Open Journal of Medical Psychology
Vol.2 No.3(2013), Article ID:34001,5 pages DOI:10.4236/ojmp.2013.23013
The Affects of a Single Bout of Exercise on Mood and Self-Esteem in Clinically Diagnosed Mental Health Patients
Centre of Sport, Health and Exercise Research, Faculty of Health Sciences, Staffordshire University, Staffordshire, UK
Email: *j.a.randall@staffs.ac.uk
Copyright © 2013 Naomi J. Ellis et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 15, 2013; revised April 30, 2013; accepted May 9, 2013
Keywords: Clinical; Exercise; Health; Mental health; Mood; Self-esteem
ABSTRACT
Objectives: Research has highlighted the importance of regular exercise within the general population and mental health groups in regard to mood and self-esteem, as well as single bout exercise within the general population. However, research into single bout exercise in mental health population is lacking. This study investigated the impact of a single bout of exercise, on mood and self-esteem, in patients with a wider clinical mental health diagnosis. Design: A quantitative questionnaire was completed immediately pre and post a single, 45 minute bout of moderate intensity exercise, consisting of the Brunel Universal Mood States (BRUMS) questionnaire and the Rosenberg Self Esteem Scale (RSE). Methods: Participants attending a mental health hospital with a clinical mental health diagnosis (N = 54) completed the questionnaire. Information regarding physical activity levels, mental health diagnosis and length of hospital stay were collated. Results: A significant improvement was identified on the RSE as well as the BRUMS (depression, anger, confusion, anxious tension and vigour) over time. Conclusion: The significant findings highlight the importance of exercise promotion within this population group, and the potentially beneficial role that a single bout of exercise can have on mood and self-esteem in patients experiencing mental health problems.
1. Introduction
Mental health is currently at the forefront of government policy and is receiving ever increasing interest from researchers, the general public and policy makers [1]. The most recent figures suggest that in the UK 1 in 4 people report at least one diagnosable mental health condition during their lifetime [2,3] costing the UK an estimated £77 billion in 2002/03 [3,4].
There is a growing recognition surrounding the mental health benefits of regular physical activity in the general population [5]. Research suggests it can reduce stress, [5,6] anxiety [7] and depression [8] whilst improving mood [5,9,10]. A number of reviews have explored psychological outcomes and regular exercise within the general population [9-11]. Findings suggest that regular exercise improves various psychological characteristics (e.g., mood). Whilst regular exercise appears to be preferable, it is not always practical. Research indicates that a single bout of exercise can enhance mood and well-being in the general population [9,12-15]. This highlights potential benefits for groups where attrition is high or attendance to multiple bouts is difficult, such as some clinical mental health populations [16].
Research into regular exercise and psychological benefits within mental health populations is by no means lacking and has further strengthened our understanding of the relationship between mental health and exercise [17-19]. There are a variety of recent reviews and metaanalyses on anxiety [20,21], depression [22,20] and psychosis [23] highlighting the relationship between exercise and psychological benefits within these populations.
Research specifically investigating the effect of a single bout of exercise with individuals experiencing mental health difficulties is limited [24,25]. Significant improvements in psychological outcomes were reported in people with depressive disorders [24-26]. Similar findings were also reported by Weinstein [25], although these reductions in depressive symptoms were not maintained over time (one hour post).
Given that evidence suggests a single bout of exercise can promote a change in mood and self-esteem within the general population [14], and in individuals with depression [24], the potential of such immediate benefits in mental health population groups, in whom the need is often greatest, warrants further investigation. Therefore, the aim of this research is to examine whether a single bout of exercise has an effect on mood and self-esteem in clinically diagnosed patients experiencing a range mental health problems.
