Open Journal of Orthopedics
Vol.3 No.2(2013), Article ID:32320,9 pages DOI:10.4236/ojo.2013.32011
Risk Assessments for Elderly Patients with Hip Arthroplasty Using POSSUM and P-POSSUM*
![]()
1Department of Orthopedic Surgery, First Affiliated Hospital of Dalian Medical University, Dalian, China; 2Department of Clinic Medicine, Dalian Medical University, Dalian, China; 3Medicose Health Net Inc., Richmond Hill, Canada; 4Health Policy and Management Department, School of Public Health, Peking University Health Science Center, Beijing, China; 5Department of Radiology, Dalian Central Hospital, Dalian, China.
Email: #yuancheng1999@163.com, dibhassan@hotmail.com, zhxiao_2004@yahoo.com.cn, xianliang_2004@yahoo.com.cn
Copyright © 2013 Yuancheng Li et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received April 2nd, 2013; revised May 9th, 2013; accepted May 21st, 2013
Keywords: Hip Arthroplasty; Mortality; Morbidity; P-POSSUM; POSSUM
ABSTRACT
Background: The physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM) is a scoring system previously validated in vascular and general surgical patients. The Portsmouth physiological and operative severity score for the enumeration of mortality and morbidity (P-POSSUM) is a reliable tool derived from POSSUM to improve the prediction of mortality. In this paper, we utilized both models to determine the most suitable and feasible one that could be utilized in orthopedic surgery in China mainland. Methods: In this retrospective study, patients’ files were extracted randomly from the medical records department of the First Hospital Affiliated with Dalian Medical University for those underwent hip replacements between 1999 and 2006. The mortality and morbidity rates were predicted by P-POSSUM and POSSUM, respectively. A comparative analysis was performed between the observed and the predicted values as well as the Observed/Expected ratio (O:E). Results: A total of 206 patients were selected for this study after fulfilling the inclusion and exclusion criteria. The predicted mortality by P-POSSUM were not significantly different from the observed values (X2 = 2.10, P = 0.552). POSSUM appeared to be better with the observed morbidity (X2 = 2.766, P = 0.598), but had overestimated mortality. Conclusion: The POSSUM morbidity equation satisfactorily estimated the risk of postoperative complications, and the P-POSSUM mortality equation appeared to stratify the risk of death more accurate than the POSSUM.
1. Introduction
With the advent of China’s aging society, there is an increasing trend of femoral neck fractures. So far, treatments for these types of fractures are either through operative or non-operative procedures (traction, abduction and so on). Early postoperative ambulation in elderly patients with femoral neck fractures prevents patients from developing complications (deep venous thrombosis, urinary tract infection, hypostatic pneumonia and so on) caused by long-term immobilization and improves the quality of life. However, it is very hard to obtain a stable fixation treatment among elderly patients by either abduction or traction. Unstable fractures in non-operative patients such as in osteoporosis or with poor general conditions might take longer time for the healing process and expose patients to a series of complications. In some researches [1-6], the rate of mortality within half a year can range from 30% to 50%. However, other studies had illustrated that elderly patients with early hip replacement can have a better prognosis than the non-operative patients, and would be less exposed to long term immobilization [7].
In China mainland, in addition to the financial factor, the operative risk factors for hip replacement among patients with chronic diseases such as diabetes, hypertension, congestive heart failure (CHF) or arrhythmias would place the surgeon, the patient and patients’ caregivers in a dilemma. At present, some surgeons [8-11] had adopted the non-operative treatment to reduce the peri-operative risks even when patients have indications for arthroplasty (GARDEN III or GARDEN IV(a) in femoral neck fractures). Over the past years, surgeons in China have always found it confusing to assess the postoperative risks (morbidity and mortality) for arthroplasty among elderly patients due to the absence of specific guidelines that is needed to be adopted in their assessment.
Therefore, we have found it necessary to provide better evidence-base guidelines in this field. This is done by comparing the predicted and observed morbidity and mortality in 206 randomly selected patients that received hip arthroplasty after being subjected to total hip or partial hip replacements.
Progression of POSSUM to P-POSSUM: In 1991, Copeland(b) and his colleagues developed the physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM) to provide a possible tool for risk adjustment as well as a comparative auditing system for different surgeons, units, hospitals and regions. The initial researchers examined 62 influencing factors on morbidity and mortality which were later reduced to just 12 physiological and 6 operative parameters (Appendix 1, Tables A1 and A2). Using the recorded parameters, the system was able to determine a physiological score and an operative severity score from which the expected mortality and morbidity rates was calculated and marked as R1 and R2 (where R1 = mortality and R2 = morbidity) by utilizing logistic regression equations. After 6 months of clinical observation, Copeland and his colleagues approved the accuracy of the formula by predicting the mortality and complications after surgery [12]. In 1996, Whiteley et al. [13] enrolled 1485 patients in Portsmouth, UK and used the POSSUM method. They found that POSSUM had overestimated the risk of death especially in low risk patients. They used the same physiological and operative scores, but modified the calculations and suggested a modified formula that fitted better their data. This has become known as the Portsmouth physiological and operative severity score for the enumeration of mortality and morbidity (PPOSSUM).
