Open Journal of Thoracic Surgery
Vol.1 No.2(2011), Article ID:9082,3 pages DOI:10.4236/ojts.2011.12002
Graft Quality Control with the Traditional Roller Pump Flow Measurement in Comparison to the Transit-Time Flow Measurement
![]()
Depapartment of Cardiovascular Surgery, University Hospital Duesseldorf, Duesseldorf, Germany.
Email: hannan.dalyanoglu@med.uni-duesseldorf.de
Received September 18th, 2011; revised October 29th, 2011; accepted November 13th, 2011.
Keywords: Coronary Artery Bypass Grafting, Flow Measurement, Quality Control
ABSTRACT
Objective: Vein graft quality control had been traditionally done for more than 20 years with a roller-pump flow measurement (RPFM) in our institute until off-pump coronary artery bypass grafting was introduced as the standard technique of myocardial revascularization in the year 2009 in our institute. In this study, the RPFM method was compared with the Transit-time flow measurement (TTFM). Patients and Methods: From February to September 2005, 31 patients (5 females) undergoing CABG in our institute were included into the study. All the patients were operated with cardiopulmonary bypass. In those patients, 27 distal anastomoses were done with the left internal thoracic artery and 99 anastomoses were done with vein grafts. Those 99 vein graft were assessed both, with the RPFM method and TTFM method. Results: CABG could be safely performed in all cases. In all target vessels, the RPFM method overestimated bypass flow compared to the TTFM method, and simple linear regression revealed no correlation between the TTFM measurement and the RPFM measurement (r = 0.08, p = 0.21). There were two cases in which a graft problem could be detected only with TTFM method, even in our small patient cohort. Conclusion: The present study suggests that the TTFM method is clearly superior to the traditional RPFM method and we believe now that TTFM should be performed routinely in all CABG to improve patient care and quality of surgical results.
1. Introduction
Transit-time flow measurement (TTFM) is the most widely used technique for intra-operative graft quality control in coronary artery bypass surgery (CABG) [1-3]. However, for more than 20 years vein graft quality control had been traditionally done with a roller-pump flow measurement (RPFM) as the standard method, up to the time when offpump coronary artery bypass grafting was introduced as the standard revascularization method in the year 2009 at our institute. According to RPFM, the proximal side of a vein bypass is cannulated and connected with a roller-pump after completion of the distal anastomosis. Thereafter, a cardioplegic solution is perfused with a constant pressure of 80 mmHg and the flow rate is measured [4]. The aim of the present study is to compare TTFM with RPFM.
2. Patients and Methods
From February to September 2005, 31 patients (5 females)
undergoing CABG at our institute were included into the study. All patients had a preoperative left ventricular ejection fraction > 50%. The average age was 67 years. Twenty four (77%) patients undergoing CABG had a left main stem stenosis. Six patients (19%) suffered from diabetes mellitus, and eight patients (26%) had a myocardial infarction in their medical history. All patients were operated with cardiopulmonary bypass for ioslated coronary revascularization. In those patients, 27 distal anastomoses were done with the left internal thoracic artery and 99 anastomoses were done with vein grafts. Those 99 vein grafts including 4 grafts to the left anterior descending artery (LAD), 23 grafts to the diagonal artery (Dx), 44 grafts to the obtuse marginal artery (OM) and 28 grafts to the right coronary artery (RCA) were evaluated in this study. A sequential grafting technique was not applied in any of the patients. After completion of the distal vein graft anastomoses, a cold blood cardioplegic solution was given through the vein grafts using a roller pump with the perfusion pressure of 80 mmHg and the flow rate through these grafts was assessed. After the patients were weaned from cardiopulmonary bypass, these vein grafts were controlled with a TTFM device with the mean blood pressure of 80 mmHg (Medistim VeriQ System, Oslo).
Results are presented as the mean ± standard deviation. Student’s t test was used for comparison of flow values measured by the TTFM method and RPFM method. Simple linear regression was used to analyse the relationship between the TTFM method and RPFM method. A p value of less than 0.05 was considered significant. SPSS 10.0 software (SPSS Inc., Chicago, IL) was used for statistical analysis in this study.
3. Results
CABG could be safely performed in all cases. There were no operative deaths, perioperative myocardial infarctions, no need for an intra-aortic balloon pumping, and no cerebral infarctions. Also, no other major complications occurred postoperatively.
Flow values measured by the TTFM method and the RPFM method were compared and the result is listed in Table 1. In all target vessels, bypass flow measured with RPFM method was significantly higher than that measured with TTFM method.
Simple linear regression revealed no correlation between the TTFM measurement and the RPFM measurement (r = 0.08, p = 0.21) and the result is presented in the Figure 1.
