Open Journal of Modern Neurosurgery
Vol.3 No.2(2013), Article ID:29634,9 pages DOI:10.4236/ojmn.2013.32003
Neurocritical Care Training for the Neurosurgery Resident*
1Department of Neurosurgery, University of New Mexico Medical Center, Albuquerque, USA
2Department of Neurosurgery, The Johns Hopkins Hospital, Baltimore, USA
Email: #paulkaloostian@hotmail.com
Copyright © 2013 Paul E. Kaloostian et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received February 7, 2013; revised March 8, 2013; accepted March 16, 2013
Keywords: Neurocritical Care; Neurosurgery Resident; Neurosurgery Survey; Neurointensivist
ABSTRACT
Introduction: Recent data has associated favorable outcomes in patients who were treated in a “semi-closed” intensive care unit and attended to by a devoted team of neurointensivists as opposed to the neurosurgeons. This has led many to question the need for dedicated critical care education in the neurosurgical residency training program. Our aim was to determine what current neurosurgery residents and program directors/chairman thoughts were on NCC education in neurosurgical resident training, and to discuss possible methods to allow for collaboration between the NCC team and the neurosurgeons. Methods: Surveys were sent out electronically to all residency programs. Thirty-nine responses from junior residents, 36 responses from senior/chief residents, and eight responses from program directors/chairman were obtained. Results: No statistical difference between the majority responses of the different level residents and between program directors/chairman and combined resident responses. Conclusions: Clearly, neurosurgery residents of all levels and program directors/chairman value NCC education and see a valuable role for this knowledge in their future. Most residents, however, do not want to spend an additional year of fellowship training to become certified neurointensivists. We discuss the role of NCC education in residency training and possible solutions to allow collaboration between the NCC team and the neurosurgical team.
1. Introduction
Over the last decade, neurosurgical care has evolved into a multi-specialty, multi-modality collaboration. In the past, patient care was largely under the direction of the neurosurgery team, as residents and attendings would manage complex patients with multiple organ pathologies. The neurosurgery intensive care unit (NICU) ran as an “open” unit, allowing the admitting surgeon to remain the primary provider throughout the patient’s stay, bringing in consult teams on a case-by-case basis. More recently, however, a “semi-closed” model has become more popular, in which the admitting physician transfers much of the patient care over to a subspecialized and highly trained group of neurointensivists (NI) [1].
Recent data has associated favorable outcomes in neurosurgical patients who were treated in a “semi-closed” ICU setting and attended to by a devoted team of NIS [2]. These NIs have been well-trained in a variety of intensive care unit (ICU) procedures (such as tracheostomies, bronchoscopes, arterial lines, central lines, and percutaneous gastrostomies) and are knowledgeable about neurological pathology. They are also familiar with the unique physiologic considerations that must be taken into when managing brain and spinal cord-injured patients, and can act efficiently to prevent secondary insults in the postoperative or intensive care setting. This customized care has been shown to improve outcome and diminish hospital costs [1].
Despite these benefits, the semi-closed model also led to ambiguity regarding the roles of the neurosurgeon and NI in managing the critically ill neurosurgical patient. The result is often an imprecise or overlapping set of responsibilities, with each party working with or against the other in an effort to maintain longitudinal care. The purpose of this study was to understand how neurosurgery residents of all levels and program directors or chairmen throughout the United States felt about this shifting paradigm in patient care. Our goal was to identify a general consensus or any common themes in opinions regarding NICU care, NI versus neurosurgery involvement in the intensive care setting, and the existing versus optimal level of neurocritical care education in residency programs nationwide.
