Open Journal of Orthopedics
Vol.4 No.2(2014), Article ID:42654,6 pages DOI:10.4236/ojo.2014.42004
Therapeutic Aspects of Chronic Bone Infections and Management Challenges
Department of Orthopaedic and Trauma Surgery, Aristide Le Dantec Teaching Hospital, Dakar, Sénégal.
Email: *cbdieme@yahoo.fr
Copyright © 2014 Charles Diémé et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Charles Diémé et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received November 12th, 2013; revised December 17th, 2013; accepted December 22nd, 2013
KEYWORDS
Chronic Bone Infection; Management; Challenges
ABSTRACT
This study aims to investigate various aspects of the treatment of chronic bone infections and the challenges in their management. The characterization of treatment of 73 patients with chronic bone infection was reported. The four management challenges including consultation delay, immune depression, extreme variety of clinical manifestations and non-use of CT or MRI were discussed in this study. We conducted a retrospective study at Aristide Le Dantec Hospital on 90 cases of chronic bone infection in 73 patients. The mean duration of symptoms before consultation was 36 months. More than half of the patients had a productive fistula at the first consultation. Sickle cell anemia was found in 6 patients. Multiple lesions were found in 10 patients; and long bones were affected in 90% of cases. The bacterial culture was positive in 93.15%. Staphylococcus aureus was the most isolated germ (68.35%). Seventy-two out of seventy-three patients were operated on. The procedure depended on anatomical and radiological lesions. Surgical treatment was associated with antibiotherapy which was firstly probabilistic and secondarily adapted to the results of bacterial culture. A favorable trend was found in 41 patients (56.16%). 32 cases of adverse effects were noted (43.83%), and 27 patients had recurrence after a favorable outcome. Several complications and sequelae were observed demonstrating the tenacity of these chronic infections.
1. Introduction
Osteomyelitis are a progressive infection of bone that results in inflammatory destruction, followed by new bone formation. Sometimes these are lifetime chronic diseases and continue to be a major public health problem in our country.
Treatment aims to master the evolution of the disease and allow patients to have a quality life compatible with a social and professional development. The extreme variety of clinical manifestations, local and systemic risk factors make patients management challenging. The therapeutic recommendations are, therefore, based on the findings of individual studies and on current textbooks [1]
The aim of our study was to report the aspects of treating chronic osteomyelitis and analyze their management challenges.
2. Materials and Methods
This is a retrospective study of 39 continuous months from January 2009 to March 2012. Were included patients older than 15 years treated for chronic osteomyelitis and whose files were complete and had a postoperative follow-up for more than 3 months. Thus, 73 of 89 patients hospitalized during this period were included representing 3.65% of hospitalizations. There were 36 cases of chronic osteomyelitis and 37 cases of chronic osteitis.
The average age was 28.8 years, ranging from 14 years to 83 years. There was a clear male predominance with a sex ratio of 4.26.
We had established a data collection form and gave it to each and every patient. It concerned reason and consultation period as well as the mode of contamination. Blood analysis included Emmel’s test, glycemia and retroviral serology.
Radiography of the concerned limb allowed us to classify radio-clinical forms. The surgical procedure depended on radiological variety and the need to cover.
An intra-operative sample with bacteriological and sensitivity analysis made it possible to isolate the organisms and test their sensitivity to antibiotics.
Antibiotherapy was continued until the normalization of monitoring parameters such as full blood count (FBC), C-reactive protein (CRP), erythrocyte sedimentation rate, and post operative control radiography.
The assessment was done according to our criteria. The criteria are the lack of pain and productive fistula, lack of sequestration and also a stable/normal X-ray image, normalization of previously raised biological parameters. Various complications were noted.
3. Results
The mean duration of symptoms before consulting our department was 36 months (6 months to 33 years). The fistula (56.6%) and pain (51%) were the main reasons for consultation. Other reasons for consultations are swelling (43.8%), chronic wounds (13.7%) and limping (11%).
Hematogeneous contamination was found in 49.3% of cases while the exogenous represented 50.7% of bone infections with 32.9% post-traumatic infection and 17, 8% postoperative infection. Sickle cell anemia was in 6 patients. The predilection of these infections was lower limb, femur and tibia constituting 58, 89% of affection (Table 1). The focus was unique in 63 patients and multiple in 10 patients.