In two patients, a bypass revision was indicated by TTFM measurement. These two cases are described more in detail:
Case 1. In a 59-years-old male patient with coronary 3-vessel disease and left main stem stenosis, CABG (LITA to the LAD and vein grafts to the Dx and the OM) was performed. After the completion of distal anastomosis to Dx, the value of the RPFM measurement was 50 ml/min, however, after the proximal anastomosis of this graft, the value of the TTFM measurement was close to zero (Figure 2(a)). According to this finding, the distal anastomosis to the Dx was revised and thereafter the value of the TTFM measurement became acceptable (Figure 2(b)). The postoperative course was uneventful.
Table 1. Flow measurement with TTFM and RPFM.
| TTFM | RPFM | p | |
| LAD (n = 4) | 48 ± 20 | 157 ± 52 | 0.01 |
| Dx (n = 23) | 42 ± 17 | 136 ± 42 | 0.01 |
| OM (n = 44) | 53 ± 21 | 146 ± 57 | 0.01 |
| RCA (n = 28) | 52 ± 28 | 170 ± 60 | 0.01 |
Dx: the diagonal artery, LAD: the left anterior descending artery, OM: the obtuse marginal artery, RCA: the right coronary artery.

Figure 1. Simple linear regression between the TTFM measurement and the RPFM measurement (r = 0.08, p = 0.21).
 (a)
(a)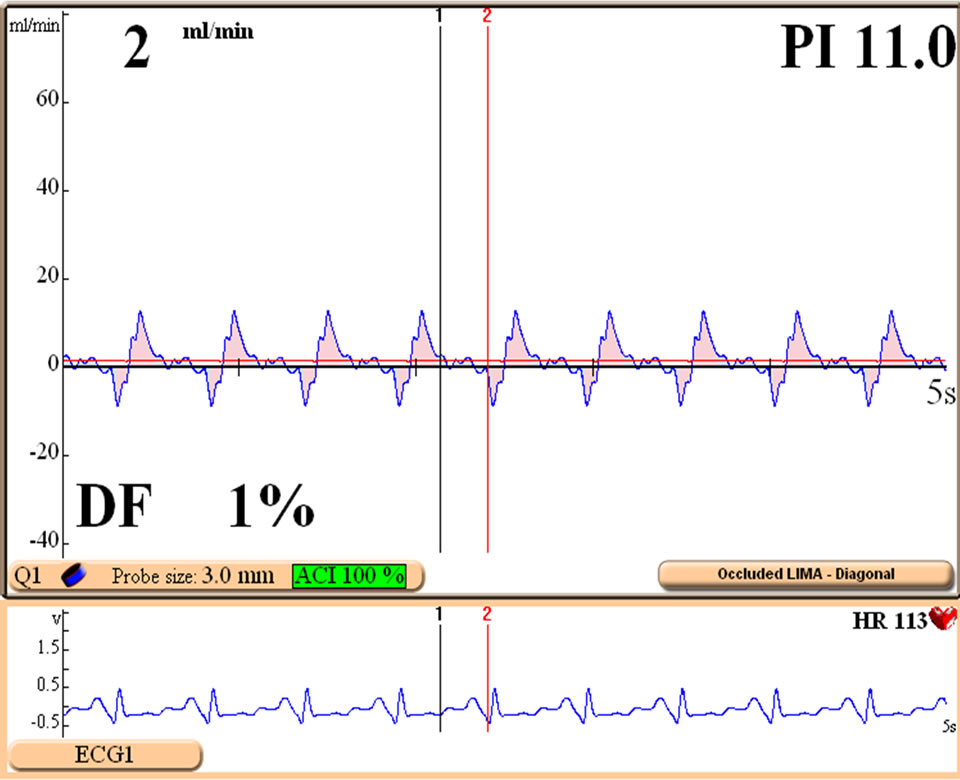 (b)
(b)
Figure 2. (a) TTFM measurement of the vein graft to Dx in the case 1; (b) TTFM measurement of the revised vein graft to Dx in the Case 1.