2. Methods
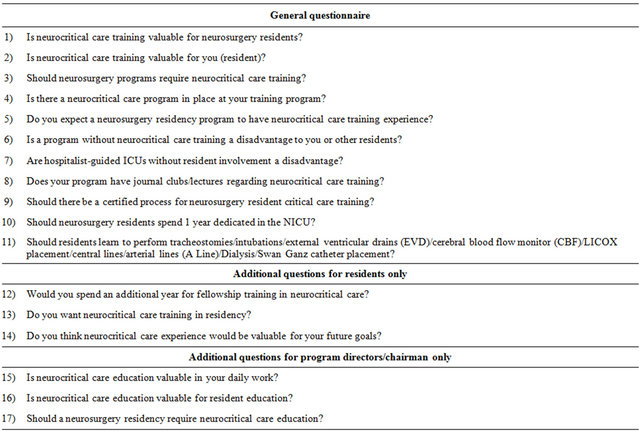
Surveys were sent out electronically to all residency programs in the United States. Responses from residents, program directors/chairman were collected and the results were tallied in blind fashion. Fisher exact test was performed to compare responses between junior and senior/chief residents, and between residents and program directors/chairman; a probability value of <0.05 was considered to be statistically significant. See Table 1 for the full questionnaire.
3. Results
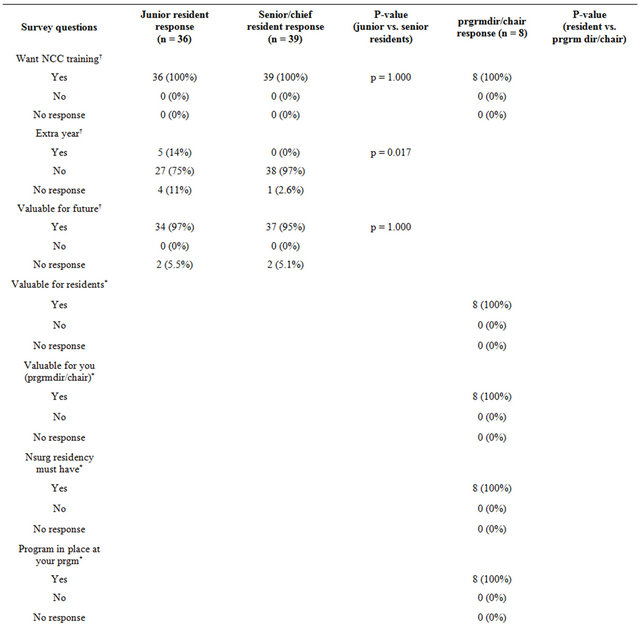
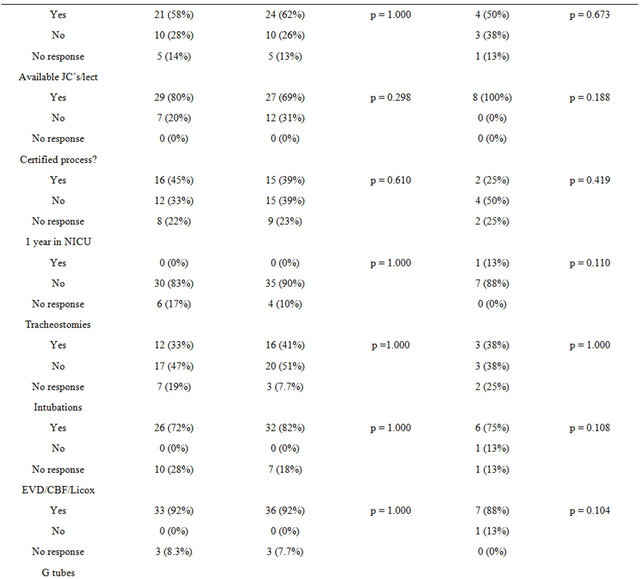
The results of the questionnaire are summarized in Tables 2 and 3.
Thirty-nine responses from junior residents, 36 responses from senior/chief residents, and eight responses from program directors/chairman were obtained. No statistical difference (p < 0.05) was found between the yes/no response rate between the different-level residents, with two exceptions (Table 2). In response to the question “Would you spend an additional year for fellowship training in neurocritical care?” 27 (75%) of the junior residents and 38 (97%) of the senior residents, responded “no” (p = 0.017). In response to the question “Should residents learn to perform tracheostomies/intubations/ external ventricular drains (EVD)/cerebral blood flow monitor(CBF)/LICOX placement/central lines/arterial lines (A Line)/dialysis/Swan Ganz catheter placement?” 24 (67%) of the junior residents and 33 (85%) of the senior residents responded “yes” (p = 0.004).