2. Methods and Materials
In this retrospective study, 260 patients were hospitalized between 1999 and 2006 for femoral neck fractures— either with GARDEN III or GARDEN IV criteria(a)—at the First Hospital Affiliated with Dalian Medical University. Patients’ records were randomly extracted from the orthopedic medical records. Information on age, sex, nature of falling and the locus of the fracture, origin of residence (inside or outside the city), clinical history, pre-operative studies and drug treatments were all collected and recorded. From the 260 patients records that were randomly selected 118 (45.38%) females and 88 (33.85%) males were considered. Around 54 (20.77%) patients were excluded from the study because of incompleteness in their medical data or didn’t fit our inclusion criteria. The total patients that undergone total hip replacements reached to 154 (74.76%), and 52 (25.24%) patients had partial hip replacement. A total of 19 (9.22%) were between 55 - 60 years old, 77 (37.38%) patients were between 61 - 70 years old, and 110 (53.40%) were above 71 years old (Table 1).
2.1. Inclusion Criteria
1) Females’ age ≥ 55 years and males’ age ≥ 60 years for those with femoral neck fractures (GARDEN III or GARDEN IV) were considered, (the variation in the age selection is because of the osteoporosis factor among women);
2) Patients that underwent either partial or total hip replacement;
3) Patients with chronic medical history such as diabetes, congestive heart failure, multiple arrhythmias but under control;
4) Patients operated on within 72 hours.
2.2. Exclusion Criteria
1) Patients without fully peri-operative data were excluded from the study;
2) Patients with hip fractures related to pathological causes such as bone tumors (primary and secondary tumors), hypoparathyroidism, idiopathic hypoparathyroidism, Paget’s diseases, and other genetic malformation of bone, metastatic disease, etc.
This study was approved by the Ethics Committee of First Affiliated Hospital of Dalian Medical University, Department of Orthopedic Surgery.
Our patients were in uniformity in terms of preoperative and postoperative treatment, which is the standard for all patients undergoing hip replacements in our hospital (see Appendix 2). The POSSUM and P-POSSUM scores were calculated 24 h preceding the operations according to the dichotomous scales. The sum scores were calculated manually by one of the researchers, and stored in a Microsoft Access Database. We defined the operative complexity according to the features of the orthopedic surgeries [14] (Appendix 3, Table A3). All physiological scores were recorded when performed within 24 hours preceding the operations. Also, data about postoperative complications and deaths within 30 days were gathered. Two of our team members kept in contact with patients directly or through family members (for those who were hospitalized less than 30 days) either through telephone discussions or through the Outpatient Department (OPD) to check out for any complications and mortalities that occurred after the discharge phase. Post-operative complications [15] included: 1) severe hemorrhage; 2) infection from deep wound, urinary tract
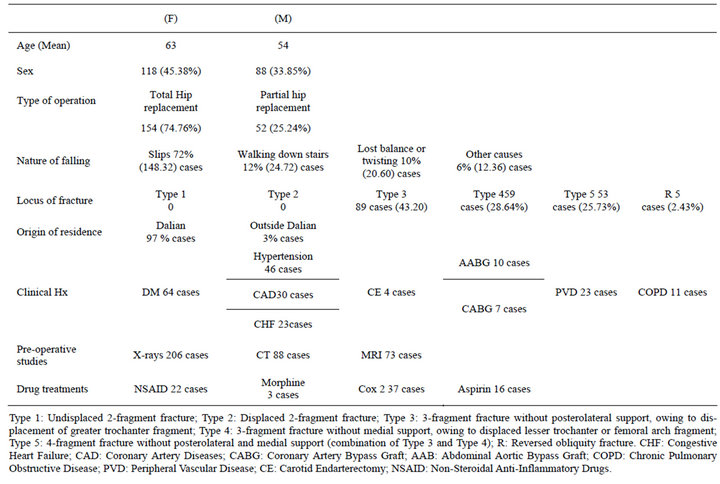
Table 1. Patients’ demographic data.