2. Method
2.1. Participants
A total of 65 participants, 45 males (69.2%) and 20 females (30.8%), engaged with the research consisting of 40 (61.5%) inpatients, 22 (35.5%) outpatients and 3 (4.6%) who did not specify. Overall 59 (90.8%) described themselves as white British, 2 (3.2%) as black British, 1 (1.5%) as “other” with 3 (4.6%) not disclosing. The mean age was 44.6 (SD = 11.7) years, minimum 19 years and maximum 70 years. Length of inpatient stay varied from 2 days to 2 years 9 months, with a mean stay of 59.22 (SD = 204.01) days. The primary diagnosis, based on staff information, was anxiety (52.3%), with additional diagnoses of depression (32.3%), schizophrenia (6.1%), bipolar (4.6%), alcoholism (3.1%) and other (1.5%). Physical activity levels were reported as being below the recommended amounts of 30 minutes at a moderate intensity on a minimum of 5 days per week. Participants reported, a mean of 2.8 days of activity (SD = 2.2) in the previous week with no difference between inpatients and outpatient responses.
2.2. Effect Size
Of the two studies undertaken within this area effect size varies. Bartholomew [24] reported a medium effect size (n = 40), while Weinstein [25] found a small effect size (n = 14). Research in the general population relating to single bout exercise and mental health has typically also found a medium effect size [14,15]. Therefore using a medium effect size of d = 0.6 and a power of 0.8 [27] 45 participants were required for this research.
2.3. Measures
Participants completed a self report questionnaire comprising of demographic information, a single item measure of physical activity, the Brunel Universal Mood States (BRUMS) questionnaire and the Rosenberg Selfesteem scale.
The physical activity single item measure has been taken from the Outdoor Health Questionnaire used in the national Walking for Health scheme. The measure has been validated [28] and the single item physical activity question has been used independently as a self-reported method of obtaining levels of physical activity [29].
The BRUMS has been regularly used to assess mood [30]. The original POMS [31] has been adapted to create a shorter 24 item version, BRUMS, that has been tested for validity and reliability [32,33]. The BRUMS has 6 mood dimensions; tension, depression, anger, vigour, fatigue and confusion. Answers are on a five point Likert scale, ranging from “not at all” to “extremely”.
The Rosenberg Self Esteem scale [34] assesses global self-esteem and is one of the most widely used tests by psychologists for this purpose. The scale has ten items on a four point Likert-type scale ranging from “strongly agree” to “strongly disagree”, and has been used within this population group [35].
2.4. Procedure
A questionnaire was developed in conjunction with the mental health Hospital ensuring it was appropriate for their patient group. Potential participants were initially approached by a member of staff, and the study explained to them. Participants were then given seven days to consider participation. Written informed consent was obtained, following which questionnaires were issued to patients by staff immediately pre and post exercise. The exercise sessions consisted of 45 minutes of moderate intensity aerobic exercise (intensity was self-reported). Participant anonymity was ensured through the use of ID numbers.
Participants met the inclusion criteria if they were: 1) a patient at the mental health hospital; 2) taking part in an exercise group at the hospital; 3) well enough on the day to complete the questionnaire; 4) over 18 years of age. Participants were informed that the questionnaire would take 10 - 15 minutes to complete pre-exercise and up to 5 minutes post exercise. Participants were able to withdraw from the study at any point. If participants requested support in filling out the questionnaire, this was provided by hospital staff. A private room was available for those completing the questionnaire. Analysis was undertaken on data collected as part of a service evaluation by the hospital. Ethical approval was granted for the analysis by Staffordshire University Faculty of Health Sciences Ethics Board; NHS ethics were informed, but as this was a service evaluation NHS ethics approval were not necessary.
3. Results
Due to incorrectly completed questionnaires 11 participants were removed from the study. As such analysis was undertaken on 54 participants.
Figure 1 highlights pre and post changes in mood and self-esteem. It can be observed that negative mood states all decrease, with the exception of fatigue. Vigour and self-esteem, which are positive moods state increase.
The data set was screened for parametric assumptions and was found to lack normal distribution. As such, non-parametric tests were applied. A Wilcoxon signed rank test for matched pairs was undertaken, using SPSS 17.
A significant difference was identified between pre and post scores for depression (T = 0.5, p = 0.000, N = 54, r = 0.678), anger (T = 14.5, p = 0.000, N = 54, r = 0.530) confusion (T = 113.0, p = 0.008, N = 54, r = 0.364), anxious tension (T = 52.5, p = 0.000, N = 54, r = 0.575) and vigour (T = 342.0, p = 0.012, N = 54, r = 0.344). There was no significant difference identified between fatigue scores. A significant difference was identified between the pre and post self-esteem scores (T = 203.5, p = 0.000, N = 54, r = 0.505).
