Advances in Infectious Diseases
Vol.07 No.02(2017), Article ID:76227,10 pages
10.4236/aid.2017.72004
Relationship between Self-Reported Vaccination History and Measles and Rubella Antibody Titers in Medical and Nursing Students
Masanori Ogawa1*, Ryusuke Ae2, Teppei Sasahara3
1Health Service Center, Jichi Medical University, Tochigi, Japan
2Division of Public Health, Center for Community Medicine, Jichi Medical University, Tochigi, Japan
3Division of Clinical Infectious Diseases, Department of Infection and Immunity, Jichi Medical University, Tochigi, Japan

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: April 21, 2017; Accepted: May 15, 2017; Published: May 18, 2017
ABSTRACT
In hospitals, infection control for measles and rubella is important. Medical and nursing students as well as healthcare workers must have immunity against these diseases. Many countries have adopted requirements for healthcare workers’ documented vaccination history or laboratory tests as evidence of their immunity. Evaluating a written vaccination history is difficult in many cases. Therefore, we compared measles and rubella antibody titers with self-reported vaccination history and we evaluated the association between the history and measles and rubella antibody titers, using the medical and nursing students’ data. We analyzed 564 data for measles and 558 data for rubella. Vaccination history was requested to be completed as accurately as possible. Students with one or more measles or rubella vaccinations had high positive ratios of titer, and the ratio was significantly higher than that of the students without vaccinations. The positive ratio between the two-dose and one-dose vaccination groups was not significantly different for measles or rubella (measles: p = 0.534, rubella: p = 0.452). Although it should be requested that the history is complete by using other resources, such as referring to maternity passbooks or proof of vaccination, self-reported history may be useful to confirm immunity, even if there is a possibility that the history is not accurate.
Keywords:
Vaccine, Measles, Rubella, Immunity

1. Introduction
Measles and rubella are very contagious infectious diseases [1] . Especially, in hospitals, there is a risk of transmission to unimmunized patients and coworkers by infected workers, and an outbreak can occur. Infection control is thus especially important in hospitals and other healthcare settings. The confirmation of immunity among healthcare workers is crucial to the prevention of measles and rubella outbreaks.
Japan, the United Kingdom (UK), and Australia have adopted guidelines requiring a documented vaccination history or evidence of immunity by laboratory test as proof of immunity for healthcare workers [2] [3] [4] [5] . The United States (US), Canada, and New Zealand have also adopted a requirement for the laboratory confirmation of disease in addition to a written vaccination history or laboratory evidence of immunity as evidence of immunity for healthcare workers [6] [7] [8] [9] .
The number of people infected with measles or rubella in developed countries has recently dropped [10] [11] , but measles and rubella infections are not always diagnosed using laboratory confirmation; in some cases, they are diagnosed based on clinical findings. Therefore, the documentation of an individual’s vaccination history or laboratory evidence of immunity is a realistic way to determine immunity in healthcare workers.
Regarding laboratory evidence of immunity, the measurement of antibodies for measles and rubella is relatively expensive. If a self-reported vaccination history could be used to identify the individuals who need one or more vaccinations, then unnecessary antibody titers could be avoided.
However, evaluating the healthcare workers’ written vaccination history itself can be difficult because they may not have their vaccination documents available. Therefore, a vaccination history depends on self-reports in most cases, and there are significant differences among individuals in the accuracy of their self-reported vaccination histories because some individuals compile these histories based on maternity passbooks, whereas others depend on their memory or their parent’s memory. The accuracy of self-reported vaccination histories is very important, especially if a self-reported vaccination history is adopted as an evidence of immunity.
Medical and nursing students practice at hospitals and these students are considered to be equal to healthcare workers from an infection control standpoint. Therefore, evaluating these students’ immunity for measles and rubella is also necessary.
In the present study, using the medical and nursing students’ data, we compared measles and rubella antibody titers with the students’ self-reported vaccination history, which was requested to be completed as accurately as possible, and evaluated the association between the self-reported vaccine history and measles and rubella antibody.