septicemia and pyrexia of unknown origin; 3) wound dehiscence, or loose/displaced prosthesis; 4) thrombosis/ deep venous thrombosis, pulmonary embolism, cerebrovascular accident and myocardial infarction; 5) renal failure, respiratory failure, cardiac failure and hypotension; 6) others (Table 2). Patients’ predicted mortality and morbidity risk was calculated using the respective equations obtained from the research performed by Copeland(b) and Prytherch [16]:
POSSUM equation for mortality rate (R1)
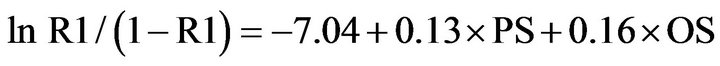 (1)
(1)
POSSUM equation for complication rate (R2)
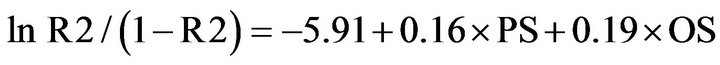 (2)
(2)
P-POSSUM equation for mortality rate (R3)
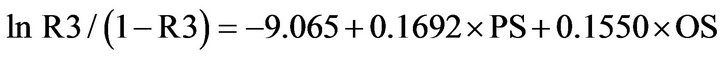 (3)
(3)
Where PS indicates physiological score; OS indicates operative score. A linear analysis was performed [17] where the predicted mean risk for patients in each risk group was calculated and multiplied by the number of patients within the group to provide patients’ predicted mortality. The predicted mortality rates were compared with the observed rates (O:E); thus, determining the accuracy of the prediction. Then we divided the admissions into: 1) fatal group; 2) non-fatal group; 3) patients with complications; and 4) patients without complications, (Tables 3-5). The observed and predicted numbers within each group were calculated and compared using a chisquared statistic. P value <0.05 was regarded to be significant. Statistical analyses were performed using SPSS for Windows version 14.0 professional (SPSS® Inc., Chicago, Illinois).
3. Results
Patients with femoral neck fractures were classified according to Garden criteria(a): The most common type in our study was Garden III femoral neck fracture (n = 89; 43.20%), followed by Garden IV (n = 59; 28.64 %) (Table 1). The mean operative time was 1: 25 hours, (SD: 1.42 ± 0.22). The mean hospital stay was 14.32 days (SD: 14.32 ± 2.45). The preoperative physiological scores were lowered for high-risk patients. As for the predicted mortality, it was lowered dramatically from 9.7% to 1.9% after adjustments (Table 6). Furthermore, for the predicted complications, the rate was lowered from around 42% to 30% after adjustment (Table 6).
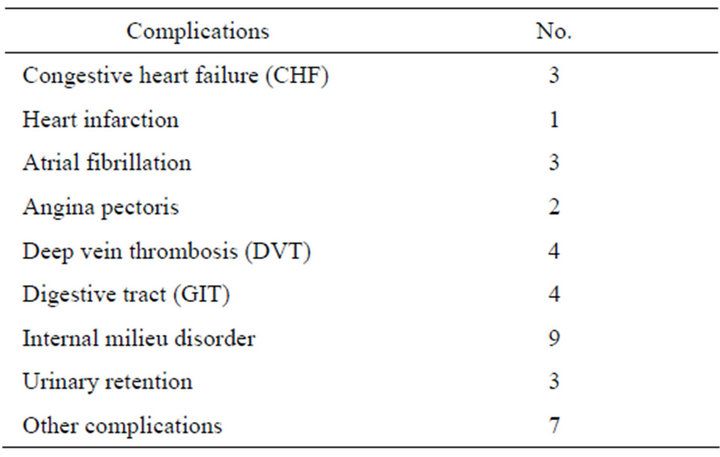
Table 2. Observed complications.
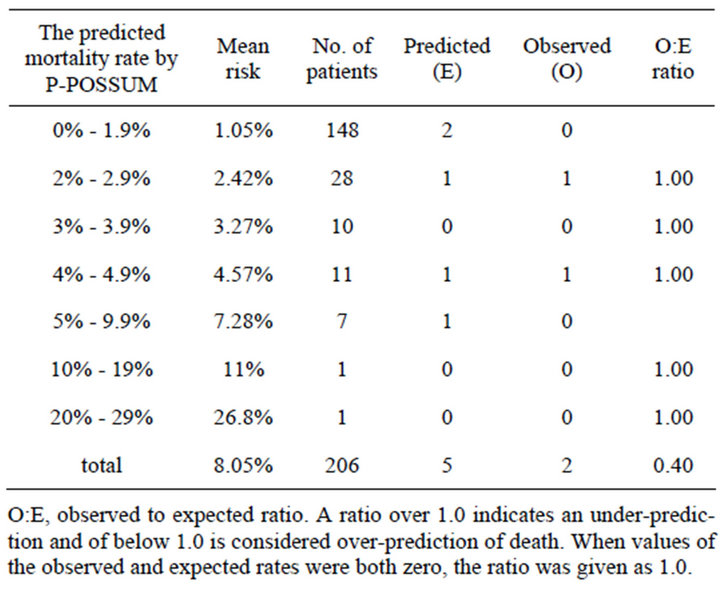
Table 3. “Linear” analysis of deaths predicted by P-POSSUM predictor equation for mortality.
