World Journal of Cardiovascular Diseases
Vol.05 No.02(2015), Article ID:53853,4 pages
10.4236/wjcd.2015.52004
Celiac Artery Aneurysm Due to Chronic Spontaneous Dissection: Two Cases of Surgical Repair
Daisuke Fukui*, Yuko Wada, Yoshinori Ohtsu, Kazunori Komatsu, Noburo Ohashi, Ko Nakahara, Toshihito Gomibuchi, Tatsuichiro Seto, Kenji Okada
Division of Cardiovascular Surgery, Department of Surgery, Shinshu University School of Medicine, Matsumoto, Japan
Email: *dfukui@shinshu-u.ac.jp
Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 7 January 2015; accepted 29 January 2015; published 6 February 2015
ABSTRACT
In this report, we describe two surgical cases of celiac artery aneurysm due to chronic and asymptomatic spontaneous dissection without atherosclerotic change or medial degeneration. Case 1 had replacement of the celiac and common hepatic arteries using a knitted Dacron prosthetic graft, and case 2 had simple aneurysmectomy. The incidence of celiac artery dissection is increasing lately, but subsequent aneurysm is relatively rare. Our two cases had no atherosclerotic risk factors, so it might be possible that celiac artery aneurysm due to spontaneous dissection may produce different findings from dissection of other arteries. We consider that the need for surgery should be determined carefully if the asymptomatic celiac artery aneurysm due to dissection is small and unless it shows any changes in its diameter in the follow-up period.
Keywords:
Celiac Artery Aneurysm, Spontaneous Dissection, Surgical Repair

1. Introduction
Spontaneous dissection of a visceral artery is classically reported to be diagnosed after fatal hemorrhage or ischemia. Lately it is not so rare due to increasing use of imaging for various intraabdominal pathophysiologies. But its mechanism is still unknown.
Before 2000, there were only five reports in the literature of celiac artery aneurysm due to spontaneous dissection [1] -[5] , but to date there have been less than 30 reported cases [6] - [12] . In this report, we describe two surgical cases of celiac artery aneurysm due to chronic and asymptomatic spontaneous dissection without atherosclerotic change or medial degeneration.
2. Case Reports
2.1. Case 1
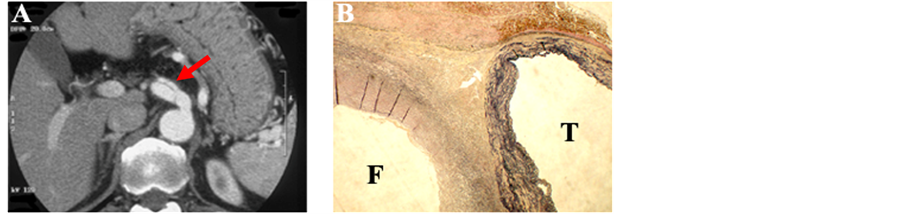
A 68-year-old man was found to have celiac artery aneurysm with spontaneous dissection by computed tomography (CT) three years after surgery for rectal cancer. He had no risk factors for cardiovascular disease and there were no iatrogenic reasons for celiac artery aneurysm. Enhanced CT revealed celiac artery aneurysm with dissection, which was 12 mm in diameter. No dissection of the aorta around celiac axis was observed. After a period of one year, we performed an operation, because the aneurysmal diameter changed to 15 mm (Figure 1(A)). After an upper abdominal median skin incision and open laparotomy, we dissected the lesser omentum and approached the celiac artery aneurysm. From its outward appearance the aneurysm was not apparently dissecting due to the thickness of the aneurysm wall. A test clamp of the orifice of the celiac artery caused weak pulsation of the hepatic and splenic arteries. After aneurysmectomy, replacement of the celiac and common hepatic arteries was performed using a knitted Dacron prosthetic graft, and the splenic artery was then reconstructed end-to-side to the graft. The left gastric artery was ligated and the dorsal pancreatic artery was sacrificed for reconstruction of the splenic artery. Macroscopic observation of the resected specimen revealed that the common hepatic artery branched from the true lumen and the splenic artery from the false lumen, respectively. Microscopic examination demonstrated dissection of the celiac artery, with the cleavage plane located in the elastic layer which was thick with chronic change (Figure 1(B)). There was no atherosclerotic change or throm- bosis. The patient’s postoperative recovery was uneventful without liver dysfunction, and he was discharged 14 days after the operation. Postoperatively, the patient is in good health and the bypass graft is patent.
