Modern Plastic Surgery
Vol.05 No.02(2015), Article ID:53864,4 pages
10.4236/mps.2015.52002
Periorbital Post-Inflammatory Hyperpigmentation after Fractionated CO2 Laser Resurfacing in Asians
Randal Tanh Hoang Pham1, Ingerlisa Mattoch2, Sterling S. Baker3,4
1Aesthetic and Refractive Surgery Medical Center, San Jose, USA
2Private Practice, Fort Collins, USA
3Department of Ophthalmology, College of Medicine, University of Oklahoma, Oklahoma City, USA
4Department of Dermatology, College of Medicine, University of Oklahoma, Oklahoma City, USA
Email: randalpham@lasernews.com
Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 20 January 2015; accepted 6 February 2015; published 9 February 2015
ABSTRACT
Background: Most data on laser resurfacing have come from studies of people with Fitzpatrick skin types 1 - 3; however, the world’s population is comprised mostly of Fitzpatrick skin types 4 - 6, which are more susceptible to post-inflammatory hyperpigmentation (PIH). Objective: For the purpose of expanding the expertise of plastic surgeons treating patients with darker skin types, this study examined the incidence of PIH in Asians who underwent laser resurfacing, including a histologic arm on fractional ablative resurfacing. Methods & Materials: The clinical study included six subjects of Vietnamese origin who underwent single-depth fractionated CO2 laser resurfacing. The histologic study involved a seventh subject. The MiXto SX® laser with a new scanning hand- piece was used, along with magnifying loupes to assess ablative depth after each of three laser passes performed. Photographs were taken at various postoperative intervals. Results: All six clinical subjects showed cosmetic improvement in skin texture and tone with no post-inflamma- tory hyperpigmentation. In the histologic study, H&E stained sections revealed uniform diathermy. Conclusion: It is possible to significantly reduce PIH in darker skinned subjects through use of a new scanning handpiece and a technique using loupes to assess the depth of ablative resurfacing. The histologic study confirms these findings.
Keywords:
Laser, CO2 Laser, CO2 Laser Resurfacing, Fractionated CO2 Laser Resurfacing, PIH, Post Inflammatory Hyperpigmentation, Asian, Face, Eyelid, Pigment, Wrinkles, Rhytid

1. Background
Laser therapy, one of the most significant advances in modern aesthetic surgery, is widely used with great success to treat various aesthetic and dermatologic conditions in humans. To date, most data on laser-assisted photorejuvenation have been derived from studies of people with white skin of Fitzpatrick types 1 - 3. However, the world’s population is comprised of mostly Fitzpatrick skin types 4 - 6. By the year 2056, it is predicted that more than 50% of the US population will be of non-white-European descent [1] . Currently in the US, Europe and Asia, there is a high demand for laser aesthetic procedures among people with these ethnic skin types.
The most visible signs of photoaging in ethnic skin are fine wrinkling and mottled pigmentation [2] . In Asians, particularly among the lighter-complexioned Chinese, Koreans, and Japanese, the signs of photoaging are solar lentigines, seborrheic keratoses, and deeper wrinkling. These symptoms usually do not develop until the age of 50. However, among lighter-complexioned Asians living in countries where sun exposure is more intense (such as Cambodia, Thailand, and Singapore), the signs of photoaging can develop at an earlier age [3] .
Laser resurfacing in Asians has been known to increase the risk of post-inflammatory hyperpigmentation (PIH) [4] . Despite claims of ever safer technologies, laser treatments (including those employing multiple lasers, as well as ablative, non-ablative, fractionated, and nonfractionated lasers) have failed to completely eliminate the risk of PIH.
2. Objective
Given the demand and demographic trends, dermatologists, plastic surgeons, and oculoplastic surgeons must expand their expertise and comfort level in laser-assisted aesthetic treatment of darker skin types.
In this pilot prospective study, evidence of PIH is specifically examined in a group of Vietnamese patients with Fitzpatrick skin types 4 and 5 who underwent single-depth fractionated CO2 laser resurfacing. A literature search showed that this is the first prospective clinical study with a histologic arm to examine fractional ablative resurfacing and the incidence of PIH in Asians.
