. Operative Procedure
Preoperatively the perforators are located with a Doppler probe and marked on the skin. In our distal ALT flap, the perforators lie in the distal third of the line connecting the anterior superior iliac spine and the lateral border of the patella, which would be the middle third of the axis in the conventional ALT flap. The flap is designed to incorporate the perforators and a medial incision is taken first to explore the perforators. When any is found, an incision is made in the fascia to trace the perforator deep into the vastus lateralis muscle. Care is taken to avoid cutting the numerous minute vessels emerging to the muscle belly; and bipolar electrocoagulation or ligation should be applied where necessary. When the descending branch is identified, the dissection continues proximally until the required pedicle length is obtained. After the pedicle is isolated, the flap is dissected circumferentially and checked for the blood supply. The pedicle is divided when the recipient site is prepared.
3. Case Reports
3.1. Case 1
A 53-year-old man with a skin ulcer over the anterior surface of the left tibia secondary to plate fixation for an open fracture (Figure 1(a)). The perforator marked with preoperative Doppler was located 8 cm proximal to the superior border of the patella across the line connecting the anterior superior iliac spine and the lateral border of the patella. The perforator rose from the descending branch of the lateral femoral circumflex artery. Without thinning, the flap was 10 × 4 cm in size and 5 mm thick at the base of the pedicle entering the flap and 3 mm thick at the margin (Figure 1(b)). The flap was grafted successfully. No additional operations, such as flap defatting, were performed (Figure 1(c)).
 (a)
(a)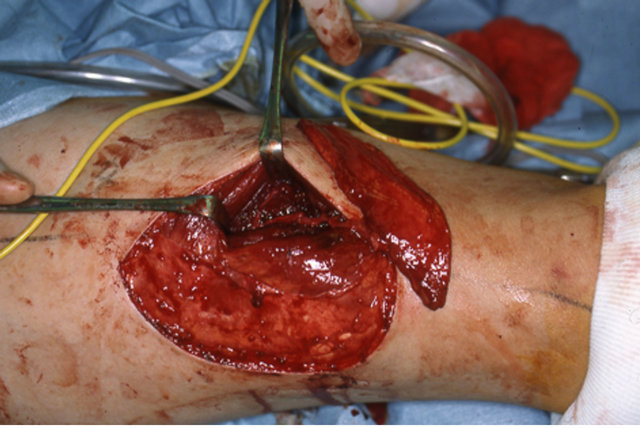 (b)
(b)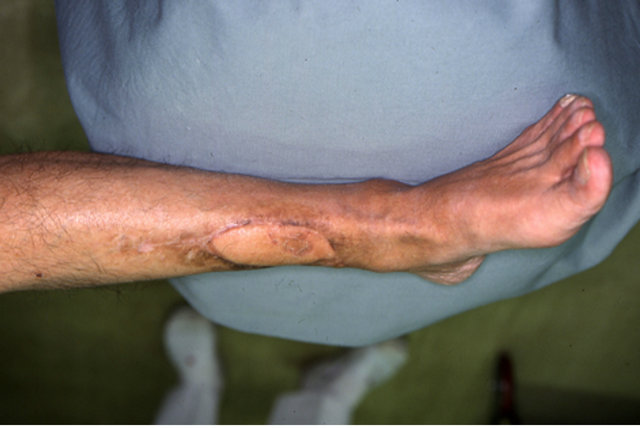 (c)
(c)
Figure 1. (a) Case 1: A 53-year-old man with a skin ulcer of the left leg after open fracture. (b) The perforator was located 8 cm proximal to the superior border of the patella. The flap was 10 × 4 cm in size and 5 mm thickness with a pedicle length of 12 cm. (c) 6 months postoperatively.
3.2. Case 2
A 46-year-old man with necrosis of the right index finger after replantation. The defect involved the cutaneous soft tissue distal to the middle of the middle phalanx and the bone distal to the distal interphalangeal (DIP) joint (Figure 2(a)). The perforator was located 8 cm proximal to
 (a)
(a) (b)
(b) (c)
(c)
Figure 2. (a) Case 2: A 46-year-old man with a skin defect of the right index finger after replantation. (b) The flap was 5 × 3 cm in size and 3 mm in thickness with a pedicle length of 12 cm. (c) 5 months postoperatively.
the superior border of the patella along the line connecting the anterior superior iliac spine and the lateral border of the patella. The flap was 5 × 3 cm in size and 3 mm in thickness with a pedicle length of 12 cm (Figure 2(b)). The pedicle was anastomosed with the radial artery and vein in the anatomical snuffbox. The patient was allowed to walk on the 4th postoperative day and no complaints have been reported about walking or pain in the flap donor site. In the 5 months since the operation, the range of motion of the hand and fingers has been good (Figure 2(c)).
4. Discussion
The descending branch of the lateral femoral circumflex artery provides musculocutaneous and/or septocutaneous perforating branches in the middle third of the thigh and supplies the anterolateral aspect of the femoral skin. These cutaneous branches serve as the nutrient vessels of the ALT flap. The descending branch passes through the middle third of the thigh, continues downward in the areolar tissue between the rectus femoris and vastus intermedius muscles, and eventually merges into the articular vascular network of the knee or terminates in the rectus femoris muscle. It also has been reported that the descending branch provides several musculocutaneous perforating branches to the rectus femoris or vastus lateralis muscle in the distal region of the thigh, but that those perforators are often extremely thin or hardly distinguishable [1,2].
The flaps we experienced are considered to have been elevated on a single musculocutaneous perforator of the distal region of the thigh without sacrificing muscle tissue. The muscle pierced by the pedicle was the vastus lateralis muscle in either case.
A distinctive feature of the “distal” ALT flap is that it is generally thinner than the conventional ALT flap. This is because the femoral subcutaneous tissue tends to become thinner as it descends in the anterolateral aspect of the thigh. For example, a flap taken from the proximal third of the anterolateral thigh is usually more than 1 cm thick and, where necessary, should be thinned before being planted on to the recipient site. In cases of immediate reconstruction, the thinning procedure involves a special technique—such as microdissection [3]—to remove unnecessary subcutaneous tissue around the pedicle entering the flap. In comparison, the distal ALT flaps we experienced were originally thin—ranging from 3 to 5 mm without thinning—and, therefore, considered useful in the reconstruction of the extremities, especially the regions proximal to the elbow and knee. Another feature of the distal ALT flap is that it can be raised with a long pedicle. It is longer than that of the conventional ALT flap because it arises from a more distal part of the descending branch.
It is not always true that useful perforators can be found in the distal region of the thigh. However, when a thin flap of good pedicle length is required, the distal ALT flap should be the first option to consider and the distal third of the thigh explored with a Doppler probe.
REFERENCES
- D. C. Xu, S. Z. Zhong, J. M. Kong, et al., “Applied Anatomy of the Anterolateral Femoral Flap,” Plastic & Reconstructive Surgery, Vol. 82, No. 2, 1988, pp. 305-310. doi:10.1097/00006534-198808000-00016
- K.-D. Wolff and A. Grundmann, “The Free Vastus Lateralis Flap: An Anatomic Study with Case Reports,” Plastic & Reconstructive Surgery, Vol. 89, No. 3, 1992, pp. 469- 475. doi:10.1097/00006534-199203000-00012
- N. Kimura, K. Satoh and Y. Hosaka, “Microdissected Thin Perforator Flaps: 46 Cases,” Plastic & Reconstructive Surgery, Vol. 112, No. 7, 2003, pp. 1875-1885. doi:10.1097/01.PRS.0000091248.41007.2D

