Open Journal of Modern Neurosurgery
Vol.3 No.1(2013), Article ID:27301,3 pages DOI:10.4236/ojmn.2013.31001
De Novo Cavernous Malformation after Radiosurgery
Department of Neurosurgery, Hospital Garcia de Orta, Almada, Portugal
Email: cata_pv@hotmail.com
Received December 28, 2011; revised January 31, 2012; accepted March 7, 2012
Keywords: Cavernous Malformation; Radiosurgery; Radiation Induced Cavernoma; Grade II Astrocytoma
ABSTRACT
Background: The general use of radiation therapy and radiosurgery as first-line or adjuvant treatment of central nervous system (CNS) lesions has been associated with several harmful effects. Case Description: We report the case of a 16-year-old male patient, submitted at the age of seven to surgical removal of a world heath organization (WHO) grade II diffuse astrocytoma and referred for adjuvant radiosurgery after three further surgeries due to local recurrences. Seven years after radiosurgical treatment, he presented with symptoms of intracranial hypertension. Magnetic resonance imaging (MRI) at the time showed a cavernous malformation in the tumor bed, histologically confirmed, without tumoral recurrence. Conclusion: This case report emphasizes the relation between radiosurgery and the appearance of the novo cavernous malformations, only described previously in one adult patient.
1. Introduction
The use of radiation therapy and radiosurgery as primary or adjuvant treatment of central nervous system (CNS) tumors has been associated with a wide range of deleterious effects, such as diffuse necrosis of white matter, demyelinization, reactive astrocytosis, cerebral atrophy, dystrophic mineralization, arteriopathy and the development of other tumors and cavernous malformations (CM) [1]. Radiation induced cavernomas were first described by Ciricillo et al. in 1994 [1]. Although this type of complication is rare, the number of publications on the subject has grown in recent years [1-6]. CM are present in about 0, 5% of the general population and they comprise 16% of all cerebrovascular malformations [7]. The lesions can occur sporadically or as an inherited trait in some families. The familial form is transmitted as an autossomal dominant trait associated with 3 genetic loci [7]. Both sporadic and familial forms have incomplete clinical and radiological penetrance. Histologically, cavernomas are composed of dilated, contiguous vascular channels, with fragile walls, lined with just one endothelial layer, without any brain parenchyma in between [7]. Calcifications and hemorrhage in different grades can be present. CM are angiographically occult lesions. Despite the fact that during surgery tiny arterial afferents and venous efferents can sometimes be demonstrated, the size and flow of these vessels lies beneath the threshold depictable with angiography. On computed tomography (CT), CM are hyperdense and usually calcified. Magnetic resonance imaging (MRI) is the most sensible and specific imaging modality for the diagnosis of these lesions. Typical MRI features include a mixed signal lesion with “popcorn” appearance surrounded by a hypointense rim.
We report the case of a 16-year old boy with a low grade astrocytoma treated with surgery and radiosurgery, who subsequently developed a cavernous malformation in the area of the radiated bed.
2. Case Report
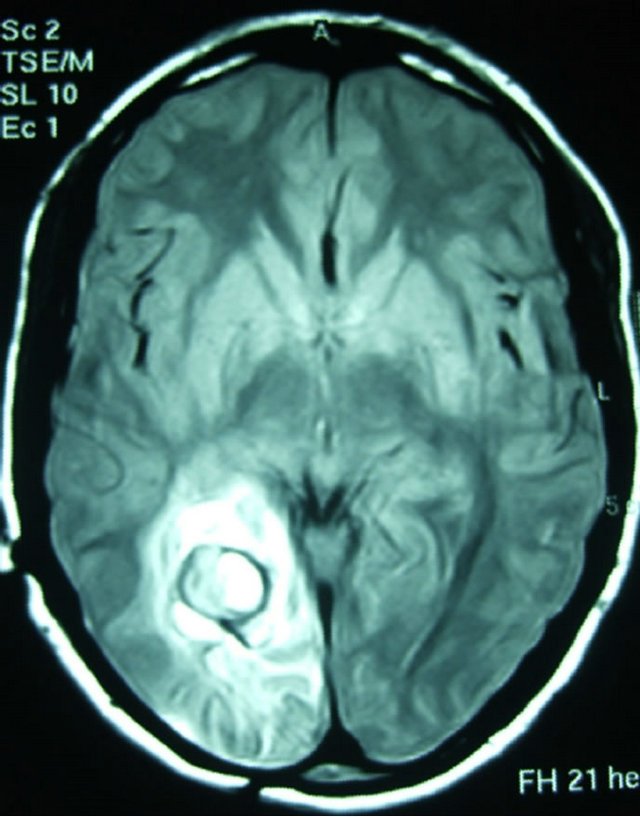
A seven-year old boy, presented with a short course intracranial hypertension. CT and MRI demonstrated a large contrast enhancing mass adjacent to the right atrium expanding into the deep white matter of the parietooccipital region. He underwent a radical resection of the tumor with no deficits and neuropathology reported a diffuse astrocytoma. The tumor was seen to recur and the patient was reoperated for three times, always with radical resections leaving a small mass attached to the choroids plexus in the right atrium. At the age of nine and after the last surgical resection, he was referred for adjuvant radiosurgery in order to improve local disease control. He received a total dose of 36 Gy in a single treatment at another institution. Since then no recurrence was ever detected in follow-up MRIs. At the age of 16, seven years after radiosurgery, he presented with recurring symptoms of intracranial hypertension, namely headache and nausea, without focal neurological deficits. MRI at the time showed a spherical right occipital subcortical peri-atrial mass, at the previous tumor bed with signal heterogeneity. It was isointense and hyperintense on T1 and hyperintense on T2-weighted imaging, compatible with recent hemorrhage, and also showed a hypointense ring surrounding the lesion in T2-weighted imaging “Figure 1”. He was submitted to surgical removal of the lesion. The lesion was easily demarcated and totally removed, with an uneventful post-operative period. The neuropathological diagnosis disclosed a CM “Figure 2”.