3. Methods & Materials
3.1. Clinical Study
Subjects selected for single-depth fractionated CO2 laser resurfacing were six people of Vietnamese origin: four females and two males with ages ranging from 26 to 45. Inclusion criteria were presence of lentigines or rhytidosis in the lower eyelids. Exclusion criteria included the followings: no aesthetic surgery of any kind during the previous 12 months, no history of herpetic infection, no history of hyperpigmentation from any cause, and no history of treatment with isotretinoin. A complete history and examination was performed to rule out ocular melanosis and other hyperpigmentation conditions.
The MiXto SX® laser was used for the study. The lower eyelid was selected as the anatomic site for treatment. Eye protection for patients was achieved with non-reflective internal ocular shields. Topical proparacaine 0.5% was used for ocular anesthetic effect. Skin anesthesia was achieved with lidocaine 5% cream. Laser settings were: pulse width 2.5 ms, pulse energy 15 mJ, and pulse fluence 21 J/cm2. Resurfacing was performed with a 300 µm diameter spot size scanning handpiece set at 20% tissue density and no intra-operative cooling. A square 8 mm × 8 mm shape was selected to correspond to the smallest preprogrammed scan size. Care was taken to eliminate or minimize any overlap of individual scans. Using magnifying loupes (at 2.5× magnification) to assess ablative depth after each pass, three laser passes were performed with no debridement of devitalized tissue between passes or at end of treatment. Aquaphor® ointment was applied to the lower lids during the first postoperative week. Polarized sun glasses were provided to all six patients during the postoperative period, and all patients were encouraged to use these glasses to prevent post-inflammatory hyperpigmentation. Postoperative photographs were taken at day 1, day 7, and then at 1-month, 2-month, and 6-month intervals. Photographs were blindly evaluated by an oculoplastic surgeon specifically looking for evidence of hyperpigmentation (purple-red darkening of skin in the lower eyelids). All six patients were asked whether they subjectively noted hyperpigmentation in the postoperative period.
3.2. Histologic Study
An additional seventh subject was selected for the histologic study. This subject was an 80-year-old Vietnamese female patient who also met all the criteria to be included in the clinical arm of the study.
Resurfacing of one 8 mm × 8 mm square-shaped area (corresponding to the smallest preprogrammed scan size) using the methods described above was performed on the upper eyelid of the subject. The upper eyelid skin was immediately excised using the cutting handpiece set in continuous wave mode at 5 watts. The tissue was placed into 10% formalin for fixation. Microscopic examination of the tissue was achieved by paraffin embedding of the formalin-fixed tissue, microtome sectioning at 5 microns, followed by hematoxylin-eosin staining (H & E).
4. Results
4.1. Clinical Study
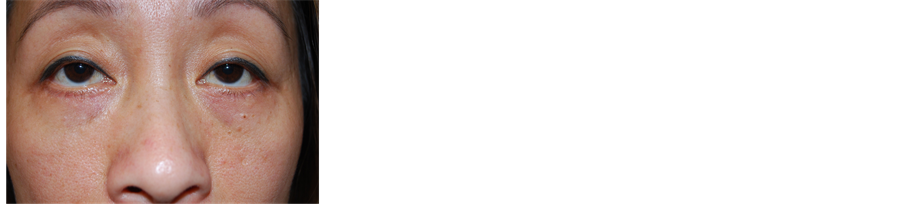
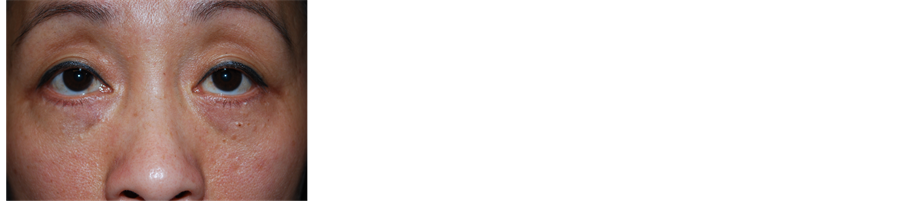
All six subjects received subjective cosmetic improvement in overall skin texture and tone with no post-in- flammatory hyperpigmentation subjectively noted by the subjects or objectively noted by the independent observer postoperatively at day 1, day 7, or at 1-month, 2-month, and 6-month intervals (Figure 1 and Figure 2).
