Open Journal of Orthopedics
Vol.2 No.2(2012), Article ID:20107,6 pages DOI:10.4236/ojo.2012.22004
Endocsopic Decompression of Intermetatarsal Nerve (EDIN) for the Treatment of Morton’s Entrapment— Multicenter Retrospective Review*
![]()
1College of Health Sciences, Midwestern University, Glendale, USA; 2Hospital Quiron, Barcelona, Spain; 3Private Practice, Houston, USA; 4Private Practice, Midland, USA; 5College of Health Sciences, Midwestern University, Glendale, USA.
Email: slbarrettpod@me.com
Received February 20th, 2012; revised March 29th, 2012; accepted April 11th, 2012
Keywords: Morton’s Neuroma; Morton’s Entrapment; Neuroma; Endoscopic Decompression
ABSTRACT
Background: The authors present the results of a four surgeon, multicenter study of endoscopic decompression for the treatment of Civinini-Morton’s entrapment of 193 interspaces. Methods: A retrospective review of 193 interspaces, which were decompressed by four different surgeons. Results: The overall success rate was high, with 92% of patients reporting a good or fair outcome. Higher success rates were reported in the 3rd interspace decompression group (95%) compared to the 2nd interspace decompression group (85%). Complications reported were minimal, with only seven cases requiring a revision with traditional neurectomy. No revisions were required in the 3rd interspace decompression group. Five of the revisions were in the 2nd interspace decompression group, with the remaining two revisions in the combined 2nd/3rd interspace decompression group. Conclusions: Endoscopic decompression for the treatment of Civinnini-Morton’s entrapment is a safe and efficacious method of treatment of this nerve entrapment, with very low complication rates and rapid return to normal activity.
1. Introduction
Morton’s entrapment is often erroneously referred to as Morton’s “Neuroma”, due to a history of inaccurate use of nomenclature [1]. This entrapment causes a degenerative process in which the common plantar digital nerve (intermetatarsal nerve) nerve demonstrates demyelination of nerve fibers and fibrosis of the endoneurium on histologycal examination [2]. This condition is a focal forefoot nerve entrapment.
Several etiological theories have been proposed for Morton’s entrapment, including hypermobililty of the metatarsal heads by Hoadley in 1893 [3], nerve ischemia by Nissen in 1948 [4], and pronation in propulsion in those with flat feet by Root in 1977 [5].
Multiple studies have recently indicated nerve entrapment as the primary underlying cause of this condition [6- 8]. In addition, via results from both open and endoscopic surgical decompression techniques, Morton’s neuroma has been demonstrated to be an entrapment phenomenon [9-14].
Therefore, as a true peripheral nerve entrapment, “Morton’s neuroma” should more precisely be referred to as simply a forefoot nerve entrapment, especially since Civinini described the condition many years prior to Morton’s; perhaps “Civinini-Mortons” entrapment would be the most accurate nomenclature [1,14]? A sad conesquence of this historical misnomer is that clinical decision-making has been effected by a descriptive name that was accepted long before a true etiological basis had been elucidated. Indeed, when a treating surgeon perceives the condition as a “neuroma”, surgical intervention may be postponed while treatment modalities considered as more “conservative” are initiated, many of which involve infliction some type of peripheral nerve injury. Unfortunately, many of these treatments, such as sclerosing or alcohol injections, can do more harm than good, and have been associated with deleterious outcomes [1,15].
It is common practice to encounter patients diagnosed with Morton’s entrapment who have been treated by local steroid injection [16]. As peripheral nerve entrapments will produce the same histological response independent of the anatomical location of the nerve that is entrapped [17], it could be surmised that peripheral nerve impingement syndromes in locations other than the lower extremity are treated by similar methods. This, however, is not the case. Though a mainstay of treatment regimens, steroid injections are avoided in the treatment of other compression syndromes, such as carpal tunnel syndrome, a compression syndrome of the median nerve in the wrist, as steroids are widely considered and have been shown to increase the risk of iatrogenic injury if used pre-operatively [17]. It has also been found that permanent nerve injury will result if steroids are injected directly into a fascicle [18]. Furthermore, plantar plate disruption, with associated medial or lateral deviation of the digit, is commonly seen in patients that have been injected with steroids for treatment of an entrapment, especially in the 2nd interspace [14]. This decreases the chance of later restoration of function in even the most reliable of surgical interventions.