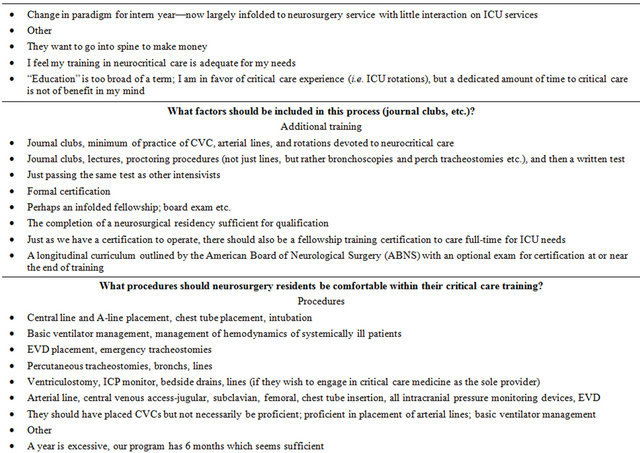
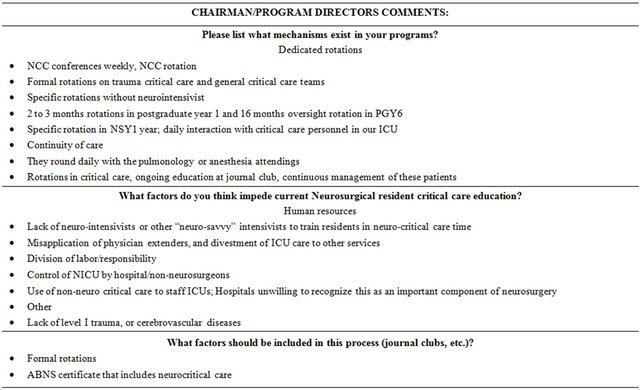
No statistical difference was found between program directors/chairman and resident responses (Table 2). Additional comments and answers to open-ended questions regarding the value, need, and critique of critical care education are summarized in Table 3.
4. Discussion
Neurosurgical care has undergone significant changes over the last decade. The shifting paradigms of medical care have been especially apparent in the setting of the NICU. What was once a small specialized unit that catered to severely ill, ventilated patients has evolved into a large, multi-specialty and multi-modal entity in which not only neurosurgeons, but also anesthesiologists, neurologists and critical care specialists are charged with caring for an increasingly complex patient population [3]. The development of the neurointensive case sub-specialty was largely driven by high rates of medical errors and inadequate care nationwide; in response, physicians in medicine, anesthesiology and critical care began working together to provide highly specialized neurocritical care in a collaborative setting [4].
Since the introduction of the closed or semi-closed unit, the NI has emerged as a dominant figure in the non-operative care of critically ill neurosurgical patients. However, the role of the NI has been an area of interest and often contention by those in neurosurgery and other related fields. Additionally, there has been some reluctance to accept the semi-closed model for fear of entrusting the care of their patients to a NICU staff that may not have any neurosurgical expertise. It is understandable that the neurosurgeon would wish to participate in the care of their critically ill patient, even if a specialized neurocritical care team was available.
Despite these qualms, quality and efficacy studies have shown a clear improvement in outcomes following the implementation a specialized, NI-led NICU. In 2002, Pronovost et al. demonstrated that high intensity ICUs were associated with reduced hospital and ICU mortality and length of stay [5]. This association between intensivist-led care and improved patient outcome has also held up in NICU setting. A meta-analysis of 12 studies with 24,520 patients comparing outcomes before and after implementation of NIs demonstrated significantly lower mortality rates (p = 0.01) and improved outcomes (p < 0.0001) in patients treated in specialized NICU’s [1]. Varelas et al. compared outcomes of patients treated before and after implementation of NIs in the NICU and identified three critical factors that improved neurosurgical patient care: 1) implementing a dedicated NI in the NICU; 2) attention to detail; 3) better monitoring procedures. They also emphasized the crucial role of neurosurgery nurse whom they described as “the most important monitor” [6]. Further studies have shown that patients with traumatic brain injuries [7], non-traumatic intracerebral hemorrhage [8], and aneurysmal subarachnoid hemorrhage [9] are more likely to receive definitive treatment, experience better outcomes, shorter hospital stays [10] and have equal or lower mortality rates when treated by a dedicated multidisciplinary NICU team. These improved outcomes were associated with a positive impact on hospital savings and diminished overall hospital costs [9].