2.2. Case 2
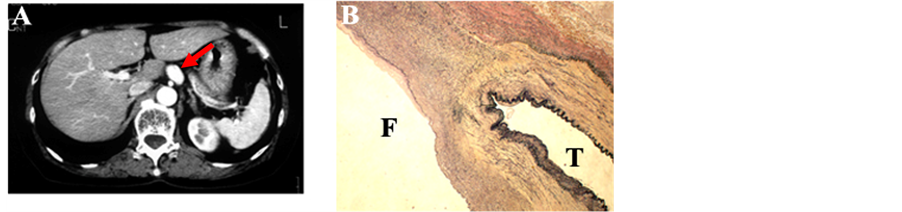
A celiac artery aneurysm was observed incidentally in a 65-year-old woman by abdominal echography during health screening. She had no risk factors for cardiovascular disease. Enhanced CT and aortography revealed a celiac artery aneurysm, which was 18mm in diameter (Figure 2(A)). And no dissection of the aorta around celiac axis was observed. Surgery was performed under patient’s informed choice. After laparotomy, we dissected the lesser omentum and approached the celiac artery aneurysm. The outward appearance of the aneurysm did not suggest dissection with chronic change. A test clamp of the celiac, common hepatic and splenic arteries caused only minor changes in the pulsation of the latter two. Therefore, we performed simple aneurysmectomy. The collateral circulation through the gastroduodenal and dorsal pancreatic arteries was preserved. Pathologic examination revealed that the common hepatic artery branched from the true lumen, and the splenic artery from the false lumen, respectively. Dissection of the celiac artery was demonstrated by histology with the cleavage plane located in the elastic layer which was thick with chronic change (Figure 2(B)). Little atherosclerotic or degenerative change was observed. The patient’s postoperative recovery was uneventful with resumption of normal alimentation. She was discharged 18 days after the operation, and postoperative course is well.
Figure 1. Case 1. (A) Abdominal CT with contrast injection showing celiac artery aneurysm with dissection 15 mm in diameter; (B) Transverse section of the celiac artery at low magnification (Weigert staining revealing elastic fibers). The cleavage plane is located in the elastic layer which is thick with chronic change. T, True lumen; F, False lumen; (×10).
Figure 2. Case 2. (A) Abdominal CT with contrast injection showing an aneurysm of the celiac artery 18 mm in diameter. The presence of dissection is unclear; (B) Transverse section of the celiac artery at low magnification (Weigert staining revealing elastic fibers). The cleavage plane is located in the elastic layer which is thick with chronic change. T, True lumen; F, False lumen; (×10).
3. Discussion
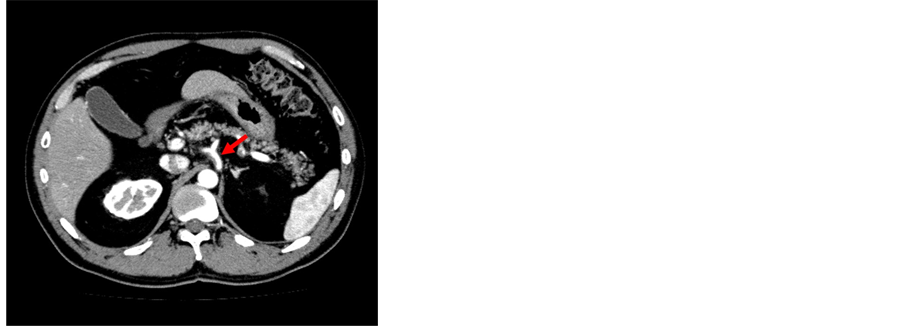
Unlike aortic dissection, which is relatively common, spontaneous dissection of arteries unrelated to the aorta has been considered to be rare. But lately it is not so rare due to increased use of imaging for various intraabdominal pathophysiologies. Symptomatic arterial dissection is classically identified by acute ischemia [13] or hemorrhage [2] . So careful medical follow up is considered to be important, but more than half of all arterial dissections are asymptomatic [5] [13] . The cases reported in the literature have involved the renal, coronary, intracranial and visceral arteries, in order of incidence [13] . In the visceral arteries, the most frequent site of arterial dissection is the superior mesenteric artery [14] . Dissection of the celiac artery and its branches, such as the hepatic, splenic and gastroduodenal artery is rarer than that of the superior mesenteric artery. Generally, celiac artery aneurysms comprise approximately 4% of all visceral artery aneurysms [15] . Hypertension is the most common clinical risk factor associated with arterial dissection, but our two cases had no atherosclerotic risk factors and no atherosclerotic change of the aneurysm wall on pathological examination. So it might be possible that dissection of the celiac artery may produce different findings from dissection of other arteries. For example, we experienced 46-year-old man, complaining transient epigastric pain due to acute thrombosed spontaneous dissection of celiac artery two years ago (Figure 3). And he had hypertension as atherosclerotic risk factor.
