Journal of Biosciences and Medicines
Vol.2 No.5(2014), Article ID:47491,11 pages
DOI:10.4236/jbm.2014.25001
A Competing Risk Hazard Model for Complications of Diabetes Mellitus
Parvin Akter Khanam1*, Mohammed Ataharul Islam2, Mohammed Abu Sayeed3, Tanjima Begum1, Mohammed Golam Rabbani4, Subhagata Choudhury1, Hajera Mahtab1
1Department of Epidemiology and Biostatistics, Bangladesh Institute of Research and Rehabilitation in Diabetes, Endocrine and Metabolic Disorders (BIRDEM), Dhaka, Bangladesh
2Department of Applied Statistics, East West University, Dhaka, Bangladesh
3Department of Community Medicine, Ibrahim Medical College, Dhaka, Bangladesh
4Department of Statistics, Biostatistics and Informatics, University of Dhaka, Dhaka, Bangladesh
Email: *parvin_khanam@yahoo.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 26 April 2014; revised 11 June 2014; accepted 25 June 2014
ABSTRACT
Diabetes mellitus is a major public health problem globally. It is the cause of serious and sometimes life-threatening complications leading to death. It is one of the most common non communicable diseases and leading cause of death in most developed countries including Bangladesh. It is associated with the increased risk of microvascular (nephropathy and retinopathy), macrovascular (cardiovascular diseases, stroke) and other mixed (cataract, pulmonary tuberculosis, foot ulcer etc.) complications. The aim of this study was to determine the risk factors related to diabetes complications and to propose competing risk models for analyzing complications of diabetes mellitus. We study 2887 diabetic patients from the BIRDEM registry record books for the period from 1984 to 1997 who have at least two follow-up visits and who are free from complications at the first visit. The data on variables such as 2-hBG, age, sex, family history of diabetes, area of residence, educational level, BMI, SBP, DBP and treatment status are obtained. Also, the time from the diagnosis of type 2 diabetes mellitus (T2DM) to the occurrence of complications was recorded. We use the competing risk hazard model and examined the potential risk factors for determining the development of such complications. This study reveals that increase in blood pressure is a potential risk factor for CHD and nephropathy in T2DM. We also found that male and illiterate patients are more affected by nephropathy. In our study, we also revealed that female and illiterate patients are also more influenced by cataract.
Keywords:Family History of Diabetes, Educational Level, Type 2 Diabetes Mellitus, Coronary Heart Disease, Mean Arterial Blood Pressure

1. Introduction
Diabetes is the most common metabolic disorder and non communicable diseases and it is the fourth or fifth leading cause of death in most developed countries. There is substantial evidence suggesting that diabetes mellitus has become epidemic in many developing and newly industrialized nation. There are 371 million people living with diabetes worldwide [1] , the number of affected people is predicted to reach 438 million by 2030 [2] . Because of the rapid increase in diabetes prevalence, the number of diabetes complications is rising quickly. For long time diabetes is a contributory factor in the development of diabetic late complications such as macrovascular and micro-vascular complications. The macro-vascular complications are related to atherosclerosis and include mainly coronary artery disease (CAD), peripheral vascular disease (CVD) and cerebrovascular disease (CVD or stroke). Nephropathy, neuropathy and retinopathy are related to the micro-vascular complications [3] . There are only a few prospective studies to investigate the risk factors of long term complications of Type 2 diabetes mellitus (T2DM). A centralized referral system of diabetes subjects at BIRDEM enabled us to investigate retrospective cohort of diabetes and its complications from 1984 to 1997.
Cox [4] developed a survival model for analysis censored lifetime data with appropriate time dependent covariates. Farewell [5] extended the theory of the proportional hazards model for competing causes of failure. There are several references where proportional hazards model deals with the modeling of longitudinal data for diabetes related complications. Duckworth et al. [6] , Holman et al. [7] , Ueda et al. [8] , Boguslawa et al. [9] , Hu et al. [10] and Tuner et al. [11] used the theory of cause-specific proportional hazards model under competing risk framework. In these studies, models for transitions have been proposed. Such models have applications to the study of survival in prospective studies and clinical trials where study subjects are followed to determine their status or well-being over a period of time. During each individual’s observation period, the subject may be classified into various states of health and may die from several causes of death.
