Open Journal of Rheumatology and Autoimmune Diseases
Vol.2 No.3(2012), Article ID:21763,2 pages DOI:10.4236/ojra.2012.23008
Erdheim-Chester Disease with Right Atrial Tumor and “Temporal Arteritis”
![]()
1Department of Internal Medicine, Mayo Clinic College of Medicine, Rochester, USA; 2Department of Pathology, Mayo Clinic College of Medicine, Rochester, USA; 3Division of Rheumatology, Mayo Clinic College of Medicine, Rochester, USA.
Email: matteson.eric@mayo.edu
Received April 30th, 2012; revised June 4th, 2012; accepted June 27th, 2012
Keywords: Erdheim-Chester Disease; Temporal Arteritis; Giant Cell Arteritis
ABSTRACT
Erdheim-Chester disease is an unusual syndrome characterized by non-Langerhans cell histiocytosis which can mimic rheumatologic diseases. We report a case of Erdheim-Chester masquerading as giant cell arteritis, which was successfully managed with anakinra as anti IL-1 therapy.
1. Introduction
Erdheim-Chester disease is an unusual syndrome characterized by non-Langerhans cell histiocytosis. It is a systemic disorder with a plethora of symptoms and signs. We report for the first time a case of Erdheim-Chester disease with histologic evidence of temporal artery inflammation in a patient who had symptoms of giant cell arteritis.
2. Case Report
Evaluation of a 71-year-old man for three months severe headache, arrhythmia, dyspnea on exertion, fever, renal failure, and unintentional weight loss that were suspected to be due to giant cell arteritis. Initial C-reactive protein was markedly elevated at 192.7 mg/L (reference range < 8 mg/L). A temporal artery biopsy done at the referring facility revealed vasculitis without granuloma, and a diagnosis of temporal arteritis (giant cell arteritis) was made. Treatment with 60 mg prednisone a day was initiated with poor response.
Further detailed evaluation revealed an infiltrating right atrial mass on cardiac magnetic resonance imaging (Figure 1) and increased F-18 FDG uptake on PET/CT in the lung pleura, pericardium, and bone. Percutaneous biopsy of the right atrial lesion demonstrated a spindle cell histiocytic infiltrate that stained positive for CD68 and negative for CD1a, S100, desmin, CD34, SMA and CD117.
A diagnosis of Erdheim-Chester disease was made. Head magnetic resonance imaging (MRI) and cerebral spinal fluid analysis were unrevealing in evaluation of the persistent headache. Temporal artery biopsy was subsequently reviewed at our facility and demonstrated an adventitial infiltrate consisting primarily of CD68 reactive histiocytes consistent with Erdheim-Chester disease (brown staining; Figure 2).
There is no standardized treatment for Erdheim-Chester disease. Based on case reports and case series, interferon-alpha has been described as a first line treatment option [1]. This patient did not wish to proceed with interferon therapy due to concern about side effects and was instead treated with anakinra, an IL-1 antagonist that has been proposed as an alternate option for treatment of Erdheim-Chester disease [2]. With treatment, the patient experienced substantial improvement within 72 hours, including resolution of his headache. C-reactive protein was undetectable at <3 mg/dL after one week of treatment. The patient has remained asymptomatic on treatment during subsequent follow up of 3 months.
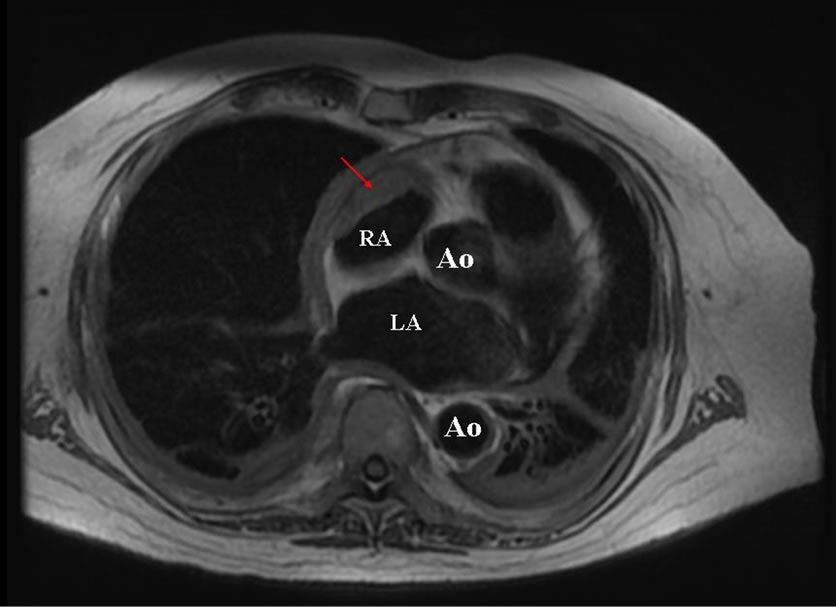
Figure 1. Magnetic resonance imaging with right atrial mass in Erdheim-Chester disease.