2. Materials and Methods
2.1. Participants
The data of 660 medical and nursing students (287 men, 373 women) were used. These were all students enrolled in Jichi Medical University from 2013-2015. The age distribution was 18 - 30 years (median: 19 years) and all students were Japanese.
2.2. The Participants’ Ages at Each Vaccination and Infection
Prior to their enrollment at the university, we asked all students’ parents to complete a vaccination history (using a template that we created), which included their age at each vaccination and whether they had experienced an infection of measles or rubella and, if “yes”, their age at the onset of each infection.
Vaccination history and experience of infection were requested to be completed as accurately as possible.
2.3. Laboratory Evidence of Immunity
During the students’ first school year, the measles and rubella immunoglobulin G (IgG) antibody titers of each student were measured by an enzyme immunoassay (CDC) method, which was performed by a commercial company (LSI Medience, Tokyo, Japan).
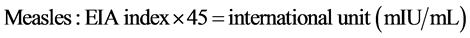
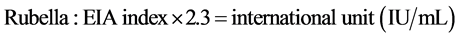
The data measured by this method are shown as the EIA index. An EIA index score of ≥4 was considered positive. For the comparison of the EIA index with the international unit, we used the following formulae for conversion [12] :
2.4. Analysis
We analyzed the students’ measles and rubella IgG antibody titers according to the vaccine dose. Although all students had submitted a completed vaccination and infection template, several templates were incomplete, and the age at which some students had received some vaccinations was unclear. We excluded these students’ data from the analysis.
Moreover, as mentioned above, measles and rubella are not always diagnosed based on laboratory tests obtained at a clinical site, and we evaluated the relationship between measles and rubella antibody titers and self-reported vaccination history in this study. Thus, we also excluded the data of the students who had experienced measles or rubella infections. Finally, we analyzed 564 samples for measles and 558 samples for rubella.
To confirm the effect of vaccine doses on the positive ratio of each IgG antibody, we performed a logistic regression analysis adjusted for age and sex, using the software program JMP 10 (SAS Institute, Cary, NC, USA).
2.5. Ethics
This study was approved by the Ethics Committee of Jichi Medical University (approval No. 15-078).
3. Results
3.1. Measles
We analyzed the measles antibody titer and self-reported vaccination history of 564 students. Their data are summarized in Table 1 based on their self-reported vaccine doses (i.e., receiving no vaccinations, one vaccination, or two or more vaccinations). Among the students who had received one or more measles vaccinations, over 95% had immunity for measles regardless of the vaccine dose. In contrast, the immunity ratio in the students who reported that they had not received a measles vaccination was 70%, which was approximately 25% lower than that in the students who had received one or more vaccinations.
The logistic regression analysis showed that the odds ratios (ORs) for positive antibody titer was increased among the students with a two-dose vaccination history compared to those with no vaccination (OR, 10.2; 95% confidence interval [95% CI], 1.90 - 46.1). The ORs for positive antibody titer was also increased among the students with a one-dose vaccination history compared to that in the students who had had no measles vaccination (OR, 13.6; 95% CI, 2.63 - 57.8). There was no significant difference between the students with a two-dose vaccination history and those with a one-dose vaccination history (OR, 0.75; 95% CI, 0.31 - 1.93) (Table 2).
Table 1. Measles IgG titer based on the self-reported vaccination history.
Table 2. The association between the positive ratio of IgG titer and vaccination dose in measles.
3.2. Rubella
We analyzed 558 students’ rubella antibody titer and their self-reported vaccination history. Their data are summarized in Table 3 according to their self-re- ported vaccine doses. Among the students who had received one or more vaccinations, approximately 90% had immunity for rubella regardless of the vaccine dose. In contrast, the immunity ratio in students who had not received a rubella vaccine was 72%, which was approximately 18% lower than in the students who had received one or more vaccinations.