The delay in time between diagnosis and eventual surgical intervention, while other senseless and ineffectual treatments are attempted, comes at the expense of positive surgical outcomes; as some studies have found postoperative surgical success to be inversely related to the duration of symptoms [18]. Indeed, in the case of countless podiatric patients, poor long-term outcomes are a direct consequence of inadequate and erroneous nomenclature, which has lead to perpetuation of dogmatic myth, and subsequent decreases in patient surgical outcomes.
Traditionally, surgical excision has been initiated after failure of conservative care, and has been considered the routine surgical intervention following “conservative” treatment. It has been repeatedly reported that surgical excision is efficacious in anywhere from 66% - 85% of cases. Many of these results must be questioned, as no standardized evaluation scale was used between studies, potentially augmenting cohort results. In fact, Womack and Richardson, et al., recently reported only 50% “good or excellent” results with excision in 120 patients, with 40% poor results [18]. Womack’s conclusion was “outcomes of neuroma excision do not appear to be as successful as long term follow-up previously reported [19].”
In addition to questionable reported outcomes, there are inherent risks of denervation procedures, such as the development of painful true neuromas, formation of hematomas, and numbness of adjacent toes [20]. It has been established that amputation neuromas, which always occur after resection of Morton’s entrapment, can become spontaneous pain generators, leading to severe conditions such as CRPS (Chronic Regional Pain Syndrome), a chronic progressive disease characterized by severe levels of pain [21].
There is no other peripheral nerve entrapment in the human body treated primarily through surgical resection [21]. Decompression procedures are the mainstay for all other cases of human primary nerve entrapment [18,21]. Risks associated with peripheral nerve decompression procedures are minimal in comparison to excision procedures, and have been shown to produce excellent results in a number of studies [9,11,14,21-23].
Excellent or good results were reported in 83% of patients treated by open transection of the deep transverse metatarsal ligament, as described by Gauthier (Figure 1) [9]. It must be noted that all open procedures are subject to a certain degree of inherent risk. These risks can be minimized through the use of minimally invasive or endoscopic procedures for surgical decompression. Some minimally invasive or endoscopic foot procedures are typically associated with less postoperative complications as opposed to “open” procedures for the same condition [24,25]. Further, Villas, Flores, and Alfonso reported “additional benefits, such as minimal tissue trauma, resulting in less post-operative pain, and earlier return to regular activity [26].”
The authors have been successfully performing minimally invasive, endoscopic decompression for the treatment of Morton’s entrapment for almost two decades, with a high success rate, and very low complication and revision rates [12].
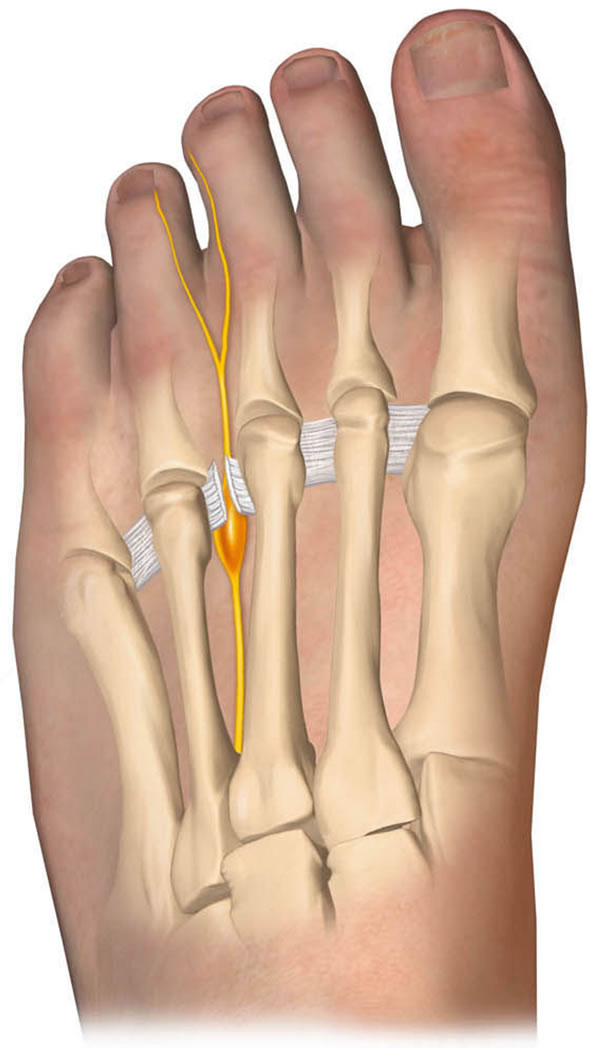
Figure 1. Third interspace Morton’s entrapment treated through transection of the intermetatarsal ligament.