Sequestration was found in 41 cases (figures 1-3), pathological fractures were noted in 3 cases and pandiaphyseal osteomyelitis in 12 cases. Anemia was found in 54.8% patients, leukocytosis in 35.6% and raise in CRP in 75.3% patients.
Pus analysis was positive in 68 cases equivalent to 93.15% and sterile in 5 cases making 6.84%. It was multiple infections in 10 cases equaling to 13.69%, of which 3 cases found in sickle cell anemia. Staphylo-coccus aureus was responsible for the infection in 58 cases, alone or combination with other germs (68.35%). Salmonella were isolated from four patients with sickle cell anemia disease and one case of Mycobacterium tuberculosis was found.
Seventy two of the seventy three patients were operated on. The procedure depended on anatomical and radiological lesions (Table 2). First step surgery, consist-

Table 1. Bones infection sites.
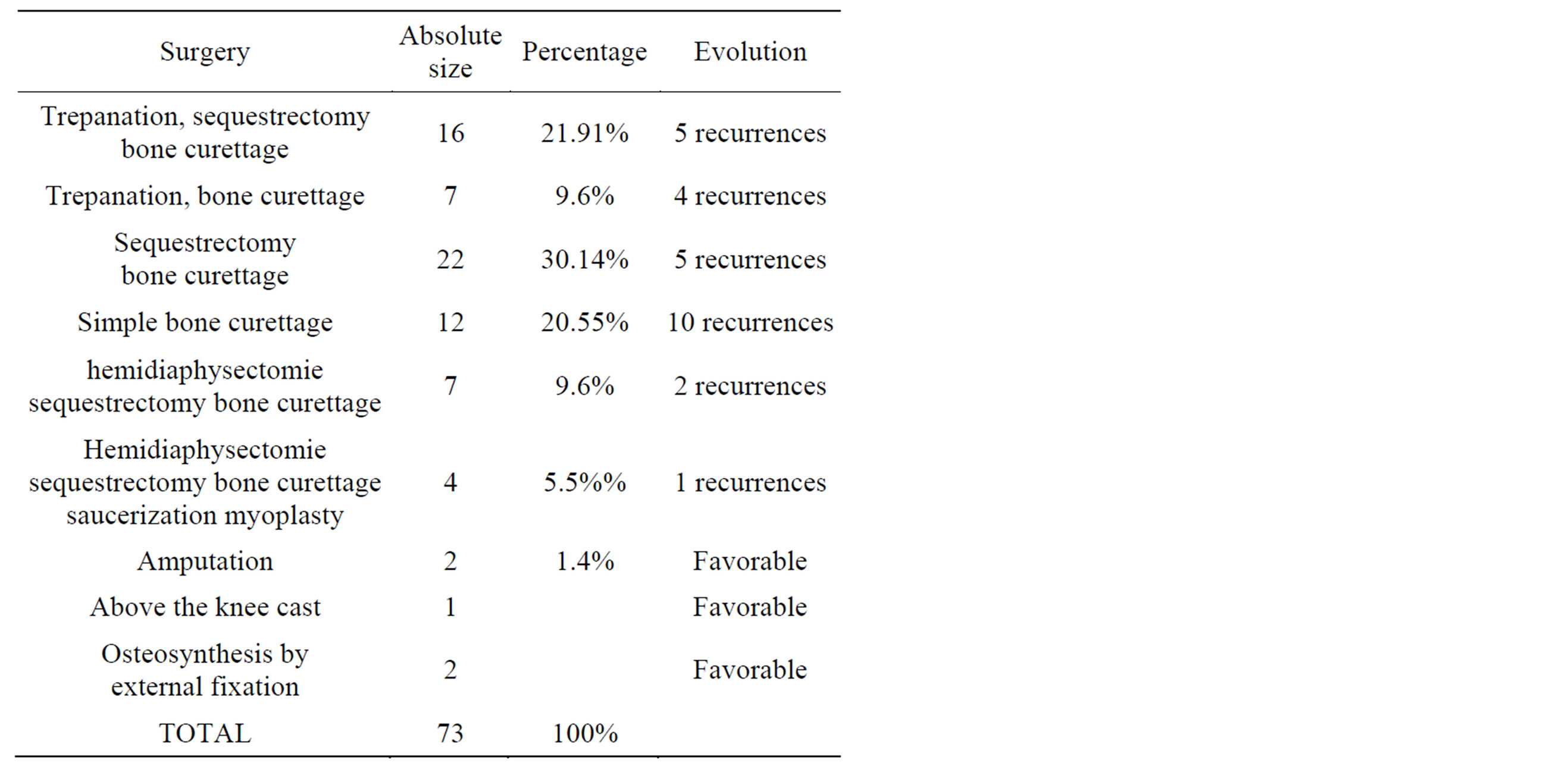
Table 2. Distribution according of the surgical treatment.