The successes of the semi-closed NICU system has raised questions in the neurosurgical education community, with educators and students asking: what role should residents play in this process? How much should they learn? Do they need to learn this information? How much neurocritical care education is too much and how much is too little? Such questions were the impetus for our study. Though neurointensivists have emerged as leaders in many NICU’s to provide centralized, proto
Table 1. Survey questions.
col-driven therapy, neurosurgeons have a responsibility to become educated in the treatment of critically ill patients. Familiarity with the complications associated with this patient population ensures that the neurosurgeon will be able to provide the best care no only during but also after the acute event. Furthermore, the NICU provides a unique classroom in which one can better appreciate the nuances of neurologic disease processes. For instance, all participating specialties—neurology, neurosurgery, anesthesiology—have benefited from and continue to draw insights into the understanding of brain death and neurologic outcome [11].
Our results suggest that neurosurgical residents and program directors/chairman believe critical care education to be an essential component of their training programs. Most of the respondents agreed that they would be at a disadvantage if they did not receive critical care training, and that that they expected to be taught how to perform or place tracheostomies, intubations, EVDs, CBF monitors, LICOX, A lines, and dialysis/Swan Ganz catheters. On the other hand, a majority of the residents stated that they would not choose to spend an additional year for fellowship training in neurocritical care. Answers from the additional comments section of the survey reflect a belief that while neurosurgeon should be knowledgeable in the general management of critical care patients, the presence and dominance of NIs in the NICU renders a critical care fellowship unnecessary, except for those who want to become certified neurointensivists. A few respondents explicitly stated that a standardized exam and certification at the end of the critical care experience or residency program would be the most optimal way of ensuring that residents had had sufficient exposure to critical care medicine.
One factor that inhibits a standardized, nationwide change in the residency curriculum is the varying nature of neurosurgical practices across the country. Most neurosurgeons practice in community hospitals with a private practice or part-private/part-academic environment. There, neurocritical care teams can have significantly different skill sets and responsibilities in comparison to those in large high-volume academic medical centers. Thus, in smaller community hospitals, the neurosurgeon may well be appointed as the main care provider for critically ill patients, thereby necessitating adequate prior critical care training.
In spite of the varying levels of interest or motivations in critical care education, it is clear that the NICU provides an indispensable learning opportunity that enhances the understanding of the physiologic, pharma-
Table 2. Survey responses.
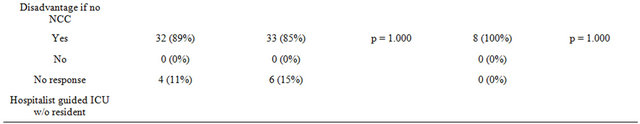
Continued
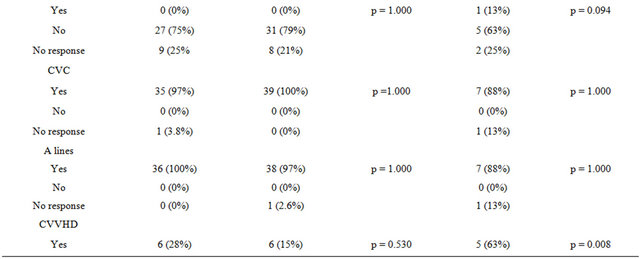
Continued
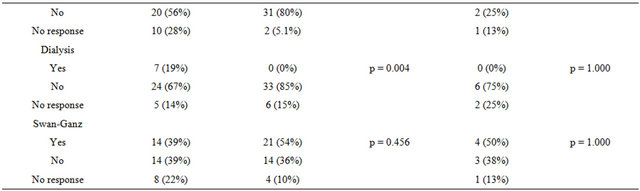
†Questions for residents only. *Questions for program directors/chairs only.