The most common pathological findings of true arterial aneurysm are medial degeneration and atherosclerosis [15] . Arterial dissection is defined as intimomedial entry tear with blood surging between the arterial layers [13] . In our cases there was arterial dissection of the media with chronic changes, and no atherosclerotic change or degeneration.
Surgery is usually recommended for true celiac artery aneurysm because nearly 80% of all reported cases have ruptured and endovascular therapy for visceral arteries has not established yet. However, Graham et al. reported that in their experience the risk of rupture was only 13% [16] . Surgery has also been recommended for arterial aneurysm due to dissection in previous reports. In both of the present cases, the wall of the false lumen was thick due to chronic change. Similarly to DeBakey IIIb type aortic dissection, surgery should be considered carefully if celiac artery aneurysm due to dissection is small and asymptomatic, and reveals no change in its diameter in the follow-up period. For most DeBakey IIIb-type aortic dissections which extend to the celiac arteries, conservative therapy might generally be chosen. Matsuo et al. reported a case where thrombosed celiac arteryaneurysm due to dissection was observed without any intervention [5] . Surgery or transcatheter embolisation was conducted for most of remaining reported case. Indication for the treatment depends on the patient’s situation and the timing for intervention should be considered under a comprehensive assessment for the risk of rupture.
If abundant collateral circulation is confirmed with an intraoperativetest clamp of the celiac artery, reconstruction of the celiac, common hepatic or splenic arteries is not necessary, and the collateral arterial branches should be preserved. Reconstruction of these arteries should be performed if the intraoperative findings suggest any possibility of hepatic or splenic ischemia, as the indication for reconstruction of the celiac artery, as with stump pressure of the hepatic artery and splenic artery, is not clearly defined.
4. Conclusion
We have reported two surgical cases of celiac artery aneurysm due to chronic spontaneous dissection. The pa-
Figure 3. Abdominal CT with contrast injection showing an acute thrombosed spontaneous dissection of celiac artery.
tients were asymptomatic and had no thrombosis, atherosclerotic change. The incidence of celiac artery dissection is increasing lately, and we consider that the surgical indication for aneurysmal change should be determined carefully if the asymptomatic celiac artery aneurysm due to dissection is small and unless it shows any changes in its diameter in the follow-up period.
References
- Bret, P.M., Partensky, C., Bretagnolle, M., Paliard, P. and Burke, M. (1987) Obstructive Jaundice by a Dissecting Aneurysm of Celiac Axis and Hepatic Artery. Digestive Diseases and Sciences, 32, 1431-1434. http://dx.doi.org/10.1007/BF01296672
- Bartoli, J.M., Moulin, G., Di Stefano, D., Rudondy, P., Gerolami, A. and Kasbarian, M. (1990) Isolated Dissection of the Celiac Trunk and Its Branches. X-Ray Computed Tomography and Angiography Findings. A Case Report. Annales de Radiologie, 33, 264-266.