ing of excision and closure of the infection site was achieved in 93% of cases.
7% of patients underwent surgery in two stages consisting of first excision, wound left open, and then followed by a skin graft. Fistulectomy was performed in patients presenting with fistulized forms. Among the three fractures noted, two were treated with external fixation and another with above the knee cast.
Bone infections after surgical orthopaedic implantations were treated with implant removal followed by bone curettage. Surgical treatment was associated with medical treatment, first probabilistic and secondarily adapted to the antibiogram (Table 3). The bi-antibiotic

Figure 1. Chronic osteomyelitis of humerus with an important sequestrum.

Figure 2. Chronic osteomyelitis of tibia with an important sequestrum.

Figure 3. Post operative tibial ostemyelitis with removal of a huge sequestrum.
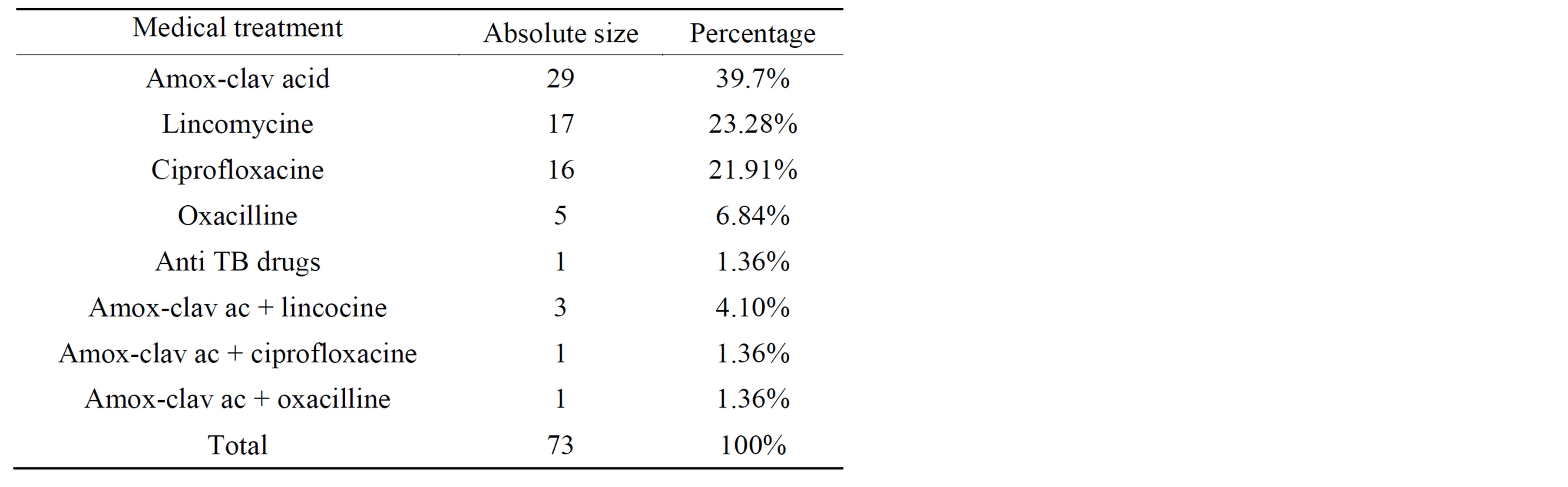
Table 3. Patients distribution based medical treatment received.
was used in 5 patients: 3 times amoxicillin-clavulanic acid and lincomycin, once ciprofloxacin amoxicillin and clavulanic acid and once oxacillin and amoxicillin-clavulanic acid. Patient that presented with clavicle tuberculosis osteomyelitis has been on TB treatment. Antibiotherapy was administered orally until achievement of stable biological monitoring parameters.