Further post-hoc analysis was then undertaken to investigate any difference in scores regarding mental health diagnosis. A Kruskal-Wallis one way ANOVA by ranks was carried out for all five diagnoses, for each variable (i.e., depression and post depression) and found no significant difference between scores regarding mental health diagnosis. A significant difference was also not noted if those diagnoses with less than five participants were removed (i.e. analysis only on anxiety n = 28; and depression n = 17). Suggesting mental health diagnosis does not affect the pre-post relationship.
4. Discussion
This study was designed to assess the effect of a single, hospital based exercise session on mood and self-esteem in individuals with a clinical mental health diagnosis. The results suggest a significant improvement in six mood states; depression, anxious tension, anger, confusion and vigour and self-esteem.
The results replicate those of healthy populations suggesting that a single bout of exercise significantly influence mood states [12-15]. The findings also support the two previous studies in participants with a clinical diagnosis of depression [24,25].
The only mood state that did not show a significant difference was that of fatigue. However, this could be due to a misinterpretation regarding definition, with participants confusing mental fatigue with physical fatigue, thus this result should be taken with caution [24].
Previous research into the effect of a single bout of exercise on psychological outcomes, for individuals with a mental health diagnosis, has focused on depression
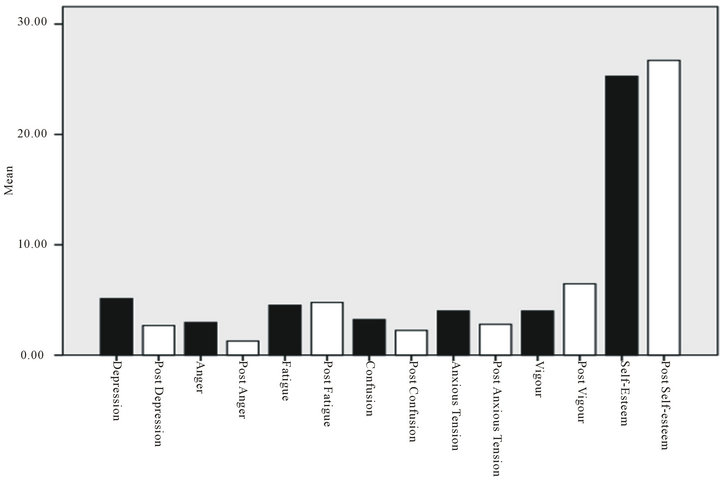
Figure 1. Graphical representation of mean mood and self-esteem results.
[24,25]. The present study aimed to collect data from participants with a range of mental health diagnosis. A significant difference was recorded over time when participants were treated as a single cohort. Further analysis into mental health diagnosis noted no significant difference between diagnoses and psychological characteristics over time. Though due to low sample sizes (when separated by diagnosis) this is not surprising and warrants further investigation.
In comparison to previous research, the sample size used in this pilot study was larger [24,25], but this research used participants with a range of diagnosis. As such, if further research was to be undertaken it would be beneficial to collect a larger sample size to fully investigate the effect of a single bout of exercise on a range of clinical diagnosis.
5. Limitations
The measure of intensity was self reported, leading to a potential for miss representation. Sample size was relatively small when participants were separated by diagnosis, which caused issues with intergroup comparisons. Caution needs to be undertaken when generalising these findings as individuals with duel diagnosis were excluded and other co-morbidities were unreported.
6. Conclusion
Overall, despite some limitations, this remains the first investigation into the effect of a single bout of exercise on aggregated individuals with a clinical mental health diagnosis. The positive results from this study are encouraging and provide support for further research in the area. If such results can be recreated with larger samples and for a wider range of mental health diagnoses then the possible implications for these findings are vast.
REFERENCES
- Department of Health, “No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages,” HMSO, London, 2011.
- Department of Health, “Making It Happen: A Guide to Delivering Mental Health Promotion,” HMSO, London, 2001.