Table 3. Additional comments.
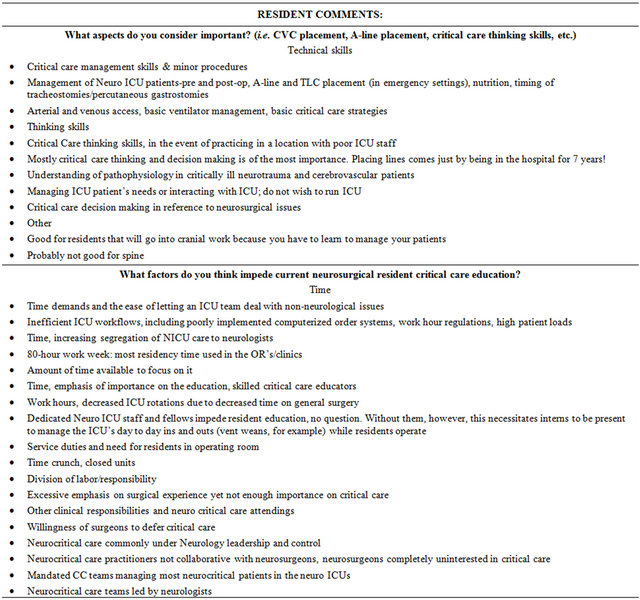
Continued
cologic, microbiologic, and pathologic features of the neurosurgical patient. The experience also teaches the neurosurgeon how to develop a systematic approach and to work cooperatively with multidisciplinary team, and especially with the neurointensivists. The skills acquired from this experience, such as risk assessment and optimization, can only strengthen the curriculum, and further ensure the safety of these patients [12].
Ultimately, collaboration between the NCC team and the neurosurgical team—including residents at all levels—is needed to optimize both patient care and clinical education. Factors that can facilitate this collaboration include standardized rounding times where the neurosurgeons and NCC team meet to discuss the plans for the day, having a resident member of the neurosurgical team involved in rounds with the NCC team, allowing NCC team members into the operating room to observe neurosurgical procedures, weekly or monthly lectures from the NCC team on various topics related to critical care, and neurosurgical presentations by residents detailing important neurosurgical considerations to the entire NCC team. These strategies may help create a more collaborative environment in the NICU, which, in turn, will allow for the best possible patient care as well as a valuable learning experience for the neurosurgery residents.
Limitations of our study begin with the low power due to the few responses from residents and program directors nationwide. However, this is the best data in the neurosurgery literature thus far. Common themes and opinions come through clearly in the survey responses. This is the first study attempting to document this problem in neurosurgery resident education and undoubtedly a larger study, perhaps with the American Association of Neurological Surgeons and Congress of Neurological Surgeons, in accordance with the Senior Neurosurgical Society, needs to be done to confirm our initial results.
5. Conclusion
Our study demonstrates that neurosurgery residents of all levels and program directors/chairman value NCC education and see a valuable role for this knowledge in their future. Most residents however, express disinterest in an additional year of fellowship training to become certified neurointensivists. Likewise, the majority of program directors/chairman who were responded to the survey agrees that a year solely dedicated to NCC is not warranted. A variety of procedures such as intracranial monitoring devices, arterial lines, intubations, and central lines are clearly valued by neurosurgery residents as part of the requisite neurosurgical repertoire. Perhaps a shift in current standard neurosurgery resident training to include a focused 3 - 6 months rotation on the ICU service working as a team with the hospitalists may be an optimal educational experience. Additionally, a standardized neurocritical care examination (either written or oral) for all residents could be implemented to allow neurosurgery residents to practice neurocritical care in the future, should they so desire. These program additions would allow neurosurgeons to better tailor their education according to their interest or expected involvement in the critical care setting. Finally, we discuss certain key factors that may help in the collaborative process between the NCC team and the neurosurgical team.