The logistic regression analysis showed that the ORs for positive titer were increased among the students with a two-dose vaccination history compared to those in students with a no-vaccination history (OR, 4.30; 95% CI, 1.44 - 12.1). The OR for positive titer was also increased among the students with a one-dose vaccination history compared to that in students with a no-vaccination history (OR, 3.34; 95% CI, 1.23 - 8.25). There was no significant difference between the students with a two-dose history and those with a one-dose vaccination history (OR, 1.29; 95% CI, 0.68 - 2.59) (Table 4).
Table 3. Rubella IgG titer based on the self-reported vaccination history.
Table 4. The association between the positive ratio of IgG titer and the vaccination dose in rubella.
4. Discussion
We compared measles and rubella antibody titers with the self-reported vaccination history of medical and nursing students, and evaluated the association between self-reported vaccine history and measles and rubella antibody.
According to the US Centers for Disease Control (CDC), one dose of the MMR (measles, mumps, and rubella) vaccine is about 93% (range, 39% - 100%) effective at preventing measles, and two doses are approximately 97% (range, 67% - 100%) effective. The CDC also considers one dose of the MMR vaccine as approximately 97% (range, 94% - 100%) effective at preventing rubella; in the investigation cited by the CDC, approximately 91% - 100% of individuals who had received two MMR doses had a detectable antibody level [13] . Comparing our data with those of the CDC report, the immunity level for measles is nearly the same and the immunity level for rubella is slightly lower. A Japanese study of the immunity level for rubella was also reported to be the same as those of the CDC report [14] ; thus, the reason the immunity level for only rubella is lower in the present study is unclear.
The immunity levels for measles and rubella were not vastly different from those in the previous reports; therefore, we suspected that an accurate self-re- ported vaccination history may be useful to confirm immunity and allow for the selection of the students who require vaccinations. An accurate report is one where the age at which each student had received a vaccination can be determined.
Our present findings showed that the students who had received one or more doses of a measles or rubella vaccine had a relatively high positive immunity ratio, and their ratio is significantly higher than in the students with no vaccinations. For both measles and rubella, the positive ratio was not significantly different among the two-dose and one-dose groups. Therefore, achieving immunity for measles and rubella is high even when an individual has had only one dose of the respective vaccine.
However, many countries, including Japan, the UK, Australia, the US, Canada, and New Zealand, recommend a two-dose vaccine for measles (e.g., the MMR vaccine) for healthcare workers [2] [3] [4] [6] [8] [9] . A two-dose rubella-containing vaccine (e.g., the MMR vaccine) is also recommended for healthcare workers, except in the US and Canada [2] [3] [5] [7] [8] [9] . Although in the US and Canada, one dose of the rubella-containing vaccine is recommended for healthcare workers, two-dose vaccine is common because MMR vaccine is also used for rubella. Proof of having received this vaccine is recognized as evidence of immunity.
Although it may not apply to live vaccines triggering long-term IgG antibodies for extended periods of time, the following generic pattern about immunity is indicated. After a vaccine is administered, the IgG antibody is produced, and, after increasing up to its peak value, the IgG antibody titer eventually returns to the baseline level. A booster vaccine reactivates the immune memory and results in a rapid increase in the IgG antibody titer. The antibody titer then declines with slower kinetics compared to that after the primary vaccine [15] , and thus the immunization continues for a longer period and is more effective.
The IgG titer measured after the one-dose vaccination in our study population appears to be enough, but a two-dose vaccine is desirable to maintain high level of immunity. In fact, there is a report that those who have been vaccinated twice are better protected against epidemic measles than single-dose recipients [16] .
In Japan, there are two opportunities to receive measles and rubella vaccinations for individuals born after 1990 according to Japan’s vaccination policy [17] . All students analyzed in the present study were born after 1990 except for five in the measles analysis and three in the rubella analysis. Therefore, the students’ self-reports of receiving two doses of a vaccination are reliable. However, we suspect that among the students who declared that they had received a vaccination once, there were several students who had actually received two doses. It also seems likely that, among the students who reported that they had received no vaccinations, these students had a one-dose or two-dose history. In light of our results, the precise positive ratio for individuals with a one-dose vaccination history was thus not obtained in this study, because our data were based on self-reports; the exact percentage of two-dose histories among the students who declared having received one dose was not determined.