2. Materials and Methods
The authors present the clinical results of a retrospective, multi surgeon, and multicenter study of the EDIN (endoscopic decompression for intermetatarsal nerve) surgical technique for the treatment of Morton’s entrapment.
All patients presented between 2007 and 2010. Preoperative clinical diagnoses were established based on careful examination of findings from clinical evaluation, history of the present illness, pain on palpation, duration of symptoms, and thorough review of radiographic imaging, including diagnostic ultrasound, which has been shown to be an effective aid in proper diagnosis of Morton’s entrapment [27-29].
Care upon clinical examination of each patient was taken to confirm that perceived pain on palpation was in the interspace between metatarsal heads, and not on any adjacent structures, which would be indicative of other pathological conditions, such as capsulitis, plantar plate rupture, degenerative joint disease, and stress fractures. Diagnostic nerve blocks of affected interspaces with small amounts of lidocaine were also used, to allow for clinical assessment of adjacent interspaces.
Following a clinical diagnosis of intermetatarsal nerve entrapment, affected interspaces were surgically decompressed. All surgeons used the Instratek Edintrak II system for decompression intraoperatively, with similar surgical technique.
The two-portal technique used by surgeons in the study, described in detail elsewhere as it is outside of the scope of this paper, involves a dorsal portal incision made proximally to the metatarsophalangeal joint transversely [12-14]. This allows the surgeon to put the transverse metatarsal ligament into a rigid position via the placement of a metatarsal retractor, following careful dissecttion (Figure 2). A second incision is made in the distal web space transversely, to allow a canula/obturator to be placed directly inferior to the transverse metatarsal ligament, thus avoiding any sort of direct contact with the plantar neurovasculature bundle, which lies below the cannula superficially. The obturator is then removed and a scope is placed into the canula so that the transverse metatarsal ligament can be visualized in contact with the superior margin of the canula (Figure 3). Once properly visualized, an angled hook knife is introduced into the canula, and the surgeon transects and subsequently releases the transverse metatarsal ligament (Figure 4).
Post-operative management includes application of a light gauze compression dressing, which is removed by the patient the next day. Patients are allowed to fully weight bear to tolerance and wear any comfortable shoe. Patients are advised that they can shower regularly the next day, but cannot immerse or soak their foot until one week after the sutures are removed at 10 - 14 days. They
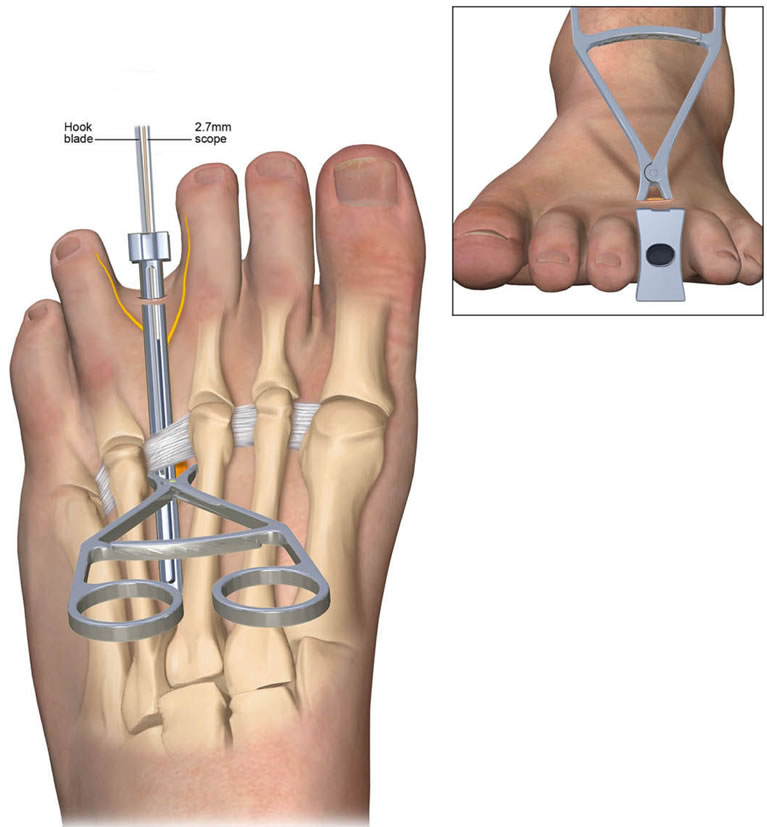
Figure 2. Placement of the intermetatarsal ligament into a rigid position via the placement of a metatarsal retractor.