A favorable evolution was found in 41 patient’s equivalent to 56.16%. Adverse effects were noted in 32 cases (43.83%) with recurrence in 27 patients who had a favorable outcome.
Complications and sequelae were observed: limb discrepancy (Figure 4) 9 cases, deformation 11 cases, pathological fracture 3 cases, nonunion 2 cases, malignant degeneration of squamous cell carcinoma 1 case and death in a state of acute septicemia 3 cases.
4. Discussion
Three forms of osteomyelitis are defined upon pathogenic mechanisms of bone infections [2]:
• osteomyelitis secondary to a contiguous focus of infection after trauma, surgery(osteosynthesis or arthroplasty)
• osteomyelitis secondary to a contiguous focus of infection associated with vascular insufficiency (diabete).
• osteomyelitis following hematogenous spread of infection wich is the major mechanism in children.
In developing countries, chronic osteomyelitis is a continuing orthopaedic challenge and the hematogenous form is predominant (49.3% in our study). Various factors like, health service inaccessibility, inadequate treatment, malnutrition, poverty contribute to disease progression from acute osteomyelitis to chronic form. In industrialized countries post-traumatic and post-operative osteomyelitis is the most important form and around 10% to 30% of cases of bone infections become chronic [3].
Chronic osteomyelitis is secondary to delayed diagnosis or inadequate treatment of acute form. But it’s very difficult to define the time evolution of acute to the chro-

Figure 4. fistulised chronic femoral osteomyelitis with significant limb discrepancy.
nicity. However two facts characterize this form: necrotic bone and host reparative reactions [4].
In Africa, the first challenge in the management of these patients is the consultation delay as reported by many authors [5-13]. The average consultation time is 36 months for our patients. This delay is linked to beliefs that make patients first consult the traditional therapists. It is also linked to adverse socio-economic conditions for most of the patients and the disease ignorance.
The second challenge is the immunodepression often seen in these patients. The principle immunodepression found in the chronic bone infection was sickle cell anemia [10,11,14,15]. We found 6 cases of sickle cell anemia in our patients. Several mechanisms including hyposplenism, impaired complement activity and the presence of infracted or necrotic bone are increased susceptibility of sickle anemia patients to infections. HIV infection was also reported by Moyikoua [9]. These factors have a predisposing effect.
The extreme variety of clinical manifestations is the third challenge and makes it difficult treatment. The treatment of chronic osteomyelitis with antibiotics without surgical intervention is generally ineffective [16]. Antibiotics alone rarely can eradicate infection because of the avascular of scar tissue and necrotic bone.
Surgery must be guided by the pre-operative imaging such as radiography in our context. But sometimes CT and MRI are performed when planning a surgical intervention and for guiding surgery [17-19]. The non-use of CT or MRI is the fourth challenge in our study.
Cierny-Mader classification system was developed a guide for surgical management but is generally not used in primary care [20]. Surgery is generally conservative. The surgical procedure was performed in one step in 93% of our patients. It involves the removal of all sequestration and pus evacuation due to wide bone trephination and excision of fistula sinus. Medulary canal filling is carried out by bone graft, gentamycin cement or by myoplasty. Coverage muscle flaps are sometimes necessary. In the cases of infections after osteosynthesis, removal of implants is systematic. In situations of severe bone destruction, cancerous or sequelae (pathological fracture, limb shortening) additional procedures are necessary like external fixation, amputation, vascularized bone segments transferts [21].