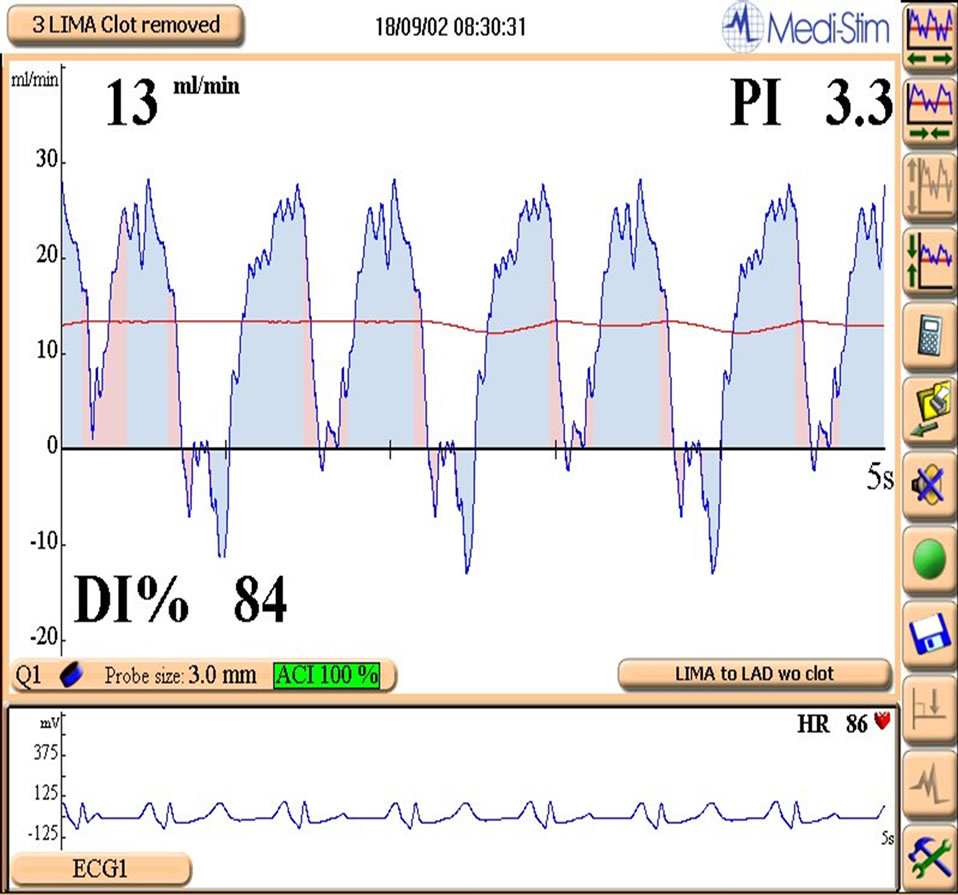
Figure 3. TTFM measurement of the LITA graft to the LAD in the Case 2.
Case 2. A 76-years old male with symptomatic left main stem stenosis exhibited progressive ST-segment elevation on the anterior wall after completion of all anastomoses (LIMA to the LAD and a vein graft to the OM). The TTFM measurement revealed non-functional LITA-graft (Figure 3). After completing an additional vein graft to the LAD, the electrocardiography was normalized. The further procedural and postoperative course was uneventful.
4. Discussion
To our best knowledge, in the year 1986 a report from our institute described for the first time the graft quality control in CABG [4]. Thereafter, the herein described method of RPFM was used for more than 20 years in our institute, however, meanwhile several modern techniques have been developed [3] and nowadays it is well accepted that the TTFM method is the method of choice for graft quality control with high levels of accuracy and convincing feasibility [1-3]. Therefore, both, the RPFM method and the TTFM method were evaluated in a direct comparison by this report. The crucial findings of the present study were 1) the RPFM method overestimated the graft flow in comparison to the TTFM method; 2) there was no correlation between the graft flow measured by TTFM method and those values measured by RPFM method; and 3) even in our small patient cohort, there were two cases in which a graft problem could be detected only with TTFM method. The present study suggests that the TTFM method is clearly superior to the traditional RPFM method and we believe now that TTFM should be performed routinely in all CABG to improve patient care and quality of surgical results.
REFERENCES
- J. J. Jokinen, K. Werkkala, T. Vainikka, T. Peräkylä, J. Simpanen and L. Ihlberg, “Clinical Value of Intra-Operative Transit-Time Flow Measurement for Coronary Artery Bypass Grafting: A Prospective Angiography-Controlled Study,” European Journal of Cardio-Thoracic Surgery, Vol. 39, No. 6, 2011, pp. 918-923. doi:10.1016/j.ejcts.2010.10.006
- H. B. Nordgaard, N. Vitale, R. Astudillo, A. Renzulli, P. Romundstad and R. Haaverstad, “Pulsatility Index Variations Using Two Different Transit-Time Flowmeters in Coronary Artery Bypass Surgery,” European Journal of Cardio-Thoracic Surgery, Vol. 37, No. 5, 2010, pp. 1063- 1067. doi:10.1016/j.ejcts.2009.11.030
- M. Leacche, J. M. Balaguer and J. G. Byrne, “Intraoperative Grafts Assessment,” Seminars in Thoracic and Cardiovascular Surgery, Vol. 21, No. 3, 2009, pp. 207-212. doi:10.1053/j.semtcvs.2009.08.007
- R. Körfer, G. Meurs, D. Seifert, K. Schmiel, P. Spiller and W. Bircks, “Reliability of Intraoperative Flow Measurements to Determine Early Graft Patency with Simultaneous Introduction of a New Method for Distal Coronary Artery Run-Off Capacity,” The Journal of Cardiovascular Surgery, Vol. 27, No. 1, 1986, pp. 79-84.