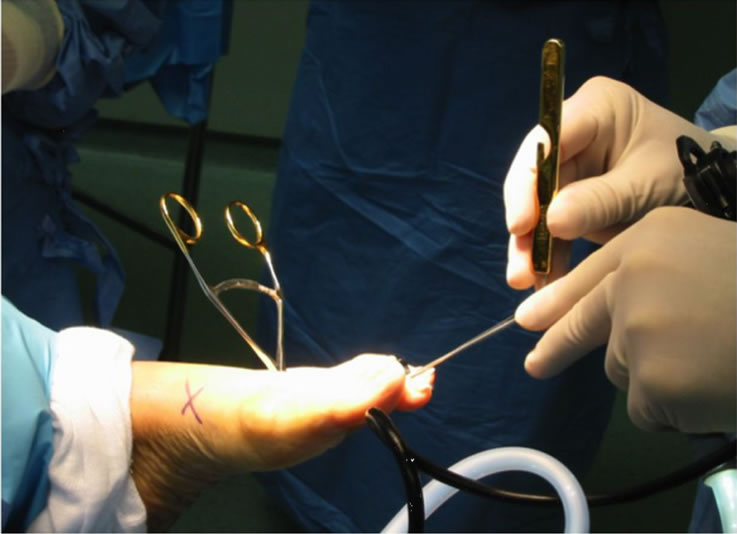
Figure 3. Intraoperative photo showing the hook blade being passed interdigitally into the cannula alongside the scope.

Figure 4. Endoscopic transection of the intermetatarsal ligament.
are also advised that they can resume activity to tolerance, and that intermittent ice application at the end of the day is suggested.
Postoperative surgical interviews were conducted at a minimum of 16 weeks following the procedure, and participants were asked to give a subjective and general self-evaluation of their outcomes. Surgical outcomes were rated subjectively as either “good”, “fair”, or “poor” (Table 1).
Collected data was analyzed for success in isolated 2nd or 3rd interspace release, simultaneous 2nd/3rd interspace release, overall revision rates (conversion to open neurectomy), and inter-surgeon reliability.
3. Results
Four surgeons decompressed a total of 193 interspaces, including 76 second, 117 third, and 66 simultaneous 2nd/ 3rd interspaces. Seven of these interspaces required revision surgery via “open” neurectomy. Complications were minimal, with one hematoma reported.
Success rates, as determined by patient self-evaluation, were high with 92% of patients reporting a “good” or “fair” outcome, and only 7.7% of patients reporting a “poor” outcome (Figure 5). Success rates were decreased in isolated 2nd interspace releases when compare to isolated 3rd interspace releases (Table 2). No revision surgeries were needed in the 3rd interspace group, whereas a total of 5 were needed in the 2nd interspace group. Patients in the isolated 3rd interspace group reported a 95% “good” or “fair” success rate. Isolated 2nd interspace decompression rates of “good” or “fair” ratings were slightly less at 85%.
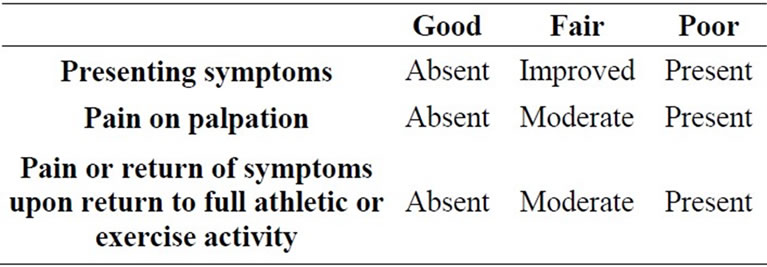
Table 1. Patient subjective evaluation scale.