- The Office of national Statistics, Cenus, 2001. www.ons.gov.uk
- Sainsbury Centre for Mental Health, “Policy Paper 3: The Economic and Social Costs of Mental Illness,” The Sainsbury Centre for Mental Health, London, 2001.
- S. J. H. Biddle and N. Mutrie, “Psychology of Physical Activity: Determinants, Well-Being and Interventions,” Routledge, Abingdon, 2008.
- K. H. Cooper, J. S. Gallman and J. L. J. McDonald, “Role of Aerobic Exercise in Reduction of Stress,” Dental Clinics of North America, Vol. 30, No. 4, 1986, pp. 133-142.
- P. J. O’Connor, J. S. Raglin and E. W. Martinsen, “Physical Activity, Anxiety and Anxiety Disorders,” International Journal of Sport Psychology, Vol. 31, No. 2, 2000, pp. 136-155.
- L. L. Craft, “Exercise and Clinical Depression: Examining Two Psychological Mechanisms,” Psychology of Sport and Exercise, Vol. 6, No. 2, 2005, pp. 151-171. doi:10.1016/j.psychsport.2003.11.003
- P. C. Dinas, Y. Koutedakis and A. D. Flouris, “Effects of Exercise and Physical Activity on Depression,” Irish Journal of Medical Science, Vol. 180, No. 2, 2011, pp. 319-325. doi:10.1007/s11845-010-0633-9
- K. R. Fox, “The Influence of Physical Activity on Mental Well-Being,” Public Health Nutrition, Vol. 2, Suppl. 3, 1999, pp. 411-418. doi:10.1017/S1368980099000567
- D. Scully, J. Kremer, M. Meade, R. Grahma and K. Dudgeon, “Physical Exercise and Psychological Well Being: A Critical Review,” British Journal of Sports Medicine, Vol. 32, No. 2, 1998, pp. 111-120. doi:10.1136/bjsm.32.2.111
- P. Ekkekakis, E. E. Hall, L. M. Van Landuyt and S. J. Petruzello, “Walking in (Affective) Circles: Can Short Walks Enhance Affect?” Journal of Behavioural Medicine, Vol. 23, No. 3, 2000, pp. 245-275. doi:10.1023/A:1005558025163
- T. C. North, P. McCullagh and Z. V. Tran, “Effect of Exercise on Depression,” Exercise and Sport Science Review, Vol. 18, 1990, pp. 379-412. doi:10.1249/00003677-199001000-00016
- A. Szabo, “Acute Psychological Benefits of Exercise Performed at Self-Selected Workloads: Implications for Theory and Practice,” Journal of Sports Science and Medicine, Vol. 2, 2003, pp. 77-87.
- R. R. Yeung, “The Acute Effects of Exercise on Mood State,” Journal of Psychosomatic Research, Vol. 40, No. 2, 1996, pp. 123-141. doi:10.1016/0022-3999(95)00554-4
- P. M. Dubbert, J. D. White, K. B. Grothe, J. O. Jile and K. A. Kirchner, “Physical Activity in Patients Who Are Severely Mentally Ill: Feasibility of Assessment for Clinical and Research Applications,” Archives of Psychiatric Nursing, Vol. 20, No. 5, 2006, pp. 205-209. doi:10.1016/j.apnu.2006.04.002
- K.A. Barbour, T. M. Edenfield and J. A. Blumrnthal, “Exercise as a Treatment for Depression and Other Psychiatric Disorders: A Review,” Journal of Cardiopulmonary Rehabilitation & Prevention, Vol. 27, 2007, pp. 359-367.
- D. Carless and K. Douglas, “The Role of Sport and Exercise in Recovery from Serious Mental Illness: Two Case Studies,” International Journal of Men’s Health, Vol. 7, No. 2, 2008, pp. 137-156. doi:10.3149/jmh.0702.137
- D. S. Hutchinson, “Structured Exercise for Persons with Serious Psychiatric Disabilities,” Psychiatric Services, Vol. 56, No. 3, 2005, pp. 353-354. doi:10.1176/appi.ps.56.3.353
- F. J. Penedo and J. R. Dahn, “Exercise and Well-Being: A Review of Mental and Physical Health Benefits Associated with Physical Activity,” Current Opinion in Psychiatry, Vol. 18, No. 2, 2005, pp. 189-193. doi:10.1097/00001504-200503000-00013
- B. M. Wipfli, C. D. Rethorst and D. M. Landers, “The Anxiolytic Effects of Exercise: A Meta-Analysis of Randomized Trials and Dose-Response Analysis,” Journal of Sport & Exercise Psychology, Vol. 30, No. 4, 2008, pp. 392-410.