Thus, even though the vaccination history is requested to be completed as accurately as possible, the possibility was suggested that the accuracy of these self-reports, especially among the students who stated they had received a vaccination once or not at all, are insufficient. This is the limitation of the self-re- ported vaccination history.
Consequently, the administrator should request not only that the vaccination history be completed as accurately as possible, but also that maternity passbooks or proof of vaccination be utilized. However, from our results, we may suggest as follows.
Students reporting that they have had two doses of a vaccine do not require the IgG antibody titer, whereas those reporting that they have had only one dose of a vaccine should be given an additional dose instead of the IgG antibody titer. Regarding the individuals with no history of vaccination, the IgG antibody titer should be performed and a two-dose vaccination should be administered if it is determined that they do not have immunity.
The positive classification may be overestimated because the EIA is sensitive. This measurement kit and cut-off point is widely used in Japan; therefore, we analyzed the data using this cut-off point.
In this study, we excluded the data of the students who had measles or rubella infection. However, among the students who stated that they had not received a measles or rubella vaccine, 70% and 72% had immunity, respectively. In most cases, it seems that those students actually had received a vaccine. However, there is a possibility that asymptomatic cases were not ruled out, considering the immunity levels for measles and rubella were not greatly different from those in the previous reports; thus, we thought that few asymptomatic cases existed.
According to CDC reports, a two-dose MMR vaccine is about 97% effective at preventing measles, and 91% - 100% effective at preventing rubella [13] . This indicates that, even if the individual who had received two doses of a vaccine, there is a possibility that some individuals do not have sufficient IgG antibody. There are reports that the IgG antibody titer measuring humoral immunity and cell-mediated immunity could also be used for preventing disease [18] [19] . Therefore, the development of techniques for measuring cell-mediated immunity is necessary.
5. Conclusions
In our study, although the students’ self-reports of receiving two doses of a vaccination were reliable, the vaccination history of the students who declared that they had received a vaccination once or not at all may be inaccurate. Although it is desirable that vaccination history is completed not only as accurately as possible, but also based on the maternity passbooks or proof of vaccination, self- reported vaccination history may be useful to confirm immunity, even if there is a possibility that the history is not completely accurate. Therefore, we can make the following recommendations.
Students who report that they have had two doses of a vaccine do not need an IgG antibody titer, whereas those reporting that they have had only one dose of a vaccine should be given an additional dose instead of the IgG antibody titer. Regarding the individuals with no history of vaccination, the IgG antibody titer should be performed and a two-dose vaccination should be administered if it is determined that they do not have immunity.
Competing Interests
The authors declare that they have no competing interests.
Cite this paper
Ogawa, M., Ae, R. and Sasahara, T. (2017) Relationship between Self-Reported Vaccination History and Measles and Rubella Antibody Titers in Medical and Nursing Students. Advances in Infectious Diseases, 7, 27-36. https://doi.org/10.4236/aid.2017.72004
References
- 1. Tang, J.W., Li, Y., Eames, I., Chan, P.K. and Ridgway, G.L. (2006) Factors Involved in the Aerosol Transmission of Infection and Control of Ventilation in Healthcare Premises. Journal of Hospital Infection, 64, 100-114.
https://doi.org/10.1016/j.jhin.2006.05.022 - 2. The Japanese Society of Environmental Infections (2014) Vaccination Guideline for Healthcare Workers. (In Japanese)
http://www.kankyokansen.org/modules/publication/index.php?content_id=17 - 3. Portsmouth Hospitals NHS Trust (2014) Measles, Mumps & Rubella (MMR) and Varicella (Chickenpox): Occupational Health Screening and Vaccination.
http://www.porthosp.nhs.uk/Downloads/Policies-And-Guidelines/Health-and-Safety-Policies/Measles_Mumps__Rubella_and_Varicella_Policy.doc - 4. Australian Government. Department of Health (2017) The Australian Immunisation Handbook. 10th Edition. Measles.