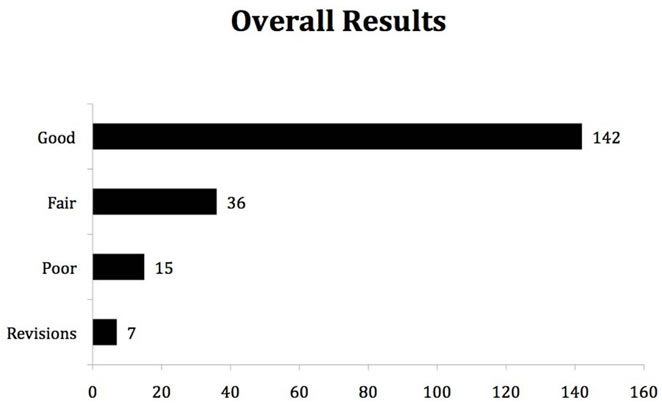
Figure 5. Overall results using patient subjective rating scale.
One surgeon did not compile data for outcomes in the simultaneous 2nd and 3rd decompression group, but in the 36 cases of simultaneous decompression that were documented, success rates were noted as 58% (21/36) “good”, 33% (12/36) “fair”, and 8% (3/36) “poor”. One revision neurectomy was needed in this group. The combined “good/fair” efficacy for the simultaneous 2nd and 3rd decompression group was 91%, which interestingly is higher than isolated 2nd interspace decompressions.
Surgeon reproducibility averaged 91.4% amongst the four surgeons participating in the study (Table 3). One surgeon, who had a disproportionate number of bilateral cases and a reproducibility of 76%, augmented this number. The average reproducibility of the other three without the outlier was 96.5%.
4. Discussion
It is the shared opinion of the authors that the EDIN technique is superior to open surgical neurectomy for the treatment of Morton’s entrapment, as EDIN is favorable in success rate and has almost no complications. Our 92% overall rate of success, as defined by subjective postoperative patient ratings of “Good” or “Fair”, was found to be similar to other endoscopic release studies [11,14,22].
Though self-reported patient ratings present a viable way of determining success rates for procedures such as EDIN, their purely subjective nature lends itself to inherent inaccuracies. In addition, no standardized means of rating patient outcomes has been used in the numerous studies that have analyzed Morton’s entrapment. If a standardized rating system were to be used by all authors, larger cohorts could be conducted, giving greater insight into this entrapment. Future studies could also benefit from rating systems in which objective variable assessments systems are designed and used in determining relative success rates.

Table 2. Isolated 3rd vs. 2nd interspace decompressions.
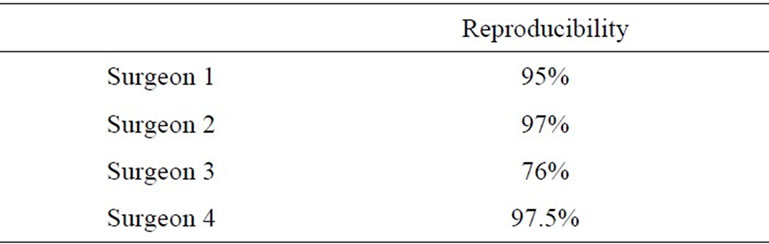
Table 3. Surgeon reproducibility.
The use of steroid injections as a means of “conservative” treatment of Morton’s entrapment is not advised, as these injections do not create a sensible means of long term relief and do little to address the apex of the pathology. In addition, steroid injections may directly damage the nerve and may cause other deleterious effects, such as plantar plate ruptures [14]. Further, no other primary nerve entrapment in the human body is treated by open resection [21].
It is well known that higher complication rates are found when any type of peripheral nerve destruction or ablation procedure is performed when compared to neurolysis. The likelihood of the development of peripheral nerve injuries or amputation neuromas is rare via the use of the EDIN technique. Our rate of conversion to open neurectomy of 3.6% further confirms this.