In 1998, Turner et al. studied the identification of the risk factors for coronary artery disease in type 2 diabetes. They used the Cox proportional hazards model and it was known as the United Kingdom Prospective Diabetes Study (UKPDS). In this study they have considered two states, one transient state and one absorbing state such as coronary artery disease. In this study they found that increasing age, sex male, LDL, HbA1c, SBP, DBP and smoking were the major risk factors for development of coronary artery disease. So this study concluded that the complications would be prevented or delayed if the patients control their LDL, HbA1c and blood pressure. In 2002, Boguslawa et al. also used this model for microvascular and macrovascular complication of Type 2 diabetes. In this study they have considered two states, one transient state and one absorbing state such as nephropathy, proliferative retinopathy, cardiovascular disease and stroke. In this study they found that FBG and MABP were the major risk factors for development of nephropathy and retinopathy in patients with type 2 diabetes. It was also found that the cholesterol was a risk factor for retinopathy. It was also revealed that the mean arterial blood pressure was a significant risk factor for coronary artery disease and stroke. High cholesterol level increases the hazard for coronary artery disease. It was also found that the history of smoking was not a risk factor for such complications. This study was not able to prove the role of increased fasting blood glucose in the development of macrovascular complications but they found that high blood pressure was a risk factor for cardiovascular disease, stroke, nephropathy and retinopathy. In 2003, Ueda et al. used the Cox proportional hazards model for factors affecting progression of renal failure in patients with type 2 diabetes. In this study it was observed that male patients, lower hemoglobin, and lower albumin were significant predictors for progression of nephropathy. It also revealed that insulin therapy was found to be a significant predictor for slow progression of renal failure and higher mean blood pressure was also a risk factor of progression of renal failure. This study did not prove a significant association of HbA1c and fasting plasma glucose. In 2004, Hu studied the sedentary lifestyle, obesity, and impaired glucose regulation and found as the risk factors for type 2 diabetes. This study revealed that increased physical activity was associated with a significantly reduced risk for type 2 diabetes but inversely associated with any joint levels of BMI and glucose level.
In 2008, Holman et al. discussed the ten years follow-up study in type 2 diabetes and it is the United Kingdom Prospective Diabetes study (UKPDS). In this study, two groups such as conventional therapy (dietary restriction) or intensive therapy (either sulfonylurea or insulin, or in overweight patients, metformin) for glucose control, were included and they attended annual UKPDS clinics for 5 years. In this study, they have taken newly diagnosed type 2 diabetes mellitus to find out the association between microvascular complications and myocardial infarction with blood glucose. This study concluded that the levels of blood pressure and plasma creatine and the ratio of albumin to creatine did not differ significantly between the two groups at any time. This study proved that continued benefit after metformin therapy was evident among overweight patients. This study also indicated that intensive glucose control starting at the time of diagnosis was associated with a significantly decreased risk of microvascular disease. However, for cardiovascular risk reduction in patients with type 2 diabetes the importance of lipid-lowering therapy was emphasized.
In 2009, Duckworth et al. used the Cox proportional hazards model for glucose control and vascular complications in Veterans with type 2 diabetes. In this study also, two groups such as the intensive-therapy (for tight glucose control) group started on maximal doses and the standard-therapy (for moderate glucose control) group started on half of the maximal doses of diabetic medications. In this study we found that the most common event was hypoglycemia, with significantly more episodes in the intensive-therapy group than in the standard-therapy group. This study also revealed that the intensive glucose control in patients with type 2 diabetes had no significant effect on major cardiovascular events, death, or microvascular complications. Only change in albumin level for nephropathy, any worsening of albumin excretion was greater in the standard therapy group; progression to macroalbuminuria was also significant.
The objective of this study was to identify the potential risk factors with diabetes related complications at different stage of first diagnosis of diabetes to follow-up periods. In this paper, we used the cause-specific hazards models of competing risk framework for diabetes related complications data at BIRDEM.
2. Model
The main objective of this study was to develop the competing risks model for Type 2 diabetes mellitus (T2DM) related complications data. For the proposed model we consider seven states of one is transient “healthy” state and others are absorbing “complications” state such as CHD (C), retinopathy (R), nephropathy (N), cataract (CAT), TB (PUL) and other diseases such as stroke, PVD, Keto, skin, etc. (Other) and in this study we considered the patients who have without any complications at the beginning of the study.