Surgical treatment is always accompanied by first an empirical antibiotherapy secondarily adapted to the antibiogram. But empirical therapy is only necessary when it is not possible to isolate pathogens [22]. Antibiotics used must have good bone diffusion, be available and administered in an effective dose. Antibiotics such as penicillins, cephalosporins, clindamycin, fluoroquinolones, rifampin, vancomycin [23] are recognized to have a correct bone penetration. Intravenous administration of antibiotics permitted to optimize bioavailability. Some authors such as Massin [19] and Zeller [24] advocate for immediate orally antibiotics such as fluoroquinolones, rifampicin and fusidic acid for excellent bioavailability. The decision to use oral or parental antibiotics should be based on results regarding microorganism sensitivity, patient compliance, infectious disease and the surgeon’s experience. Bi antibiotherapy is recommended by some authors in the immediate postoperative [7,19,25]. For Delaere [23], monoantibiotherapy can be used immediately if debridement is correct. Bi antibiotherapy was used only in 5 of our patients. The duration of antibiotherapy varies according to many authors: 6 weeks Roger [25], 3 months Martini [26], 6 months to 1 year Massin [19]. We realize it until normal CRP in the absence of a hyperleucocytosis and sequestration on radiography.
Compared to other studies in Africa with different follow up duration, good result are variable (Table 4), but all authors found a high rate of recurrence. We noted 27 cases of recurrence after favorable outcome. These recurrences are often considered as patient’s failures and it
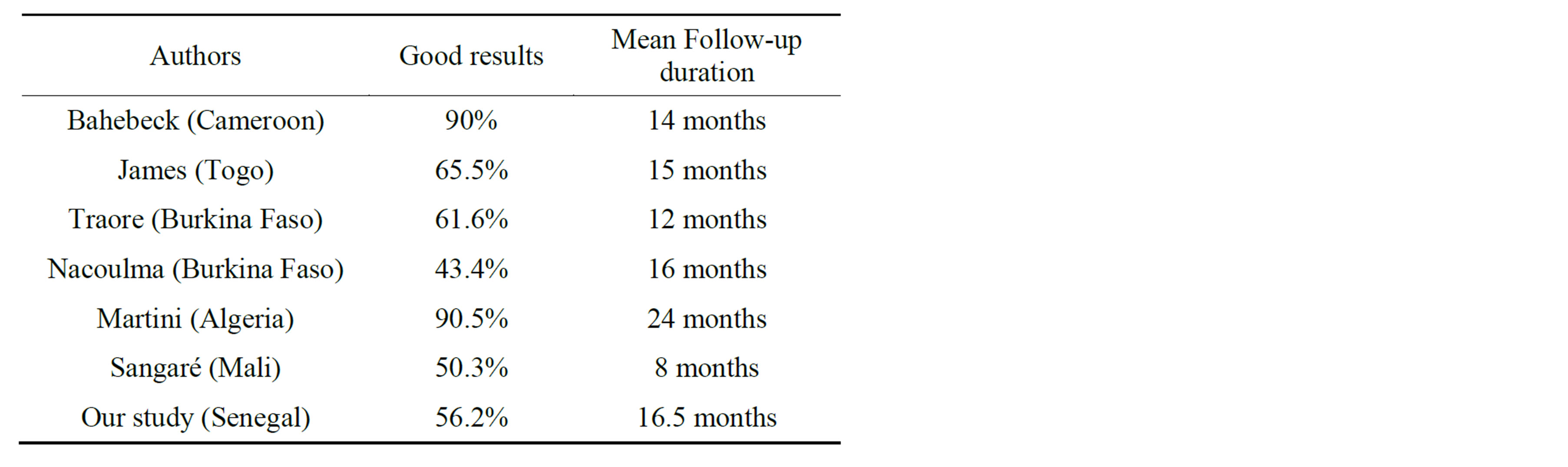
Table 4. comparison of results from various authors in Africa.
is not uncommon for these patients to return to the traditional healers for the treatment of this infection. It is the fifth challenge.
Complications are often reported in the literature. They are limb shortening deformation, limb amputation resulting in a major functional impairment. Malignant transformations are also reported. They occur after several years of evolution and are of squamous cell carcinoma type [14]. We had 3 cases of death. They are linked to acute septicemia [9].