http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook10-home~handbook10part4~handbook10-4-9#4-9-7 - 5. Australian Government. Department of Health (2017) The Australian Immunisation Handbook. 10th Edition. Rubella.
http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook10-home~handbook10part4~handbook10-4-18#4.18.4 - 6. Centers for Disease Control and Prevention (2016) Measles. For Healthcare Professionals.
http://www.cdc.gov/measles/hcp/ - 7. Centers for Disease Control and Prevention (2016) Rubella. For Healthcare Professionals.
http://www.cdc.gov/rubella/hcp.html - 8. Government of Canada (2016) Canadian Immunization Guide: Part 3—Vaccination of Specific Populations.
https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-3-vaccination-specific-populations/page-11-immunization-workers.html#p3c10t1 - 9. Immunisation Advisory Center, The University of Auckland (2011) Evidence of Immunity: Requirements for Healthcare Personnel.
http://www.immune.org.nz/sites/default/files/resources/DiseaseEvidenceImmunityImac20111114V05Final.pdf - 10. World health Organization (2016) Measles Reported Cases.
http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tsincidencemeasles.html - 11. World health Organization (2016) Rubella Reported Cases.
http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tsincidencerubella.html - 12. Kato, H., Mori, M., Oba, M., Kawahara, H. and Kaneko, T. (2016) Persistence and Half-Lives of Anti-Measles and Anti-Rubella Antibodies in Japanese Hospital Workers: A Longitudinal Study. Internal Medicine, 55, 2587-2594.
https://doi.org/10.2169/internalmedicine.55.6762 - 13. Paunio, M., Peltola, H., Valle, M., Davidkin, I., Virtanen, M. and Heinonen, O.P. (1999) Twice Vaccinated Recipients Are Better Protected against Epidemic Measles than Are Single Dose Recipients of Measles Containing Vaccine. Journal of Epidemiology and Community Health, 53, 173-178.
https://doi.org/10.1136/jech.53.3.173 - 14. Takeuchi, J., Goto, M., Kawamura, T. and Hiraide, A. (2013) Influence of Vaccination Dose and Clinico-Demographical Factors on Antibody Titers against Measles, Rubella, Mumps, and Varicella-Zoster Viruses among University Students in Japan. Japanese Journal of Infectious Diseases, 66, 497-502.
https://doi.org/10.7883/yoken.66.497 - 15. CA Siegrist (2008) Vaccine Immunology (General Aspects of Vaccination).
http://www.who.int/immunization/documents/Elsevier_Vaccine_immunology.pdf - 16. McLean, H.Q., Fiebelkorn, A.P., Temte, J.L. and Wallace, G.S. (2013) Centers for Disease Control and Prevention. Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recommendations and Reports, 62, 1-34.
- 17. Kanamori, H., Tokuda, K., Ikeda, S., Endo, S., Ishizawa, C., Hirai, Y., Takahashi, M., Aoyagi, T., Hatta, M., Gu, Y., Yano, H., Weber, D.J. and Kaku, M. (2014) Prevaccination Antibody Screening and Immunization Program for Healthcare Personnel against Measles, Mumps, Rubella, and Varicella in a Japanese Tertiary Care Hospital. The Tohoku Journal of Experimental Medicine, 234, 111-116.
https://doi.org/10.1620/tjem.234.111 - 18. Amanna, I.J., Carlson, N.E. and Slifka, M.K. (2007) Duration of Humoral Immunity to Common Viral and Vaccine Antigens. The New England Journal of Medicine, 357, 1903-1915.
https://doi.org/10.1056/NEJMoa066092 - 19. Tosh, P.K., Kennedy, R.B., Vierkant, R.A., Jacobson, R.M. and Poland, G.A. (2009) Correlation between Rubella Antibody Levels and Cytokine Measures of Cell-Mediated Immunity. Viral Immunology, 22, 451-456.
https://doi.org/10.1089/vim.2009.0068