To construct the proposed model, we assume that the estimation of one cause regards failure and the remaining five causes are censored. Under this assumption we consider the following transitions where S denotes the state:
1) SDM ® SC
2) SDM ® SR
3) SDM ® SN
4) SDM ® SCAT
5) SDM ® SPUL
6) SDM ® SOther
Figure 1 shows the transition to various complications.
Now to define the model in detail, let there be n individuals are in the study when
it starts and time ;
; . and
. and . Then the defined hazard
rates of this model are functions of different cova-
. Then the defined hazard
rates of this model are functions of different cova-
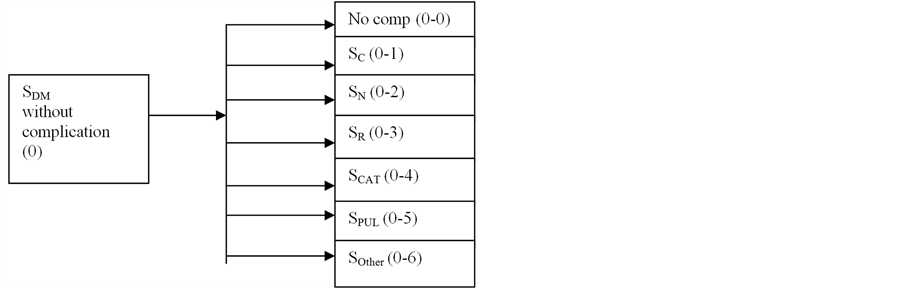
Figure 1. Flow diagram for the proposed competing risk model.
riates. The extended Cox’s proportional hazard model can be expred as,
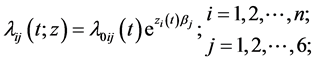
where
 is a vector of p covariate values for the ith subject depending at time t and b
is a vector of coefficients and
is a vector of p covariate values for the ith subject depending at time t and b
is a vector of coefficients and
 is unspecified arbitrary functions and
is unspecified arbitrary functions and . Now the extension of
causespecific hazard function model for different transitions defined as
. Now the extension of
causespecific hazard function model for different transitions defined as
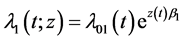
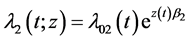
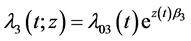
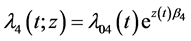
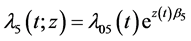
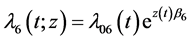 where
where
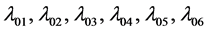 are arbitrary baseline hazard functions
when covariates have no effects upon given transition, and
are arbitrary baseline hazard functions
when covariates have no effects upon given transition, and
 are the unknown regression co-efficient vector corresponding to the covariate set.
are the unknown regression co-efficient vector corresponding to the covariate set.
2.1. Estimation of Parameters
The partial likelihood function [12] for
 is obtained by taking the product of all observed failure time t is
is obtained by taking the product of all observed failure time t is
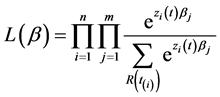
where
 be the risk set at time
be the risk set at time .
.
Then the log-likelihood function becomes
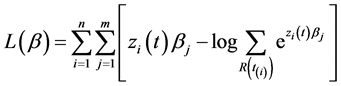
To obtain the maximum likelihood estimator of b can be easily estimated by Newton-Raphson
iterative procedure which requires the score vector and observed Fisher’s information
matrix of b. Then the hth element of score vector
 for cause j is obtained from
for cause j is obtained from
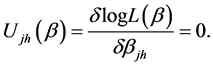
The
 th element of Fisher’s observed information matrix
th element of Fisher’s observed information matrix
 is obtained as
is obtained as
2.2. Test of Hypotheses
For testing the hypotheses , we can use the asymptotic chi-squire
for large samples as follows:
, we can use the asymptotic chi-squire
for large samples as follows:
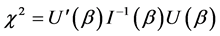
where b is comprised of all vectors of parameters.