- Takeda, H., Matsunaga, N., Sakamoto, I., Obata, S., Nakamura, S. and Hayashi, K. (1995) Spontaneous Dissection of the Celiac and Hepatic Arteries Treated by Transcatheter Embolization. American Journal of Roentgenology, 165, 1288-1289. http://dx.doi.org/10.2214/ajr.165.5.7572520
- Chaillou, P., Moussu, P., Noel, S.F., Sagan, C., Pistorius, M.A., Langlard, J.M., et al. (1997) Spontaneous Dissection of the Celiac Artery. Annals of Vascular Surgery, 11, 413-415. http://dx.doi.org/10.1007/s100169900070
- Matsuo, R., Ohta, Y., Ohya, Y., Kitazono, T., Irie, H., Shikata, T., et al. (2000) Isolated Dissection of the Celiac Artery―A Case Report. Angiology, 51, 603-607. http://dx.doi.org/10.1177/000331970005100710
- D’Ambrosio, N., Friedman, B., Siegel, D., Katz, D., Newatia, A. and Hines, J. (2007) Spontaneous Isolated Dissection of the Celiac Artery: CT Findings in Adults. American Journal of Roentgenology, 188, W506-W511.
- Takayama, T., Miyata, T., Shirakawa, M. and Nagawa, H. (2008) Isolatedspontaneous Dissection of the Splanchnic Arteries. Journal of Vascular Surgery, 48, 329-333. http://dx.doi.org/10.2214/AJR.06.0315
- Obon-Dent, M., Shabaneh, B., Dougherty, K.G. and Strickman, N.E. (2012) Spontaneous Celiac Artery Dissection Case Report and Literature Review. Texas Heart Institute Journal, 39, 703-706. http://dx.doi.org/10.1016/j.jvs.2008.03.002
- Jung, S.C., Lee, W., Park, E.A., Jae, H.J., Chung, J.W. and Park, J.H. (2013) Spontaneous Dissection of the Splanchnic Arteries: CT Findings, Treatment, and Outcome. American Journal of Roentgenology, 200, 219-225. http://dx.doi.org/10.2214/AJR.11.7877
- Mousa, A.Y., Coyle, B.W., Affuso, J., Haser, P.B., Vogell, T.R. and Graham, A.M. (2009) Nonoperative Management of Isolated Celiac and Superior Mesenteric Artery Dissection: Case Report and Review of Literature. Vascular, 17, 359-364. http://dx.doi.org/10.2310/6670.2009.00053
- Glehen, O., Feugier, P., Aleksic, Y., Delannoy, P. and Chevalier, J.M. (2001) Spontaneous Dissection of the Celiac Artery. Annals of Vascular Surgery, 15, 687-692. http://dx.doi.org/10.1007/s10016-001-0012-0
- Batt, M. and Baque, J. (2011) Successful Percutaneous Embolisation of a Symptomatic Celiac Artery Dissection with Aneurysm Dilation with Detachable Vascular Plugs. Journal of Vascular Surgery, 54, 1812-1815. http://dx.doi.org/10.1016/j.jvs.2011.05.016
- Foord, A.G. and Lewis, R.D. (1959) Primary Dissecting Aneurysms of Peripheral and Pulmonary Arteries. Archives of Pathology, 68, 553-577.
- Iha, K., Nakasone, Y., Nakachi, H., Horikawa, Y., Gushiken, M. and Matsuda, H. (2000) Surgical Treatment of Spontaneous Dissection of the Superior Mesenteric Artery: A Case Report. Annals of Thoracic and Cardiovascular Surgery, 6, 65-69.
- Lakin, R.O. and Kashyap, V.S. (2000) Splanchnic Artery Aneurysms. In: Rutherford, R.B., Ed., Vascular Surgery, 8th Editions, WB Saunders Co., Philadelphia, 2220-2235.
- Graham, L.M., Stanley, J.C., Whitehouse Jr, W.M., Zelenock, G.B., Wakefield, T.W., Cronenwett, J.L., et al. (1985) Celiac Artery Aneurysms: Historic (1745-1949) versus Contemporary (1950-1984) Differences in Etiology and Clinical Importance. Journal of Vascular Surgery, 2, 757-764. http://dx.doi.org/10.1016/0741-5214(85)90053-9
NOTES
*Corresponding author.