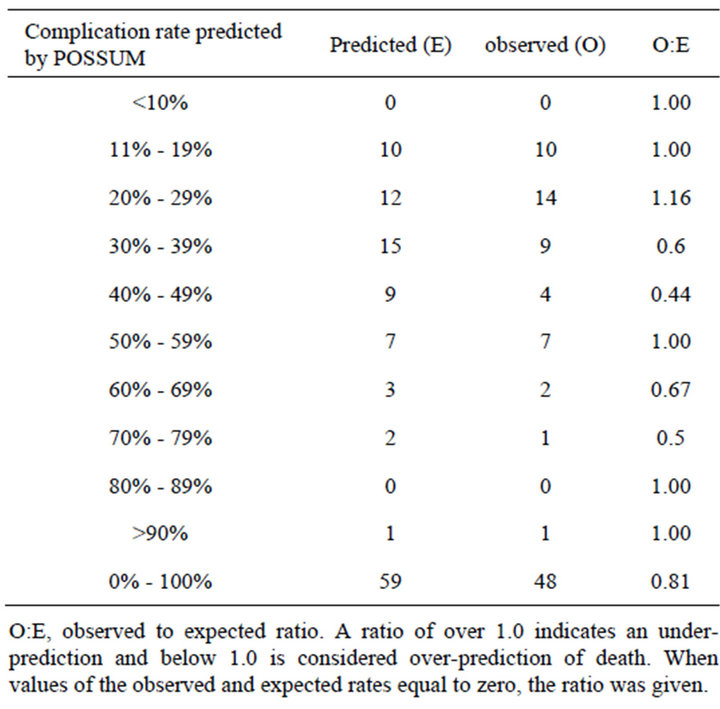
Table 4. “Linear” analysis of morbidity predicted by POS- SUM.
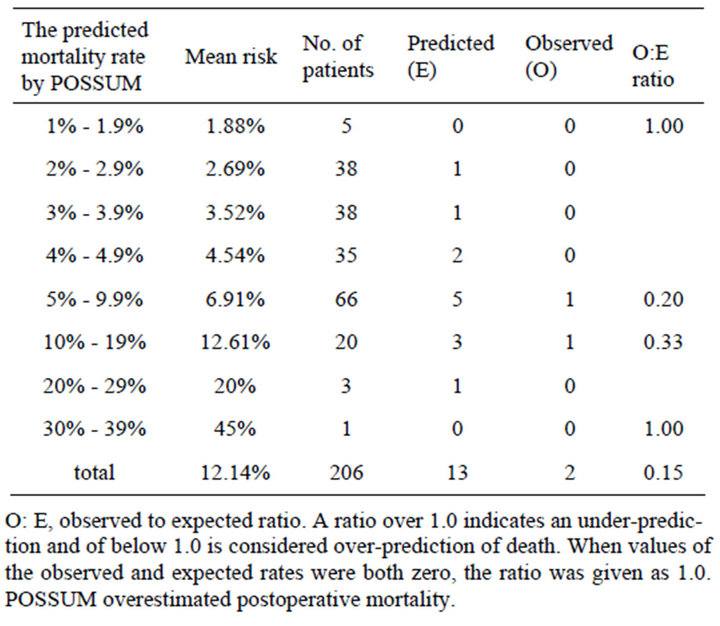
Table 5. Linear analysis of deaths predicted by POSSUM.
A total of 9 serious postoperative complications were recorded from 36 patients. The main complications were Atrial Fibrillation (AF), Deep Venous Thrombosis (DVT), Congestive Heart Failure, internal milieu disorders (water and electrolytes imbalances) and Gastrointestinal Tract (GIT) diseases as shown in as shown in Table 3; and 2 deaths had occurred in-hospital stay.
As for the predicted mortality by P-POSSUM they were not significantly different from the observed values (X2 = 2.10, P = 0.552; the overall O: E ratio is 0.4, Table 3). The POSSUM appeared to fit well with the observed morbidity (X2 = 2.766, P = 0.598; the overall O:E ratio is 0.81, Table 4), but had an overestimated mortality, the overall O:E ratio was 0.15 (Table 5).
4. Discussion
The majority of patients in this study were old aged patients. This group had a higher tendency for sudden falls resulting in rapid hip fractures. This is due to bone fragility due to insufficient intake of protective and preventive medications-osteoporosis disease-against multiple bones fractures. Hence, we evaluated morbidity and mortality among this age group by implementing two scoring systems POSSUM and P-POSSUM in order to calculate the predicted mortality and morbidity. POSSUM and PPOSSUM were developed in the British medical setting and over 200,000 patients have been scored through these systems [18]. Since that time, these two scoring systems have been implemented in general surgery, vascular surgery, surgical gastroenterology, urology, surgical ICU patients, orthopedic surgery, and are used by many health-care organizations [19-22]. However, there are very limited data about using these two scoring systems in orthopedic surgery. Our study showed that the lowest mortality rate in the predicted mortality group by POS-
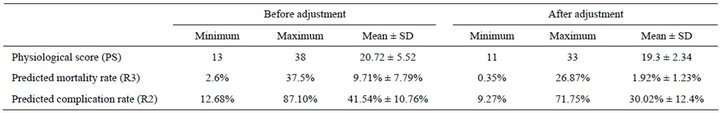
Table 6. Adjustment of the preoperative parameters.