3. Data and Variables
In this study the data were collected at BIRDEM hospital from medical record book from January 1984 to December 1997. All the data were registered diabetic patients at BIRDEM in the time of first diagnosis of diabetes and we have taken those patients who were developed no complications at initial stage and followed them upto 1997. Out of 5528 patients, we have taken 2887 patients for our analysis and the other patients were excluded for the different types of errors in information. The average duration of T2DM for these populations is approximately 5.61 years, ranging from 0.01 to 13.0 years. This study is based on the data from prospective study design. A total of 2887 diabetic patients were collected in the follow-up component of the study. In this study we have considered the patients who have no complications at the time of first registration. After diagnosis of diabetes, they might have developed different types of complications during the subsequent follow-up periods. Generally, different types of complications occur for diabetes such as Macro-vascular complications, Microvascular and also mixed type of complications. We also collected information on demographic, socio-economic and anthropometric and clinical variables.
This study makes an attempt to address different types of diabetes related complications during the study period. The complications considered as, coronary heart disease (CHD), nephropathy, retinopathy, cataract, pulmonary tuberculosis (TB) and other diseases (stroke, foot ulcer, PVD, etc.). The explanatory variables are: demographic variables age, sex, family history of diabetes (FHD), etc.; socio-economic variables place of residence, educational level etc. and clinical and anthropometric variables height, weight and calculated body mass index (BMI), blood pressure (systolic and diastolic blood pressure) and calculated mean arterial blood pressure (MABP), 2-h after breakfast blood glucose (2-hBG) and treatment status according to the need of the individual patients. Complications status considered the following categories: “0 = No” means the absence of complication and “1 = Yes” means the presence of the complication and it flows for every complications. The explanatory variables considered the following categories: age (≤40 y = 0, <40 y = 1), sex (female = 0, male = 1), 2-hBG (≤10.0 = 0, >10.0 = 1), MABP (≥93.33 = 0, 93.33 - 100.55 = 1, >100.55 = 2), BMI (≥21.46 = 0, 21.46 - 24.29 = 1, >24.29 = 2), FHD (No = 0, Yes = 1, Unknown = 3), residence (rural = 0, urban = 1, suburban = 2), schooling (yes = 0, no = 1) and treatment (insulin = 0, tablet = 1 diet = 2).
4. Results
To construct the competing risks model for type 2 diabetes mellitus (T2DM) related complications data, we consider one is transient ‘no complication’ state and others are absorbing (complications) state such as different type of complications. We also assume that the estimation of one cause (complication) regards failure and the remaining five causes are censored. Hence, if a transition ends with an event, then it is included in the model.
Table 1 shows the background characteristics of the study population. In our study we have retrieved 2887 diabetic patients. Among them male and female participant were 67.3% and 32.7% respectively. Age is a very common risk factor for diabetes and about 86.3% of the patients were in the age group above 40 years. Most of them (87.2%) were married during registration. Only 12.8% of them were unmarried. About two-thirds of the diabetic subjects (68.9%) were registered from urban and only 22.4% from rural area. During registration only about one-third of the subjects had positive family history of diabetes and about two-thirds could not confirm whether there was any diabetic member in their families. The level of education of the patients registered in 1984 shows that about 11.4% were without any formal education, about 88.6% had primary, secondary or higher. About one-fourth of the subjects had family members equal to or less than four and about 76.4% had family member more than four. In our study we observe that the occupation of the respondents comprise of house-wife 29.3%, labour skilled or unskilled 7.4% and remaining 63.3% were the executive of government or non-government organizations, business proprietors, land-holder-farmers, school teachers, doctors, engineers and other professions. Only 9.4% of diabetics gave the history of regular physical activities. Sedentary habits were reported by 38.3%. The subjects with both physical and mental works constituted the largest group (45.1%). These occupational findings suggest that either the diabetes prevalence was less among those who were exposed to physical activities than those who were not.
Table 2 shows the summary of transition of different types of complications. We found that the patients have developed different types of complications such as coronary heart disease, nephropathy, diabetic retinopathy, cataract, pulmonary tuberculosis and other disease were 5.2%, 5.8%, 6.2%, 5.6%, 2.8% and 10.8% respectively during their follow up period among the participants who started with no complication at the initial stage.
Table 1. Distribution of Type 2 diabetic subjects by background characteristics.
Table 2. Percentage distribution of diabetic patients having complications at different states.
Table 3 displays the estimates of parameters for the hazards models of competing risk framework on diabetes related complications during their follow-up period. We studied the cause defined as complications such as
*p < 0.10, **p < 0.05, ***p < 0.005.