According to Walter and al. [1], interdisciplinary treatment between orthopedic surgeons, plastic surgeons, radiologist, microbiologists, anesthesists, vascular surgeons and internal medicine specialists is essential for successful management of chronic osteomyelitis. It is our last challenge.
5. Conclusions
Chronic bone infection is still common in our African context. It is a lifetime chronic disease. Looking for immunodepression should be systematic. HIV infection and sickle cell anemia are the most predominant underlying conditions in our African context.
Improving the management of his chronic infections should through:
• Correct information about the disease to patients and its management challenges.
• Appropriate surgical procedure.
• Better cooperation between anesthetist, surgeon and Infectiologist.
REFERENCES
- G. Walter, M. Kemmerer, C. Kappler and R. Hoffmann, “Treatment Algorithms for Chronic Osteomyelitis,” Deutsches Ärzteblatt international, Vol. 109, No. 14, 2012, pp. 257-264.
- D. P. Lew and F. A. Waldvogel, “Osteomyelitis,” Lancet, Vol. 364, No. 9431, 2004, pp. 369-379. http://dx.doi.org/10.1016/S0140-6736(04)16727-5
- G. Hofmann, “Chronische Osteitis. Infektionen der Knochen und Gelenke,” Jena Urban & Fischer, Munchen, 2004, pp. 59-83.
- B. A. Lipsky and A. R. Berendt, “XVI Osteomyelitis,” American College of Physicians Medicine, 7 Inf Dis, XVI, 2010, pp. 1-20.
- J. Bahebeck, M. Ngowe, P. Mokom, O. J.-M. Bob, S. Moyo, M. Sosso and P. Hoffmeyer, “Le Traitement de l’Ostéomyélite Chronique Hématogène de l’Enfant. Ré- sultats Préliminaires d’une Série de 49 Patients à Yaoundé (Cameroun),” Médecine et Hygiène, Vol. 60, 2002, pp. 2381-2384.
- A. Habibou, Y. Salifou, H. Yacouba and L. Bazira, “Ostéomyélite Hématogène de l’Enfant et de l’Adolescent. A Propos de 126 cas. Niamey (Niger),” Médecine d’Afrique Noire, Vol. 46, No. 7, 1999, pp. 379-383.
- J. Y. Edem, A. Anani, W. Atchi, D. Assang and S. Badjona, “Les Infections Osseuses Chroniques de l’Adulte : Aspects Epidémiologiques et Thérapeutiques au CHU Tokoin de Lomé,” Journal de la Recherche Scientifique de l'Universite de Lome, Vol. 11, No. 1, 2009, pp. 101- 105.
- H. Martini, A. Daoud, A. Saïgui-Bouaouina, F. Ziani, F. Burni and M. Donkerwolcke, “Traitement Chirurgical des Ostéomyélites Hématogènes Chroniques: Une Série de 420 cas,” Revue de Chirurgie Orthopédique, Vol. 80, No. 7, 1994, pp. 642-650.
- A. Moyikoua, B. Pena-Pitra, J. M. Ondzoto and J. M. Kaya, “Ostéomyélites de l’Adulte à Propos de 25 cas,” Médecine d’Afrique Noire, Vol. 39, No. 11, 1992, pp. 749-750.
- S. I. Nacoulma, D.-D. Ouédraogo, E. W. Nacoulma, A. Korsaga and J. Y. Drabo, “Ostéomyélites Chroniques au CHU de Ouagadougou (B.F.): Étude Rétrospective de 102 cas (1996-2000),” Bulletin de la Société de Pathologie exotique, Vol. 100, No. 4, 2007, pp. 264-268.
- A. Sangaré, T. Alwata, S. Sidibé, M. Macalou and A. Touré, “Les Ostéites dans le Service d’Orthopédie et de Traumatologie de l’hôpital Gabriel Touré de Bamako,” Mali Médical, Vol. 23, No. 1, 2008, pp. 27-30.
- S. I. L. Seye, E. l. S. Camara, N. Bassene and I. Pouye, “Ostéomyélite Chronique au CHU Aristide-Le-Dantec à Dakar,” Bulletin de la Société de Pathologie Exotique, Vol. 87, 1994, pp. 238-240.