SUM was 1.73% (12 points in the physiological score, 9 in the operative severity), which was evidently higher than the observed. On the other hand, the lowest mortality in the predicted mortality group showed 0.34% by P-POSSUM. We concluded that P-POSSUM could reflect the observed mortality rate more closely than POSSUM in hip arthroplasty among elderly patients with femoral neck fractures, but tended to overestimate the mortality rate in low-risk patients 0% - 1.9%.
Our study showed that, and according to P-POSSUM, the predicted mortality was low, while POSSUM provided overestimation in the predicted mortality, which fitted well with the observed complications compared with similar observations in Ramanathan et al. [23] and Wang et al. [24]; however, they have advised that it should be used with caution whether as an auditing tool or for preoperative triage. Also, as an auditing tool for femoral neck fractures, Wright et al. [25] study concluded that POSSUM can accurately predict mortality and morbidity in patients with femoral fractures. Also, Gu et al. [26] showed that a perfect agreement was found between the observed number of deaths and the predicted number of deaths calculated by P-POSSUM, while POSSUM overestimated the overall mortality-similar to our study. As for the study done by Tekkis et al. [27] proposed that there was a goodness of fit between the overall observed morbidity and mortality and the prediction by POSSUM and P-POSSUM, while overestimation occurred among the elective surgery and the young group (opposite to our old aged patients). Hence, it is important to be discreet while introducing these systems for the low-risk surgeries. While Mohamed and Copeland [14] proved a close correlation between the overall observed rates for mortality and morbidity and the predicted values—derived only from the POSSUM logistic regression equation—in the orthopedic surgery and avoided performing any comparisons between POSSUM and P-POSSUM, which is the opposite to our comparisons.
The differential differences in the observed results between studies may have occurred for several reasons. First, the medical background, such as the medical system, hospital facilities sanitation, peri-operative nursing care, and staff efficiency all are different whether domestically or when compared from one country to another. Second, in some studies the conditions differed such as patient’s physiological immunity, ability to tolerate duration of operation, operation method, peri-operative treatment, and so on. Third, the parameters’ scores such as estimated blood loss, respiratory and cardiovascular history are prone to errors and might be due to different measurement systems.
In the last couple of years, another method was used where researchers applied Estimation of Physiologic Ability and Surgical Stress (E-PASS) risk-scoring system for predicted and actual morbidity and mortality rates to assess the predictive ability of the E-PASS and compared it with the physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM) systems in patients with hip fractures. They showed that E-PASS scoring system is useful for defining postoperative risk, and its underlying algorithm can accurately predict morbidity and mortality rates in patients with hip fractures before surgery, which can be utilized to manage their condition and potentially improve treatment outcomes [28].
4.1. Recommended Policy Assessment
No regression equation for risk assessment should remain indefinitely static [14]. In the past decade we have found there was no need for any change in the equation, but in the coming future changes should occur where the equation could be easily updated without the need to alter the variables scores. Consequently, both of these systems should be updated in steps to match up with the rapid developments in modern medicine.
4.2. Study Limitations
Due to the structuring of this research paper, we were not able to gather all further information about patients’ mortality and morbidity once they were discharged. Then, the discriminatory power and predictive value of each scoring system was not evaluated using receiver operator characteristic (ROC) curve analysis, which might have provided more accurate results. Nevertheless, we were able to show that POSSUM overestimation of mortality which had fitted morbidity, and P-POSSUM provided low estimation of mortality.
In conclusion, the POSSUM morbidity equation had satisfactorily estimated the risk of postoperative complications, and the P-POSSUM mortality equation appeared to stratify much accurately the risk of death than POSSUM. They are good measurable tools to detect the expected morbidity and mortality for patients undergoing hip arthroplasty in China mainland.
4.3. Footnotes
1) Garden Criteria Grade I is an incomplete or valgus impacted fracture.
Grade II is a complete fracture without bone displacement.
Grade III is a complete fracture with partial displacement of the fracture fragments.
Grade IV is a complete fracture with a total displacement of the fracture fragments.
Garden R (1961) Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br 43:647-661.
2) Copland Derivation of POSSUM and P-POSSUM Formulas POSSUM scoring system was first conceived and successfully implemented by G. P. Copland et al. Driven by the need to develop a simple risk scoring system applicable to diverse general surgical populations, whose main use would be in surgical audit, POSSUM scoring system was developed. First published article of POSSUM had appeared in British Journal of Surgery March 1991; 78: 356-360. Copland et al. conducted a prospective study over a period of six months in 1372 patients undergoing operation in general surgery units. POSSUM scoring system produced an assessment of morbidity and mortality rates which did not significantly differ from observed rates. They concluded that although POSSUM may not be able to replace highly specific scoring systems for individual disease states or the intensive care patient, it does appear to provide an efficient indicator of the risk of morbidity and mortality in the general surgical patient. Authors also stressed the usefulness of POSSUM as an adjunct to surgical audit.