CHD, nephropathy, retinopathy, cataract, pulmonary tuberculosis (TB) and other diseases and nine explanatory/predictor variables such as age, sex, 2-hBG, mean arterial blood pressure (MABP), body mass index (BMI), area of residence, schooling, family history of diabetes (FHD) and treatment. For coronary heart disease (CHD) we observe that the effect of lower 2-hBG have significantly greater risk as compared with high 2-hBG (2-hBG £10 v. >10, HR = 0.685, p < 0.02). It is also evident that the highest tertile of MABP (MABP £93 v. >101, HR = 1.748, p < 0.04), urban patients (rural v. urban, HR = 1.753, p < 0.05) and OHA (HR = 1.42, p < 0.08) p < 0.005) treatments are associated significantly with greater risk for CHD than compared with high 2-hBG, lower MABP, residence and insulin treatment. So the risk factors, 2-hBG, MABP, place of residence and treatment have significant associations for coronary heart disease (CHD) during their follow-up periods. For nephropathy, the effect of lower age (age £40 v. >40, HR = 0.343, p < 0.0001), middle (MABP ≤93.33 v. >93.33, HR = 1.906, p < 0.009) and highest tertile of MABP (MABP ≤93.33 v. >100.55, HR = 3.481, p < 0.0001) and illiterate (illiterate v. literate, HR = 2.039, p < 0.002) patients have greater risk for nephropathy. So it reveals that age, MABP and schooling have a significant association with nephropathy during follow-up period. It is only found that comparatively more lean patients (BMI: HR = 0.563, p < 0.007) have developed diabetic retinopathy. We also observe that lower 2-hBG (2-hBG £10 v. >10, HR=0.519, p < 0.001), illiterate (literate v. illiterate, HR = 1.628, p < 0.037), lowest BMI (BMI ≤21.46 v. >24.29, HR = 0.620, p < 0.03) have developed cataract. So it reveals that 2-hBG, BMI are negatively associated with cataract while illiterate patients had developed cataract during their follow-up period at a higher proportion. For pulmonary tuberculosis, comparatively more lean (BMI £21.46 v. £24.29, HR = 0.315, p < 0.0001; BMI £21.46 v. >24.29, HR = 0.380, p < 0.005) patients and family history of unknown diabetes (FHD: No v. unknown, HR = 2.064, p < 0.01) are more affected by pulmonary tuberculosis. It also shows that insulin (insulin v. OHA, HR = 0.323, p < 0.0005) treatment is not effective for TB. So for pulmonary tuberculosis, the risk factors, BMI, family history of diabetes (FHD) and treatment have significant associations with pulmonary tuberculosis. For other diseases, it is evident that comparatively lower age (age £40 v. >40, HR = 0.267, p < 0.0001) group, insulin (insulin v. OHA, HR = 0.75, p < 0.05) treatment and female (female v. male, HR = 0.619, p < 0.001) patients are more affected by other diseases during their follow up periods. So it reveals that age, sex and treatment are significantly associated with other diseases.
5. Discussion
In this study, we use competing risk hazard model for diabetes related complications data during the follow-up period. It is clear that multistate hazards models can be an ideal choice for analyzing the data which consider transition from no complication to complication. Our study revealed that almost two-thirds were male both at initial registration and also throughout the follow-up period. We also found that urban subjects were comparatively more than compared with rural or suburban. In our study we also found that average age ±SD was 47.07 ± 12.27. This indicates that older age is also a risk factor for T2DM. In our study we have taken 2887 patients, among them the independently individual prevalence of CHD, nephropathy, retinopathy, cataract, pulmonary tuberculosis and other disease were 5.1%, 5.7%, 6.1%, 5.6%, 2.7% and 10.9% respectively. In our study we observe that all the complications increased in the initial period of follow-up. The complications in the initial period of follow up may be attributed to late detection and registration of diabetes when they had already developed some complications. It is also possible that the complications might aggravate to such an extent that the many of them are lost to follow up.