- O. Traoré, J. Yilboudo, G. Reyes, A. Rouamba and R. M. Ouiminga, “L’ostéomyélite Chronique: Aspects Cliniques et Thérapeutiques à Propos de 38 cas au Centre CHN de Bobo Dioulasso,” Médecine d’Afrique Noire, Vol. 44, No. 3, 1997, pp. 170-174.
- A. Bourchida, M. Rifi, H. Yacoubi, M. Mahfoud, El Bardouni, F. Ismail, M. S. Berrada, M. El Manouar and M. El Yacoubi, “La Dégénerecence Carcinomateuse sur Ostéomyélite Chronique,” Revue Marocaine de Chirurgie Orthopédique et Traumatologique, Vol. 35, 2008, pp. 24-26.
- B. Zelaere, “Les Ostéomyélites,” Louvain Médical, Vol. 119, 2000, pp. 525-530.
- J. Buchman and J. E. Blair, “The Surgical Management of Chronic Osteomyelitis by Saucerization, Primary Closure and Antibiotic Control,” The Journal of Bone & Joint Surgery, Vol. 33, No. 1, 1951, pp. 107-113.
- T. Gross, A. H. Kaim, P. Regazzoni and A. F. Widmer, “Current Concepts in Post-Traumatic Osteomyelitis: A Diagnostic Challenge with New Imaging options,” The Journal of Trauma, Vol. 52, No. 6, 2002, pp. 1210-1219.
- S. E. Selzer, “Value of Computed Tomo (CT) in Planning Medical and Surgical Treatment of Chronic osteomyelitis,” Journal of Computer Assisted Tomography, Vol. 8, No. 3, 1984, pp. 482-487.
- P. Massin, E. Legrand, P. Cronier, D. Chappard and M. Audran, “Diagnostic et Traitement des Ostéomyélites Chroniques de l’Adulte à Pyogène,” Revue du Rhumatisme, Vol. 73, No. 4, 2006, pp. 380-386. http://dx.doi.org/10.1016/j.rhum.2006.02.010
- G. Cierny 3rd, J. T. Mader and J. J. Penninck, “A Clinical Staging System for Adult Osteomyelitis,” Clinical Orthopaedics and Related Research, Vol. 414, 2003, pp. 7-24. http://dx.doi.org/10.1097/01.blo.0000088564.81746.62
- M. B. Wood and W. P. Cooney, “Vascularized Bone Segment Transferts for Management of Chronic Osteomyelitis,” Orthopedic Clinics of North America, Vol. 15, No. 3, 1984, pp. 461-472.
- E. Concia, N. Prandini, L. Massari, F. Ghisellini and F. Menichetti, “Osteomyelitis: Clinical up Date for Pratical Guidelines,” Nuclear Medicine Communications, Vol. 27, No. 8, 2006, pp. 645-660. http://dx.doi.org/10.1097/00006231-200608000-00007
- B. Delaere, “Les Ostéomyélites,” Louvain Médical, Vol. 119, 2000, pp. 525-530.
- E. Senneville, L. Legout, C. Loïez and H. Migaud, “Technique de Prescription des Antibiotiques en Chirurgie Orthopedique,” Encyclopédie Médico-Chirurgicale, 2008, pp. 44-88.
- P.-M. Roger, V. Lesbats, E. Cuaa, R. Farhad, C. Trojani, P. Boileau and P. Dellamonica, “Examens Paracliniques et Durée de l’Antibiothérapie des Infections Ostéoarticulaires,” Médecine et Maladies Infectieuses, Vol. 41, 2011, pp. 242-247. http://dx.doi.org/10.1016/j.medmal.2010.12.003
- H. Martini, F. Ziani and A. Adjrad, “L’association Amoxicilline/Acide Clavulinique Comme Antibiothérapie Complémentaire de la Chirurgie dans le Traitement des Osté- omyélites Hématogènes Chroniques,” Médecine et Maladies Infectieuses, Vol. 21, 1991, pp. 710-711. http://dx.doi.org/10.1016/S0399-077X(05)80238-0
NOTES
*Corresponding author.