The authors postulate that the lower success rate seen in 2nd interspace decompression in comparison to 3rd interspace decompression is likely due to the increased complexity of pathomechanics occurring in the 2nd ray, as well as the potential for undiagnosed, concomitant conditions to be present upon clinical diagnosis of Morton’s entrapment. The diagnosis of Morton’s entrapment is often based solely on clinical signs and symptoms [29]. Conditions that mimic peripheral nerve entrapments need to be ruled out when an entrapment is suspected in the 2nd interspace, a common location of such pathologies. Thus, it is imperative that coexisting conditions of equinus, capsulitis, or metatarsalgia due to partial plantar plate rupture, be appreciated pre-operatively, if successful surgical outcomes are to be achieved.
There can be a significant learning curve with the EDIN technique, but once it is overcome surgeon reproducibility is high. The one surgeon outlier in our multi surgeon study had a higher number of bilateral cases, which may have contributed to an overall lower efficacy rate. However, it is important to note that the conversion to open neurectomy was the lowest in the group.
5. Conclusion
Endoscopic decompression of intermetatarsal nerve (EDIN), as evidenced by postoperative subjective ratings, is a viable and efficacious technique for the treatment of Morton’s entrapment, often referred to erroneously as Morton’s Neuroma. EDIN is not only favorable in success rate and complications to open nerve resection procedures, but also has high surgeon reproducibility once the learning curve is overcome.
REFERENCES
- E. E. Larson, S. L. Barrett, B. Battiston, C. T. Maloney Jr. and A. L. Dellon, “Accurate Nomenclature for Forefoot Nerve Entrapment: A Historical Perspective,” Journal of the American Podiatric Medical Association, Vol. 95, No. 3, 2005, pp. 298-306.
- F. Goldman, “Intermetatarsal Neuromas: Light and Electron Microscopic Observations,” Journal of the American Podiatry Association, Vol. 70, No. 6, 1980, p. 265.
- A. E. Hoadley, “Six Cases of Metatarsalgia,” Chicago Medical Recorder, Vol. 5, 1893, pp. 32-37.
- K. Y. Nissen, “Plantar Digital Neuritis, Morton’s Neuralgia,” Journal of Bone and Joint Surgery, Vol. 30-B, No. 1, 1948, pp. 84-94.
- M. L. Root, W. P. Orien and J. H. Weed, “Normal and Abnormal Function of the Foot,” Clinical Biomechanics Corp., Los Angeles, 1977.
- C. E. Graham and D. M. Graham, “Morton’s Neuroma: A Microscopic Analysis of the Interdigital Neuroma,” Foot and Ankle, Vol. 5, No. 3, 1984, pp. 150-153.
- I. J. Alexander, K. A. Johnson and J. W. Parr, “Morton’s Nueroma: A Review of Recent Concepts,” Orthopedics, Vol. 10, No. 1, 1987, pp. 103-106.
- M. J. Shereff and D. A. Grande, “Electron Microscopic Analysis of the Interdigital Neuroma,” Clinical Orthopedics, Vol. 271, 1991, pp. 296-299.
- G. Gauthier, “Thomas Morton’s Disease: A Nerve Entrapment Syndrome,” Clinical Orthopedics, Vol. 142, 1979, pp. 90-92.
- P. F. Diebold, B. Daum, V. Dang-Vu and M. Litchinko, “True Epineural Neurolysis in Morton’s Neuroma: A 5-Year Follow Up,” Orthopedics, Vol. 19, No. 5, 1996, pp. 397-400.
- A. L. Dellon, “Treatment of Morton’s Neuroma as a Nerve Compression,” Journal of the American Podiatric Medical Association, Vol. 86, No. 8, 1992, pp. 399-402.
- S. L. Barrett and T. T. Pignetti, “Endoscopic Decompression for Intermetatarsal Nerve Entrapment—The EDIN Technique: Preliminary Study with Cadaveric Specimens; Early Clinical Results,” Journal of Foot and Ankle Surgery, Vol. 33, No. 5, 1994, pp. 503-508.
- S. L. Barrett and A. S. Walsh, “Endoscopic Decompression of Intermetatarsal Nerve Entrapment: A Retrospective Study,” Journal of the American Podiatric Medical Association, Vol. 96, No. 1, 2006, pp. 19-23.