The pathogenesis of the long term complications in diabetes mellitus is not fully known and controversies exist about why it occurs in some patients and not in others. This study made an attempt to define more clearly the risk factors influencing susceptibility to such complications in T2DM. There are a few clinical studies in this direction and focused only towards one complication at a time. Therefore, we attempted to do a follow-up study of T2DM patients with macro and micro vascular complications. This study demonstrates that an increased mean blood pressure was a risk factor for CHD, nephropathy, retinopathy and cataract in T2DM. These results are consistent with the finding of other studies [8] [9] [11] [13] -[17] . The presence of hypertension is a risk factor for development of the microvascular complications [9] [18] [19] . Our result is also consistent with this finding. We also show that male and illiterate patients are more affected by nephropathy. These results are also consistent with other studies [14] [20] . It is likely that illiterate people are poor and they live in rural areas and these patients belong to disadvantaged communities and their complications are detected in advanced stage when they have developed typical symptoms with weight loss and even complications like nephropathy. On the other hand the urban people with easy access to health, might prevent or reduce the diabetic complications like nephropathy. And it also has significant association with males. These findings are consistent with [14] . In our study, we also observe that female patients are also more affected by cataract. This result is also consistent with other studies [17] . We also observe that the epidemiological studies have documented tendencies for cataracts to occur more frequently among diabetics than in the general population [17] [21] . We have demonstrated the association between the increasing 2-hBG and the risk of long-term complications for cataract and other complications. Though many studies reported hyperglycemia as a risk factor for macrovascular complication [22] -[24] . The relation of 2-hBG to CHD in subjects with type 2 diabetes is reported as controversial in some studies [9] [25] and the multistate models provide evidence of such association. The two most world famous prospective studies -the Diabetes Complication Control Trial (DCCT) and the United Kingdom Prospective Diabetes Study (UK-PDS) concluded that strict monitoring and maintenance of normal blood glucose certainly prevents micro-vascular complications. For macrovascular complications, glycemic control could not confirm such prevention. In our study we reveal that increased age is also a major risk factor for CHD, retinopathy and cataract with T2DM. This result is also consistent with other studies [17] [25] -[27] . We also found that males have higher risk of nephropathy and TB as evident from the multistate models. These results are similar to other studies [14] [28] . It is also evident that obesity is positively associated with the complications. There is positive association of diabetes complications and older age. There is positive association between MABP and CHD, nephropathy, retinopathy, and cataract. We observe that insulin treatment is more effective than compared with other OHA for long-term complications with T2DM. In a recent study conducted in China, it is found that newly diagnosed T2DM patients treated with intensive insulin therapy is better remission for T2DM. Remission was attributed to early intervention with glucose control, reducing glucotoxicity and enabling pancreatic β-cell rest and recovery of function [29] . Different studies show that the disease progression leads to β-cells deterioration and to reduced secretion of insulin [30] . Early diagnosis and treatment of diabetes is essential to reducing or preventing the long term complications [31] [32] . These results are also consistent to our study for long term complications.
6. Conclusion
This study reveals that increase in blood pressure is a major risk factor for CHD and nephropathy in T2DM. We also revealed that urban participants were more affected by CHD whereas; rural population was the most vulnerable for developing nephropathy. We also found that male and illiterate patients are more affected by nephropathy. In our study, we also reveal that female and illiterate patients are also more influenced by cataract. Furthermore, we couldn’t prove that the increasing blood glucose is a major risk factor for complications in T2DM. Finally, we may conclude from this study that the multistate models can provide extensive results and it is evident that these transitional models are more likely to reveal the underlying relationships between the complications of diabetes mellitus and the potential risk factors on the basis of longitudinal data.
References
- (2012) IDF Diabetes Atlas. 5th Edition.
- Whiting, D.R., Guariguata, L., Weil, C. and Shaw, J. (2011) IDF Diabetes Atlas: Global Estimates of the Prevalence of Diabetes for 2011 and 2030. Diabetes Research and Clinical Practice, 94, 311-321. http://dx.doi.org/10.1016/j.diabres.2011.10.029
- Fowler, M.J. (2008) Microvascular and Macrovascular Complications of Diabetes. Clinical Diabetes, 26, 77-82. http://dx.doi.org/10.2337/diaclin.26.2.77
- Cox, D.R. (1972) Regression Models and Life Tables. Journal of the Royal Statistical Society, 34, 187-202.
- Farewell, V.T. (1979) An Application of Cox’s Proportional Hazard Model to Multiple Infection Data. Applied Statistics, 28, 73-75. http://dx.doi.org/10.2307/2346815
- Duckworth, W., Abraira, C., Moritz, T., Reda, D., Emanuele, N., Reaven, P.D., Zieve, F.J., Marks, J., Davis, S.N., Hayward, R., Warren, S.R., Goldman, S., McCarren, M., Vitek, M.E., Henderson, W.G. and Huang, G.D. (2009) VADT Investigators. Glucose Control and Vascular Complications in Veterans with Type 2 Diabetes. The New England Journal of Medicine, 360, 129-139.