An article by Whitely et al. in 1996 showed how the original POSSUM regression equation failed to work in patients in Portsmouth. The authors found that POSSUM over-predicted death in a cohort of 1485 patients, particularly those at low risk. It was still possible to use the POSSUM physiology and operative severity data set, but a different regression equation was needed. This regression equation became the Portsmouth predictor equation, or P-POSSUM.
REFERENCES
- M. Martinez-Reig, L. Ahmad and G. Duque, “The OrthoGeriatrics Model of Care: Systematic Review of Predictors of Institutionalization and Mortality in Post-Hip Fracture Patients and Evidence for Interventions,” Journal of the American Medical Directors Association, Vol. 13, No. 9, 2012, pp. 770-777. doi:10.1016/j.jamda.2012.07.011
- A. Agustí, E. Pagès, A. Cuxart, E. Ballarín, X. Vidal, J. Teixidor, J. Tomás, M. M. Villar and J. R. Laporte, “Exposure to Medicines among Patients Admitted for Hip Fracture and the Case-Fatality Rate at 1 Year: A Longitudinal Study,” European Journal of Clinical Pharmacology, Vol. 68, No. 11, 2012, pp. 1525-1531. doi:10.1007/s00228-012-1273-y
- S. A. Frost, N. D. Nguyen, D. A. Black, J. A. Eisman and T. V. Nguyen, “Risk Factors for In-Hospital Post-Hip Fracture Mortality,” Bone, Vol. 49, No. 3, 2011, pp. 553- 558. doi:10.1016/j.bone.2011.06.002
- P. N. Kannegaard, S. van der Mark, P. Eiken and B. Abrahamsen, “Excess Mortality in Men Compared with Women Following a Hip Fracture,” National Analysis of Comedications, Comorbidity and Survival, Age Ageing, Vol. 39, No. 2, 2010 pp. 203-209. doi:10.1093/ageing/afp221
- B. Abrahamsen, T. van Staa, R. Ariely, M. Olson and C. Cooper, “Excess Mortality Following Hip Fracture: A Systematic Epidemiological Review,” Osteoporosis International, Vol. 20, No. 10, 2009, pp. 1633-1650. doi:10.1007/s00198-009-0920-3
- P. N. Streubel, W. M. Ricci, A. Wong and M. J. Gardner, “Mortality after Distal Femur Fractures in Elderly Patients,” Clinical Orthopaedics and Related Research, Vol. 469, No. 4, 2011, pp. 1188-1196. doi:10.1007/s11999-010-1530-2
- E. W. Evans, “Trochanteric Fractures: A Review of 110 Cases Treated by Nail-Plate Fixation,” The Journal of Bone and Joint Surgery, Vol. 3, No 33, 1951, pp. 192- 204.
- L. H. Ooi, T. H. Wong, C. L. Toh and H. P. Wong, “Hip Fractures in Nonagenarians—A Study on Operative and Non-Operative Management,” Injury, Vol. 36, No. 1, 2005, pp. 142-147. doi:10.1016/j.injury.2004.05.030
- J. J. Gregory, K. Kostakopoulou, W. P. Cool and D. J. Ford, “One-Year Outcome for Elderly Patients with Displaced Intracapsular Fractures of the Femoral Neck Managed Non-Operatively,” Injury, Vol. 41, No. 12, 2010, pp. 1273-1276. doi:10.1016/j.injury.2010.06.009
- M. Hossain, V. Neelapala and J. G. Andrew, “Results of Non-Operative Treatment Following Hip Fracture Compared to Surgical Intervention,” Injury, Vol. 40, No. 4, 2009, pp. 418-421. doi:10.1016/j.injury.2008.10.001
- A. A. Faraj, “Non-Operative Treatment of Elderly Patients with Femoral Neck Fracture,” Acta Orthopaedica Belgica, Vol. 74, No. 5, 2008, pp. 627-629.