4.2. Histologic Study
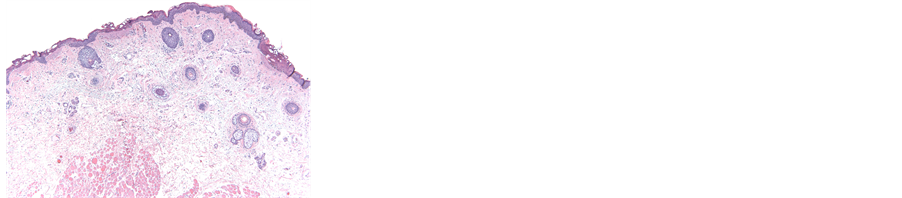
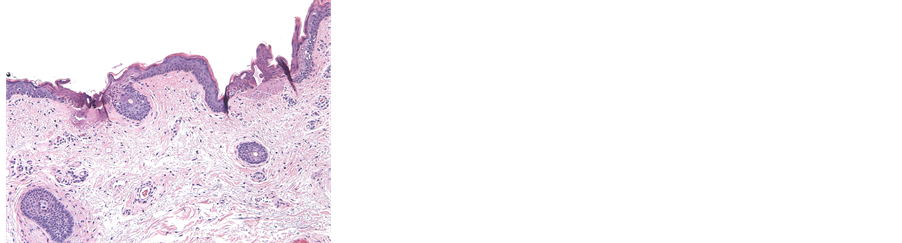
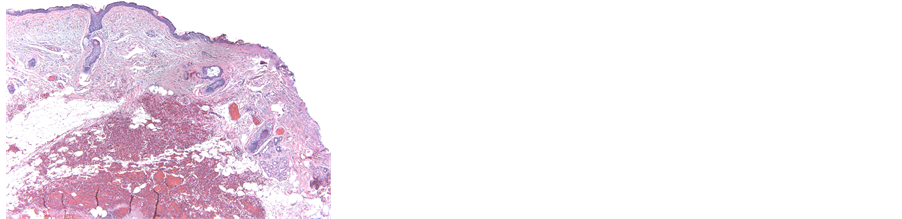
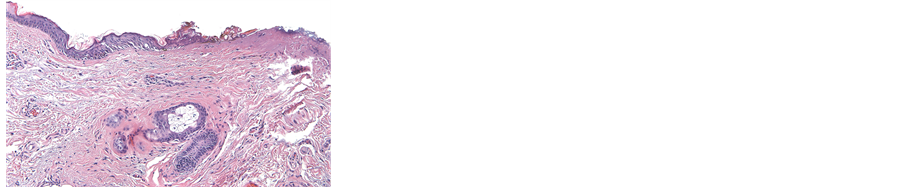
Examination of H & E stained sections 40× (Figure 3) and 100× (Figure 4) magnifications of original specimen revealed uniform diathermy at a depth of 0.05 mm for area resurfaced. For the area next to the excision wound, a uniform depth of 0.15 mm of diathermy was noted at 40× (Figure 5) and 100× (Figure 6).
Figure 1. Pre-op photograph of patient before laser resurfacing of lower lids. Note fine static rhytids in lower lids.
Figure 2. Post-op photograph of patient at 2 months after laser resurfacing. Note improvement of lower lid rhytids and no evidence of post inflammatory hyperpigmentation.
Figure 3. H & E stain histologic section at 40× magnification. Note uniform diathermy at a depth of 0.05 mm for area resurfaced.
Figure 4. H & E stain histologic section at 100× magnification. Note uniform diathermy at a depth of 0.05 mm for area resurfaced.
Figure 5. H & E stain histologic section at 40× magnification. Note uniform depth of 0.15 mm of diathermy in the area next to the edge of the excised wound using continuous wave mode.
Figure 6. H & E stain histologic section at 100× magnification. Note uniform depth of 0.15 mm of diathermy in the area next to the edge of the excised wound using continuous wave mode.
5. Discussion
It is well documented in medical literature that PIH is the most common side effect following traditional ablative laser resurfacing across all skin types [5] , with a higher percentage occurring in darker-skinned patients [6] [7] .