- C. D. Rethorst, B. M. Wipfli and D. M. Landers, “The Anti-Depressive Effects of Exercise: A Meta-Analysis of Randomized Trials,” Sports Medicine, Vol. 39, No. 6, 2009, pp. 491-511. doi:10.2165/00007256-200939060-00004
- N., Ellis, D. Crone, R. Davey and S. Grogan, “Exercise Interventions as an Adjunct Therapy for Psychosis: A Critical Review,” British Journal of Clinical Psychology, Vol. 46, No. 1, 2007, pp. 95-111. doi:10.1348/014466506X122995
- J. B. Bartholomew, D. Morrison and J. T. Ciccolo, “Effects of Acute Exercise on Mood and Well-Being in Patients with Major Depressive Disorder,” Medicine and Science in Sports and Exercise, Vol. 37, No. 12, 2005, pp. 2032-2037. doi:10.1249/01.mss.0000178101.78322.dd
- A. A. Weinstein, P. A. Deuster, P. L. Francis, C. Beadling and W. J. Kop, “The Role of Depression in Short-Term Mood and Fatigue Responses to Acute Exercise,” International Journal of Behavioral Medicine, Vol. 17, No. 1, 2010, pp. 51-57. doi:10.1007/s12529-009-9046-4
- R. R. Yeung and D. R. Hemsley, “Effects of Personality and Acute Exercise on Mood States,” Personality and Individual’s Difference, Vol. 20, No. 5, 1996, pp. 545-550. doi:10.1016/0191-8869(95)00222-7
- D. Clark-Carter, “Quantitative Psychological Research Third Edition,” Psychology Press, New York, 2010.
- K. Milton, F. C. Bull and A. Bauman, “Reliability and Validity Testing of a Single-Item Physical Activity Measure,” British Journal of Sports Medicine, Vol. 6, 2010, pp. 348-352.
- N. Ellis, C. Gidlow and R. Davey, “Exploring Mental Health Benefits of Physical Activity Using a Social Marketing Approach in Community Settings,” Care Service Improvement Partnership Document, 2009.
- T. Andrade, C. Arce, J. Torrado, J. Garrido, C. De Fancisco and I. Arce, “Factor Structure and Invariance of The Poms Mood State Questionnaire in Spanish,” Spanish Journal of Psychology, Vol. 13, No. 1, 2010, pp. 444-452. doi:10.1017/S1138741600003991
- D. M. McNaire, M. Lorr and L. F. Droppleman, “Manual for the Profile of Mood States,” Education and Industrial Testing Service, San Diego, 1971.
- P. C. Terry, A. M. Lane and G. J. Fogarty, “Construct Validity of the Profile of Mood States—Adolescents for the Use with Adults,” Psychology of Sport and Exercise, Vol. 4, No. 2, 2003, pp. 125-139. doi:10.1016/S1469-0292(01)00035-8
- P. C. Terry, A. M. Lane, H. J. Lane and L. Keohane, “Development and Validation of a Mood Measure for Adolescents,” Journal of Sport Sciences, Vol. 17, No. 22, 1999, pp. 861-872. doi:10.1080/026404199365425
- M. Rosenberg, “Society and the Adolescent Self-Image,” Princeton University Press, Princeton, 1965.
- W. C. Torrey, K. T. Mueser, G. H. McHugo and R. E. Drake, “Self-Esteem as an Outcome Measure in Studies of Vocational Rehabilitation for Adults with Severe Mental Illness,” Psychiatric Services, Vol. 51, No. 2, 2000, pp. 229-233. doi:10.1176/appi.ps.51.2.229
NOTES
*Corresponding author.