- G. P. Copeland, D. Jones and M. Walters, “POSSUM: A Scoring System for Surgical Audit,” The British journal of Surgery, Vol. 78, No. 3, 1991, pp. 335-360. doi:10.1002/bjs.1800780327
- M. S. Whiteley, D. R. Prytherch, B. Higgins, P. C. Weaver and W. G. Prout, “An Evaluation of the POSSUM Surgical Scoring System,” The British Journal of Surgery, Vol. 83, No. 6, 1996, pp. 812-815. doi:10.1002/bjs.1800830628
- K. Mohamed and G. P. Copeland, “An Assessment of the POSSUM System in Orthopaedic Surgery,” The Journal of Bone and Joint Surgery, Vol. 84, No. 5, 2002, pp. 735-799. doi:10.1302/0301-620X.84B5.12626
- P. G. Copeland, “The POSSUM System of Surgical Audit,” Archives of Surgery, Vol. 137, No. 1, 2002, pp. 15-19. doi:10.1001/archsurg.137.1.15
- D. Prytherch, M. S. Whiteley, B. Higgins, P. C. Weaver, W. G. Prout and S. J. Powell, “POSSUM and Portsmouth POSSUM for Predicting Mortality: Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity,” The British Journal of Surgery, Vol. 85, No. 9, 1998, pp. 1217-1220. doi:10.1046/j.1365-2168.1998.00840.x
- L. D. Wijesinghe, T. Mahmood, D. J. Scott, D. C. Berridge, P. J. Kent and R. C. Kester, “Comparison of POSSUM and the Portsmouth Predictor Equation for Predicting Death Following Vascular Surgery,” The British Journal of Surgery, Vol. 85, No. 2, 1998, pp. 209-212. doi:10.1046/j.1365-2168.1998.00709.x
- E. Bennett-Guerrero, J. A. Hyam, S. Shaefi, D. R. Prytherch, G. L. Sutton, P. C. Weaver, M. G. Mythen, M. P. Grocott and M. K. Parides, “Comparison of P-POSSUM Risk-Adjusted Mortality Rates after Surgery between Patients in the USA and the UK,” The British Journal of Surgery, Vol. 90, No. 12, 2003, pp. 1593-1598. doi:10.1002/bjs.4347
- A. Brunelli, A. Fianchini, F. Xiume, R. Gesuita, A. Mattei and F. Carle, “Evaluation of the POSSUM Scoring System in Lung Surgery: Physiological and Operative Severity Score for the Enumeration of Mortality and Morbility,” The Thoracic and Cardiovascular Surgeon, Vol. 46, No. 3, 1998, pp. 141-146. doi:10.1055/s-2007-1010211
- N. Gotohda, H. Iwagaki, S. Itano, S. Horiki, T. Fujiwara, S. Saito, A. Hizuta, H. Isozaki, N. Takakura, N. Terada and N. Tanaka, “Can POSSUM, a Scoring System for Perioperative Surgical Risk, Predict Postoperative Clinical Course?” Acta Medica Okayama, Vol. 52, No. 6, 1998, pp. 325-329.
- P. P. Tekkis, H. M. Kocher, A. J. Bentley, P. T. Cullen, L. M. South, G. A. Trotter and J. P. Ellul, “Operative Mortality Rates among Surgeon: Comparison of POSSUM and P-POSSUM Scoring Systems in Gastrointestinal Surgery,” Diseases of the Colon and Rectum, Vol. 43, No. 11, 2000, pp. 1528-1532. doi:10.1007/BF02236732
- N. Ogan, T. Morgan, B. Venkatesh and D. Purdie, “Evaluation of the P-POSSUM Mortality Prediction Algorithm in Australian Surgical Intensive Care Unit Patients,” Australian and New Zealand Journal of Surgery, Vol. 72, No. 10, 2002, pp. 735-738. doi:10.1046/j.1445-2197.2002.02528.x
- T. S. Ramanathan, I. K. Moppett, R. Wenn and C. G. Moran, “POSSUM Scoring for Patients with Fractured Neck of Femur,” British Journal of Anaesthesia, Vol. 94, No. 4, 2005, pp. 430-433. doi:10.1093/bja/aei064
- T. J. Wang, B. H. Zhang and G. S. Gu, ”Evaluation of POSSUM Scoring System in the Treatment of Osteoporotic Fracture of the Hip in Elder Patients,” Chinese Journal of Traumatology, Vol. 11, No. 2, 2008, pp. 89-93. doi:10.1016/S1008-1275(08)60019-X
- D. M. Wright, S. Blanckley, G. J. Stewart and G. P. Copeland, “The Use of Orthopaedic POSSUM as an Audit Tool for Fractured Neck of Femur,” Injury, Vol. 3, No. 4, 2008, pp. 430-435. doi:10.1016/j.injury.2007.11.009
- G. S. Gu, D. B. Zhang, B. H. Zhang and N. K. Sun, “Evaluation of P-POSSUM Scoring System in Predicting Mortality In Patients with Hip Joint Arthroplasty,” Chinese Journal of Traumatology, Vol. 9, No. 1, 2006, pp. 50-55.
- P. P. Tekkis, H. M. Kocher and N. J. Kessaris, “How AcCurate Is POSSUM and P-POSSUM in Predicting Mortality in Emergency Surgery and in Old Age?” British Journal of Surgery, Vol. 88, Suppl. 11, 2001, pp. 42-43.