In the last imaging follow up (24 months after surgery) there were no clinical or imaging signs of either tumor or CM recurrence.
3. Discussion
In the revision of the literature on de novo CM of the CNS after radiotherapy, there are about 80 cases reported, in adults and children [1-6]. However there is just one case reported of a CM occuring after radiosurgery treatment in an adult after 2 cycles of treatment, with a latency period of 2 years [5].
These lesions are rare and since they were first described, the association with radiation therapy has been surrounded by controversy. The complications of radiation therapy, whole-brain radiotherapy or radiosurgery, depend on therapy related factors such as total radiation dose, volume of irradiated parenchyma and associated use of chemotherapy, and factors inherent to the patient,
 (a)
(a)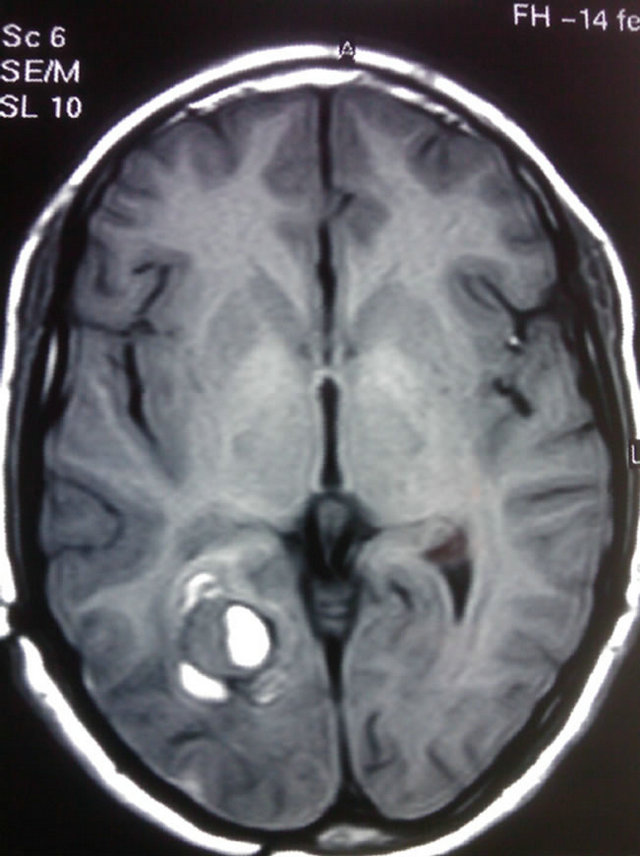 (b)
(b)
Figure 1. Axial T2 (a) and T1 (b) MRI scan showing a round occipital subcortical lesion, hyperintense lesion with a hypointense rim on T2 and iso/hyperintense on T1.
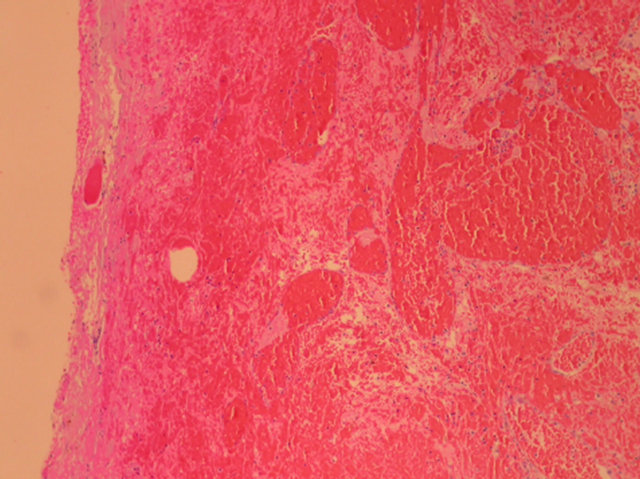
Figure 2. Hematoxylin-eosin staining showing a compact mass of hyalinised vascular channels without interposed brain parenchyma, typical of cavernous malformation.
such as age, immune status, genetic factors and type of primary tumor [1]. The latency period is variable, from one to 26 years, between the first radiation treatment and the diagnosis of CM. For this reason, the follow-up period has to be long. This latency period is inversely related to the total radiation dose. The majority of cases occur with radiation dose of more than 30 Gy [4].