- S. L. Barrett, “Endoscopic Nerve Decompression,” Clinics in Podiatric Medicine and Surgery, Vol. 23, No. 3, 2006, pp. 579-595. doi:10.1016/j.cpm.2006.05.002
- N. Espinosa, J. D. Seybold, L. Jankauskas, et al., “Alcohol Sclerosing Therapy Is Not an Effective Treatment for Interdigital Neuroma,” Foot and Ankle International, Vol. 32, No. 6, 2011, pp. 576-580. doi:10.3113/FAI.2011.0576
- J. Greenfield, J. Rea and F. W. Llfed, “Morton’s Interdigital Neuroma: Indications for Treatment by Local Injections versus Surgery,” Clinical Orthopedics, Vol. 185, 1984, pp. 142-144.
- C. L. Hankins, M. G. Brown, R. A. Lopez, et al., “A 12-Year Experience Using the Brown Two-Portal Endoscopic Procedure of Transverse Carpal Ligament Release in 14,722 Patients: Defining a New Paradigm in the Treatment of Carpal Tunnel Syndrome,” Plastics and Reconstructive Surgery, Vol. 120, No. 7, 2007, pp. 1911- 1921. doi:10.1097/01.prs.0000287287.85044.87
- S. E. MacKinnon and A. L. Dellon, “Surgery of the Peripheral Nerve,” Thieme Medical Publishers, New York, 1988.
- C. Villas, B. Florez and M. Alfonso, “Neurectomy versus Neurolysis for Morton’s Neuroma,” Foot and Ankle International, Vol. 29, No. 6, 2008, pp. 578-80. doi:10.3113/FAI.2008.0578
- I. Ducic, A. N. Mesbahi, C. E. Attinger and K. Graw, “The Role of Peripheral Nerve Surgery in the Treatment of Chronic Pain Associated with Amputation Stumps,” Plastics and Reconstructive Surgery, Vol. 121, No. 3, 2008, pp. 908-914. doi:10.1097/01.prs.0000299281.57480.77
- A. L. Dellon, “Treatment of Recurrent Metatarsalgia by Neuroma Resection and Muscle Implantation: Case Report and Proposed Algorithm of Management for Morton’s ‘Neuroma’,” Microsurgery, Vol. 10, No. 3, 1989, pp. 256-259.
- S. L. Shapiro, “Endoscopic Decompression of the Intermetatarsal Nerve for Morton’s Nueroma,” Foot and Ankle Clinics, Vol. 9, No. 2, 2004, pp. 397-407.
- B. R. Vito and L. M. Talarico, “A Modified Technique for Morton’s Neuroma,” Journal of the American Podiatric Medical Association, Vol. 93, No. 3, 2003, pp. 190- 194.
- S. Kinley, S. Frascone, S. Calderone, et al., “Endoscopic Plantar Fasciotomy versus Traditional Heel Spur Surgery: A Prospective Study,” Journal of Foot and Ankle Surgery, Vol. 32, No. 6, 1993, pp. 595-603.
- R. L. Tomczak and B. D. Haverstock, “A Retrospective Comparison of Endoscopic Plantar Fasciotomy to Open Plantar Fasciotomy with Heel Spur Resection for Chronic Plantar Fasciitis/Heel Spur Syndrome,” Journal of Foot and Ankle Surgery, Vol. 34, No. 3, 1995, pp. 305-311. doi:10.1016/S1067-2516(09)80065-3
- C. Villas, B. Florez and M. Alfonso, “Neurectomy versus Neurolysis for Morton’s Neuroma,” Foot and Ankle International, Vol. 29, No. 6, 2008, pp. 578-580. doi:10.3113/FAI.2008.0578
- L. A. Ernberg, R. S. Adler and J. Lane, “Ultrasound in the Detection and Treatment of a Painful Stump Neuroma,” Skeletal Radiology, Vol. 32, No. 5, 2003, pp. 306-309. doi:10.1007/s00256-002-0606-9
- S. Kaminsky, L. Griffin, J. Milsap, et al., “Is Ultrasonography a Reliable Way to Confirm the Diagnosis of Morton’s Neuroma?” Orthopedics, Vol. 20, No. 1, 1997, pp. 37-39.
- F. D. Youngswick, “Intermetatarsal Neuroma,” Clinics in Podiatric Medicine and Surgery, Vol. 11, No. 4, 1994, pp. 579-592.
NOTES
*Financial Disclosure: Stephen L. Barrett, D.P.M. was a paid medical consultant for Instratek, Inc., which manufactures the EDIN instrumentation. None of the other authors have any financial disclosure.