- J. Hirose, J. Ide, H. Irie, K. Kikukawa and H. Mizuta, “New Equations for Predicting Postoperative Risk in Patients with Hip Fracture,” Clinical Orthopaedics and Related Research, Vol. 467, No. 12, 2009, pp. 3327-3333. doi:10.1007/s11999-009-0915-6
Appendix 1
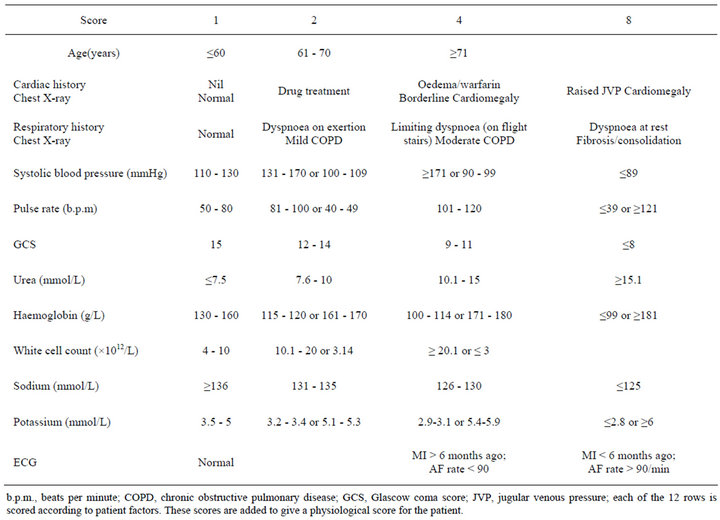
Table A1. POSSUM physiological score.
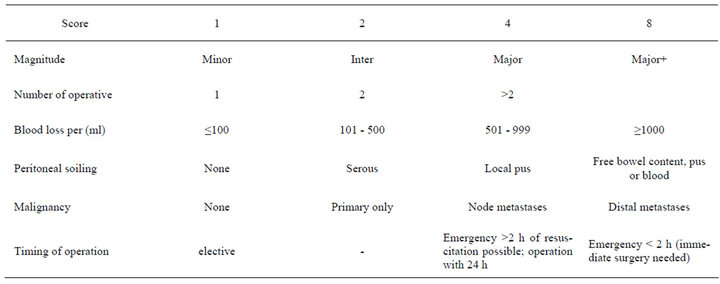
Table A2. POSSUM operative score.
Appendix 2
Peri-Operative Clinical Care
Patients who were enrolled in this study were treated according the hospital guidelines for hip fracture in the elderly. All of them received peri-operative analgesia with parenteral metamizole and paracetamol q6 h and intravenous morphine as needed to achieve a VAS pain score of <4. Skin traction was routinely applied to the injured leg before surgery. All patients were included in a protocol for prevention of pressure sores. Intravenous fluid therapy, started immediately after admission, consisted of 10 - 30 ml/kg/day Ringer’s lactate solution and transfusion, if haemoglobin was <9 (g/dl). Patients fasted for at least 6 h before surgery. All of them received pre-operative prophylaxis against venous thrombosis involving thromboembolic deterrent stockings and subcutaneous unfractionated heparin. Antibiotic prophylaxis was started before induction of anaesthesia and continued for 72 h. Anaesthesia and surgery were always performed by staff anaesthesiologists and surgeons during office hours. Post-operatively, fluid therapy consisted of 2000 ml of Ringer’s-glucose 5% solution per 24 h. Supplementary oxygen was given for at least 6 h after surgery. The patients were allowed to eat after 6 h and nutritional supplementation (oral protein energy supplements) was added in patients who were malnourished at the time of the fracture or if they had poor food intake in the hospital. Mobilization and rehabilitation were started as soon as possible (ideally during the first 72 h) and the discharge plan was discussed with both patients and relatives.
Appendix 3
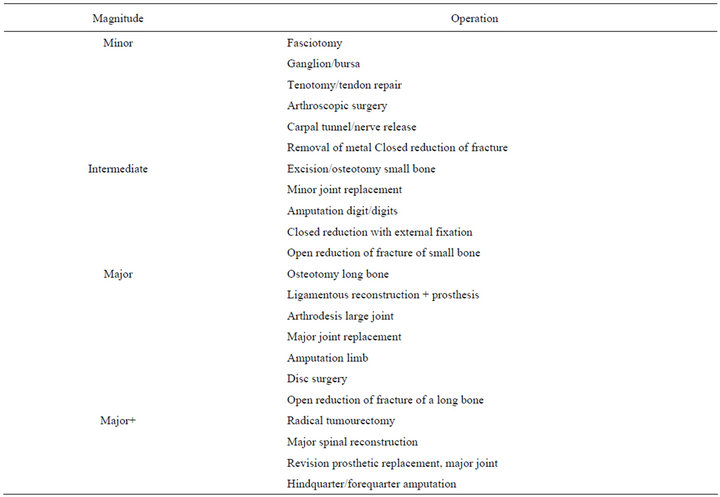
Table A3. Orthopedic complexity.
NOTES
*Conflict of Interest: We declare there isn’t any conflict of interest. Funding: This research needed no funding.
#Corresponding author.