- Holman, R.R., Paul, S.K., Bethel, M.A., Matthews, D.R. and Neil, H.A.W. (2008) 10-Year Follow-Up of Intensive Glucose Control in Type 2 Diabetes. The New England Journal of Medicine, 359, 1577-1589. http://dx.doi.org/10.1056/NEJMoa0806470
- Ueda, H., Matsumoto, N., Ishimura, E., Fukumoto, S., Shoji, T., Miki, T., et al. (2003) Factors Affecting Progression of Renal Failure in Patients with Type 2 Diabetes. Diabetes Care, 26, 1530-1534. http://dx.doi.org/10.2337/diacare.26.5.1530
- Boguslawa, N.S., Dariusz, M. and Wladyslaw, G. (2002) Risk of Macrovascular and Microvascular Complications in Type 2 Diabetes: Results of Longitudinal Design. Journal of Diabetes and Its Complications, 16, 271-276. http://dx.doi.org/10.1016/S1056-8727(01)00184-2
- Hu, G., Lindstrom, J., Valle, T.T., Eriksson, G., Jousilahti, P., Silventoinen, K., et al. (2004) Physical Activity, Body Mass Index, and Risk of Type 2 Diabetes in Patients with Normal or Impaired Glucose Regulation. Archives of Internal Medicine, 164, 892-896. http://dx.doi.org/10.1001/archinte.164.8.892
- Turner, R.C. (1998) The UK Prospective Diabetes Study. Diabetes Care, 21, C35-C38.
- Cox, D.R. (1975) Partial Likelihood. Biometrika, 62, 269-276. http://dx.doi.org/10.1093/biomet/62.2.269
- Sasso, F.C., Salvatore, T., Nicola, L.D., et al. (2006) Cardiovascular Risk Factors and Disease Management in Type 2 Diabetic Patients with Diabetic Nephropathy. Diabetes Care, 29, 498-503. http://dx.doi.org/10.2337/diacare.29.03.06.dc05-1776
- Agarwal, N., Senger, N.S., Jain. P.K. and Khare, R. (2011) Nephropathy in Newly Diagnosed Type 2 Diabetes with Special Stress on the Role of Hypertension. Journal of the Association of Physicians of India, 59, 145-147.
- Matthews, D.R., Stratton, I.M., Aldington, S.J., Holman, R.R. and Khner, E.M. (2004) UK Prospective Diabetes Study Group. Risk of Progression of Retinopathy and Vision Loss Related to Tight Blood Pressure Control in Type 2 Diabetes Mellitus: UKPDS 69. Archives of Ophthalmology, 122, 1631-1640. http://dx.doi.org/10.1001/archopht.122.11.1631
- Leelawattana, R., Pratipanawatr, T., Bunnag, P., Kosachunhanun, N., Suwanwalaikorn, S., Krittiyawong, S., et al. (2006) Thailand Diabetes Registry Project: Prevalence of Vascular Complications in Long-Standing Type 2 Diabetes. Journal of the Medical Association of Thailand, 89, S54-S59.
- Kim, S.I. and Kim, S.J. (2006) Prevalence and Risk Factors for Cataracts in Persons with Type 2 Diabetes Mellitus. Korean Journal of Ophthalmology, 20, 201-204. http://dx.doi.org/10.3341/kjo.2006.20.4.201
- Javier, F., Perez, C.F., Ruiz, I.M., de Gorospe Pérez-Jáuregui, C., Rodríguez, B.S., Losada, T.G. and Galindo, A.S. (2011) Microvascular Complications and Risk Factors in Patients with Type 2 Diabetes. Endocrinología y Nutrición, 58, 163-168. http://dx.doi.org/10.1016/j.endonu.2011.01.006
- Nathan, D.M., Cleary, P.A., Backlund, J.Y., Genuth, S.M., Lachin, J.M., Orchard, T.J., Raskin, P. and Zinman, B. (2005) Intensive Diabetes Treatment and Cardiovascular Disease in Patients with Type 1 Diabetes. New England Journal of Medicine, 353, 2643-2653. http://dx.doi.org/10.1056/NEJMoa052187
- Sayeed, M.A., Khanam, P.A., Hossain, M.M., et al. (1999) Diabetic Subjects with Severe Hyperglycemia and Proteinuria Are More Prevalent in Rural than Urban and in Poor than Rich People. Diabetes and Endocrine Journal, 27, 35-40.