REFERENCES
- A. H. Kramer and D. A. Zygun, “Do Neurocritical Care Units Save Lives? Measuring the Impact of Specialized ICUs,” Neurocritical Care, Vol. 14, No. 3, 2011, pp. 329- 333. doi:10.1007/s12028-011-9530-y
- T. P. Bleck, “The Impact of Specialized Neurocritical Care,” Journal of Neurosurgery, Vol. 104, No. 5, 2006, pp. 709-710, Discussion 710. doi:10.3171/jns.2006.104.5.709
- E. F. Wijdicks, W. R. Worden, A. Miers and D. G. Piepgras, “The Early Days of the Neurosciences Intensive Care Unit,” Mayo Clinic Proceedings, Vol. 86, No. 9, 2011, 903-906. doi:10.4065/mcp.2010.0815
- J. Gasperino, “The Leapfrog Initiative for Intensive Care Unit Physician Staffing and Its Impact on Intensive Care Unit Performance: A Narrative Review,” Health Policy, Vol. 102, No. 2, 2011, pp. 223-228. doi:10.1016/j.healthpol.2011.02.005
- P. J. Pronovost, D. C. Angus, T. Dorman, K. A. Robinson, T. T. Dremsizov and T. L. Young, “Physician Staffing Patterns and Clinical Outcomes in Critically Ill Patients: A Systematic Review,” The Journal of the American Medical Association, Vol. 288, No. 7, 2002, pp. 2151-2162. doi:10.1001/jama.288.17.2151
- P. N. Varelas, D. Eastwood, H. J. Yun, et al., “Impact of a Neurointensivist on Outcomes in Patients with Head Trauma Treated in a Neurosciences Intensive Care Unit,” Journal of Neurosurgery, Vol. 104, No. 5, 2006, pp. 713- 719. doi:10.3171/jns.2006.104.5.713
- H. C. Patel, D. K. Menon, S. Tebbs, R. Hawker, P. J. Hutchinson and P. J. Kirkpatrick, “Specialist Neurocritical Care and Outcome from Head Injury,” Intensive Care Medicine, Vol. 28, No. 5, 2002, pp. 547-553. doi:10.1007/s00134-002-1235-4
- M. A. Mirski, C. W. Chang and R. Cowan, “Impact of a Neuroscience Intensive Care Unit on Neurosurgical Patient Outcomes and Cost of Care: Evidence-Based Support for an Intensivist-Directed Specialty ICU Model of Care,” Journal of Neurosurgical Anesthesiology, Vol. 13, No. 2, 2001, pp. 83-92. doi:10.1097/00008506-200104000-00004
- O. Samuels, A. Webb, S. Culler, K. Martin and D. Barrow, “Impact of a Dedicated Neurocritical Care Team in Treating Patients with Aneurysmal Subarachnoid Hemorrhage,” Neurocritical Care, Vol. 14, No. 3, 2011, pp. 334-340. doi:10.1007/s12028-011-9505-z
- J. I. Suarez, O. O. Zaidat, M. F. Suri, et al., “Length of Stay and Mortality in Neurocritically Ill Patients: Impact of a Specialized Neurocritical Care Team,” Critical Care Medicine, Vol. 32, No. 11, 2004, pp. 2311-2317.
- A. H. Ropper, S. K. Kennedy and N. T. Zervas, “Neurological and Neurosurgical Intensive Care,” University Park Press, Baltimore, 2004.
- E. A. Pereira, H. Madder, J. Millo and C. F. Kearn, “Neurosciences Intensive Care Medicine in Initial Neurosurgical Training,” British Journal of Neurosurgery, Vol. 23, No. 2, 2009, pp. 193-196. doi:10.1080/02688690802512841
Abbreviations
EVD: extraventricular drain;
CBF: cerebral blood flow;
CVVHD: continuous veno-venous hemodialysis;
ICU: intensive care unit;
NCC: neurocritical care;
NICU: neurosurgery intensive care unit;
Nsurg: neurosurgery;
NOTES
*Acknowledgements/conflicts of interest: none.
#Corresponding author.