There are two main explanations for the appearance of CM in patients treated with radiotherapy. The first supports the idea that CMs are pre-existent lesions that develop and are found just after the radiation treatment. The second theory sustains that CMs are caused by a proliferating vasculopathy that is started by the action of radiation in the cerebral vasculature, both locally and distally [2,8]. The increased incidence of angiographically occult vascular malformation in children after radiotherapy may be linked to the high levels of angiogenic factors found in children compared with adults [3]. The pathogenesis of cavernous hemangiomas following radiotherapy is believed to result from injury to vascular structures because the radiotherapy stimulates the upregulation of angiogenesis factors such as vascular endothelial growth factor and basic fibroblast growth factor. This upregulation results in mineralizing microangiopathy, which leads to luminal narrowing in the smaller blood vessels in the brain. Stimulation of such growth factors, which are found in cavernous hemangiomas, may explain increased CM formation following radiotherapy [3].
Indications for surgery are of course dependent on patient symptoms, as well as the size, number and location of the CM. Conservative treatment is advised in asymptomatic patients with no hemorrhage, but a close follow up is recommended [3].
The present case report may suggest that more focused forms of high dose radiation treatment, like radiosurgery, can also induce the development of CM. In our patient the latency period was 7 years after a radiosurgery dose of 36 Gy, in accordance with the previously reported patients submitted to whole-brain radiotherapy. To support the cause-effect relation between radiosurgery and the appearance of the novo CM is the fact that the location of the cavernoma was the same as the residual glioma, which was submitted to radiosurgery.
With the incremental use of radiosurgery in recent years for the treatment of both benign brain tumors and arteriovenous malformations, the development of CM after this form of treatment will probably increase in the future, given the long latency period allowed by these diseases.
4. Conclusion
In the light of present knowledge, it is difficult to deny that the development of the novo CM is a rare and late complication of radiation treatment, either radiotherapy or radiosurgery as depicted in the present case. The increasing number of reported cases, especially in children, should make us more aware of this association, recommending imaging follow up whenever the clinical symptoms so justify.
REFERENCES
- J. F. Martinez-Lage, I. de la Fuente, J. R. de San Pedro, J. L. Fuster, M. A. Pérez-Espejo and M. T. Herrero, “Cavernomas in Children with Brain Tumors: A Late Complication of Radiotherapy,” Neurocirugia, Vol. 19, 1998, pp. 50-54.
- A. Azevedo, D. Salgado, I. Costa, M. L. Quintal, J. M. B. Marques and P. Pereira, “Radiation Induced Cavernomas,” Sinapse, 2006, pp. 1-6.
- S. Burn, R. Gunny, K. Philips, M. Gaze and R. Hayward, “Incidence of Cavernoma Development in Children after Radiotherapy for Brain Tumors,” Journal of Neurosurgery, Vol. 106, No. 5, 2007, pp. 379-383.
- M. Furuse, S. I. Miyatake and T. Kuroiwa, “Cavernous Malformation after Radiation Therapy for Astrocytoma in Adult Patients: Report of 2 Cases,” Acta Neurochirurgica, Vol. 147, No. 10, 2005, pp. 1097-1101. doi:10.1007/s00701-005-0579-2
- Y. Iwai, K. Yamanaka and M. Yoshimura, “Intracerebral Cavernous Malformation Induced by Radiosurgery. Case Report,” Neurologia Medico Chirurgica, Vol. 4, No. 4, 2007, pp. 171-173. doi:10.2176/nmc.47.171
- S. M. Nimjee, C. J. Powers and K. R. Bulsara, , “Review of the Literature on the Novo Formation of Cavernous Malformations of the Central Nervous System after Radiation Therapy,” Neurosurgical Focus, Vol. 21, No. 1, 2006, p. e4.
- J. E. Conway and D. Rigamonti, “Cavernous Malformations: A Review and Current Controversies,” Neurosurgery Quarterly, Vol. 16, No. 1, 2006, pp. 15-23. doi:10.1097/01.wnq.0000203021.93797.a4
- P. W. Detwiler, R. W. Porter, J. M. Zabramski and R. F. Spetzler, “De Novo Formation of a Central Nervous System Cavernous Malformation: Inplications for Predicting Risk of Hemorrhage. Case Report and Review of the Literature,” Journal of Neurosurgery, Vol. 87, No. 4, 1996, pp. 629-632. doi:10.3171/jns.1997.87.4.0629