- Klein, B.E., Klein, R. and Moss, S.E. (1985) Prevalence of Cataracts in a Population-Based Study of Persons with Diabetes Mellitus. Ophthalmology, 92, 1191-1196. http://dx.doi.org/10.1016/S0161-6420(85)33877-0
- Lehto, S., Ronnemaa, T., Haffner, S.M., Pyörälä, K., Kallio, V. and Laakso, M. (1997) Dislipidemia and Hyperglycemia Predict Coronary Heart Disease Events in Middle-Aged Patients with NIDDM. Diabetes, 46, 1354-1359. http://dx.doi.org/10.2337/diab.46.8.1354
- Gall, M.A., Borch-Johnsen, K., Hougaard, P., Nielsen, F.S. and Parving, H.H. (1995) Albuminuria and Poor Glycemic Control Predict Mortality in NIDDM. Diabetes, 44, 1303-1309. http://dx.doi.org/10.2337/diab.44.11.1303
- Haffner, S.M. (1999) Epidemiological Studies on the Effects of Hyperglycemia and Improvement of Glycemic Control on Macrovascular Events in Type 2 Diabetes. Diabetes Care, 22, C54-C56.
- Wilson, P.W.F. and Meigs, J.B. (2008) Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease: A Pivotal Role for Metabolic Factors. European Heart Journal, 10, B11-B15.
- Duckworth, W., Abraira, C., Moritz, T., Reda, D., Emanuele, N., Reaven, P.D., Zieve, F.J., Marks, J., Davis, S.N., Hayward, R., Warren, S.R., Goldman, S., McCarren, M., Vitek, M.E., Henderson, W.G., Huang, G.D. for VADT Investigators (2009) Glucose Control and Vascular Complications in Veterans with Type 2 Diabetes. New England Journal of Medicine, 360, 129-139. http://dx.doi.org/10.1056/NEJMoa0808431
- Raman, R., Pal, S.S., Adams, J.S.K., Rani, P.K., Vaitheeswaran, K. and Sharma, T. (2010) Prevalence and Risk Factors for Cataract in Diabetes: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study. Investigative Ophthalmology & Visual Science, 51, 6253-6261. http://dx.doi.org/10.1167/iovs.10-5414
- Kuo, H.S., Chang, H.J., Chou, P., Teng, L. and Chen, H.H. (1999) A Markov Chain Model to Assess the Efficacy of Screening for Non-Insulin Dependent Diabetes Mellitus (NIDDM). International Journal of Epidemiology, 28, 233-240. http://dx.doi.org/10.1093/ije/28.2.233
- Weng, J., Li, Y., Shi, L., Zhang, Q., Zhu, D., Hu, Y., Yan, X., Tian, H., et al. (2008) Effect of Intensive Insulin Therapy on β-Cell Function and Glycaemic Control in Patients with Newly Diagnosed Type 2 Diabetes: A Multicentre Randomized Parallel-Group Trial. Lancet, 371, 1753-1760. http://dx.doi.org/10.1016/S0140-6736(08)60762-X
- Absood, A., Gandomani, B., Zaki, A., Nasta, V., Michail, A., Habib, P.M. and Hodish, I. (2013) Insulin Therapy for Pre-Hyperglycemic Beta-Cell Endoplasmic Reticulum Crowding. PLoS ONE, 8, Article ID: e54351. http://dx.doi.org/10.1371/journal.pone.0054351
- The Diabetes Control and Complications Trail Research Group (1993) The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. New England Journal of Medicine, 329, 977-986.
- Alder, A.I., Stevens, R.I., Manley, S.E., Bilous, R.W., Cull, C.A. and Holman, R.R. on Behalf of the UKPDS Group (2003) Development and Progression of Nephropathy in Type 2 Diabetes: The United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney International, 63, 225-232. http://dx.doi.org/10.1046/j.1523-1755.2003.00712.x
NOTES
![]()
*Corresponding author.