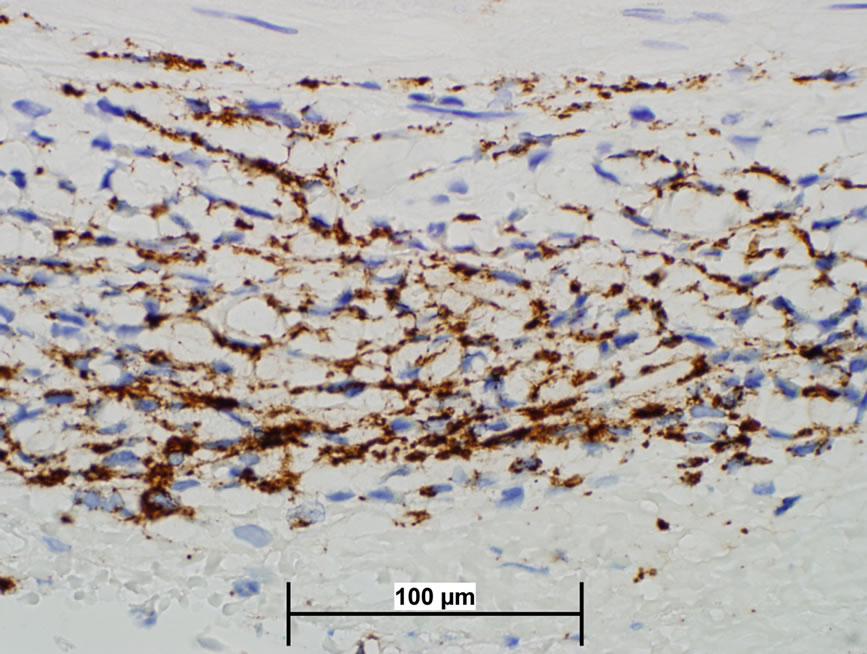
Figure 2. Temporal artery biopsy with CD68 staining consistent with Erdheim-Chester disease.
3. Discussion
First described in 1930, Erdheim-Chester disease is a rare non-Langerhans cell histiocytosis characterized by mononuclear cell infiltration of multiple organ systems [3]. Commonly reported sites of involvement include bone, heart, retroperitoneum/renal, and lungs/pleura [1]. Our patient presented with likely involvement of all of these systems. Right atrial tumor is one notable aspect of this case.
Cardiac complications of Erdheim-Chester disease are often under-recognized and carry a poor prognosis [4]. Right atrial tumor is a characteristic finding of ErdheimChester disease. One case series reported right atrial tumor in 30% of patients with cardiac involvement of Erdheim-Chester disease and right atrial infiltration in 49% of patients [4]. Indeed, Erdheim-Chester should be considered in the differential diagnosis of any patient with unexplained right atrial cardiac mass.
Bone involvement is among the most common presentations of Erdheim-Chester disease. The typical finding is of bilateral and symmetric sclerotic long bone lesions in the diaphysis associated with persistent pain [1]. Our patient did not have bone pain and skeletal X-ray survey was negative. However, his PET scan demonstrated bony metabolic abnormalities consistent with asymptomatic Erdheim-Chester involvement.
Temporal artery infiltration and inflammation caused by Erdheim-Chester disease is a novel aspect of this case that, to our knowledge, has not previously been reported. This patient presented with a severe headache associated with pathologically-proven inflammation of the temporal artery due to Erdheim-Chester disease infiltration. The patient’s headache resolved with anakinra treatment of his Erdheim-Chester disease. This patient’s temporal artery infiltrate did not have features suggestive of giant cell arteritis (classical temporal arteritis) but instead was an arterial inflammatory infiltrate due to Erdheim-Chester disease histiocytic infiltrate. A prior case report by Derrett-Smith and Dasgupta describes a patient with Erdheim-Chester disease mimicking giant cell arteritis; however, that patient’s symptoms were found to be due to a retro-orbital infiltrate and the temporal artery biopsy was negative for Erdheim-Chester disease involvement [5].
REFERENCES
- J. Haroche, L. Arnaud and Z. Amoura, “Erdheim-Chester Disease,” Current Opinion in Rheumatology, Vol. 14, No. 1, 2012, pp. 53-59. doi:10.1097/BOR.0b013e32834d861d
- A. Aouba, S. Georgin-Lavialle, C. Pagnoux, N. M. Silva, A. Renand, et al., “Rationale and Efficacy of Interleukin-1 Targeting in Erdheim-Chester Disease,” Blood, Vol. 116, No. 20, 2012, pp. 4070-4076. doi:10.1182/blood-2010-04-279240
- W. Chester, “Über Lipoidgranulomatose,” Virchows Archive, Vol. 279, No. 2, 1930, pp. 561-602. doi:10.1007/BF01942684
- J. Haroche, P. Cluzel, D. Toledano, G. Montalescot, D. Touitou, et al., “Cardiac Involvement in Erdheim-Chester Disease: Magnetic Resonance and Computed Tomographic Scan Imaging in a Monocentric Series of 37 Patients,” Circulation, Vol. 119, No. 25, 2009, pp. e597- e598. doi:10.1161/CIRCULATIONAHA.108.825075
- E. C. Derrett-Smith and B. Dasgupta, “Erdheim-Chester Disease: Yet another Mimic of Polymyalgia Rheumatica and Giant Cell Arteritis?” Rheumatology, Vol. 44, No. 3, 2005, pp. iii14-iii15.