Treating patients with fractional laser resurfacing (whether ablative or non-ablative) has been shown to reduce (although not eliminate) the incidence of PIH because of the relatively low treatment density on tissue [8] [9] .
Using an ablative CO2 fractional laser (with a new scanning handpiece that uses a patented scanning algorithm) on patients with Fitzpatrick skin types 4 - 5, the incidence of PIH was eliminated. This mathematical algorithm is designed to place laser spots in a non-sequential Z-shaped pattern, thereby providing the longest possible time between adjacent spots (during any particular scan time), while still filling in a given area of tissue. This allows for maximum tissue cooling due to minimal heat buildup between adjacent spots.
Bulk tissue heating during laser resurfacing is documented as the leading determining factor in the increased incidence of PIH [9] [10] . However, when performing CO2 laser fractional ablative resurfacing, it is possible to eliminate or significantly reduce postoperative hyperpigmentation through use of a new scanning handpiece designed to lower bulk thermal injury to tissue.
The authors developed a technique using loupes during the procedure to enable accurate assessment of the depth of ablative resurfacing. In addition to this depth control, the technique also stacks pulses within the square- shaped resurfacing area; this maneuver provides an additional time gap between each pass, thus allowing dissipation of bulk thermal accumulation within tissue after each pass. The histologic study confirms these findings. The uniform depth of 0.05 mm of thermal injury within the resurfaced area, as compared with 0.15 mm of thermal injury at the skin edged excised in continuous wave mode, showed that stacking of scanned pulses was accurate enough to provide consistent depth ablation and yet only minimal thermal injury occurred when compared to the use of laser in continuous wave mode. This result was achieved with the use of magnifying loupes and the inherent thermal-spacing characteristic of the scanning algorithm provided by the laser device.
Financial Disclosure
The authors have no financial disclosure and no financial interest in any of the products mentioned in this paper.
References
- (2000) Projections of the Resident Population by Race, Hispanic Origin, and Nativity: Middle Series, 2006 to 2010. Populations Projections Program, Population Division, US Census Bureau, Washington DC.
- Gilchrest, B.A. (1989) Skin Aging and Photoaging: An Overview. Journal of the American Academy of Dermatology, 21, 610-613. http://dx.doi.org/10.1016/S0190-9622(89)70227-9
- Goh, S.H. (1990) The Treatment of Visible Signs of Senescence: The Asian Experience. British Journal of Dermatology, 122, 105-109. http://dx.doi.org/10.1111/j.1365-2133.1990.tb16134.x
- Pham, R.T. (1998) Hyperpigmentation in Asians after Carbon Dioxide Laser Resurfacing. Journal of Dermatologic Surgery, 29, 118.
- Nanni, C.A. and Alster, T.S. (1998) Complications of Carbon Dioxide Laser Resurfacing: An Evaluation of 500 Patients. Washington Institute of Dermatologic Laser Surgery, Washington DC. Journal of Dermatologic Surgery, 24, 315-320.
- Goldberg, D. (2004) Complications in Cutaneous Laser Surgery. Taylor & Francis Group, UK, 29.
- Sriprachya-Anunt, S., Marchell, N., Fitzpatrick, R., et al. (2002) Facial Resurfacing in Patients with Fitzpatrick Skin Type IV. Lasers in Surgery and Medicine, 30, 86-92. http://dx.doi.org/10.1002/lsm.10012
- Gold, M. (2009) Aesthetic Update, Fractional Laser Technology. The Journal of Clinical and Aesthetic Dermatology (JCAD). http://www.jcadonline.com/2217/aesthetic-update-update-on-fractional-laser-technology
- Chan, H.L., Manstein, D., Yu, C.S., et al. (2007) The Prevalence and Risk Factors of Post-Inflammatory Hyperpigmentation after Fractional Resurfacing in Asians. Lasers in Surgery and Medicine, 39, 381-385. http://dx.doi.org/10.1002/lsm.20512
- Rahman, Z., Alam, M. and Dover, J.S. (2006) Fractional Laser Treatment for Pigmentation and Texture Improvement. Skin Therapy Letter, 11, 9. http://www.skintherapyletter.com/2006/11.9/2.html