Open Journal of Stomatology
Vol.4 No.5(2014), Article ID:45601,5 pages DOI:10.4236/ojst.2014.45032
Intrabony Schwannoma of the Mandible: Case Report and Review of Literature
Abdeljalil Abouchadi¹, Alae Guerrouani1*, Yasmina Ribag¹, Karim El Khatib¹, Mohamed Nassih²
¹Department of Plastic and Maxillofacial Surgery, Military Hospital, Rabat, Morocco
²Department of Plastic and Maxillofacial Surgery, School of Medicine, University of Rabat, Rabat, Morocco
Email: *alaeguerrouani@hotmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 11 March 2014; revised 15 April 2014; accepted 23 April 2014
ABSTRACT
This paper focuses on the case of intrabony mandibular schwannoma in a 39 yrs healthy male who was addressed by his dentist for an asymptomatic radiolucency of the left mandibular corpus. Computed Tomography Dentascan showed a soft tumour continuous to the path of the inferior alveolar nerve. Confirmation was made after surgical excision and careful histological examination. Radiolucent images of the mandible are frequently met by dentists and oro-facial surgeons, and suggest first odontogenic cysts because of their high frequency. But even if sheath nerve tumours are very rare, this case report reminds the necessity to keep them in mind.
Keywords:Neurilemmoma, Mandible, Nerve Sheath Neoplasms

1. Introduction
Schwannoma, also known as neurilemmoma or neurinoma, is a slow growing benign tumour taking its origin from the sheath of peripheral myelinited nerves, mostly sensitive nerves. The head and neck location seems to be affected in 24% - 48% with a predilection for soft tissues. Intraosseous schwannomas represent a rare condition since schwannomas represent less than 1% of primary benign bone tumours [1] [2] . Literature reports nearly 60 cases of true intrabony schwannomas of the jaw.
Here we present another case of intraosseous schwannoma of the mandible and review of literature.
2. Case Report
A 39-year-old male was referred by his dentist for a left mandibular radiolucent image without clinical complaint. The patient has no personal medical history. Physical examination found no dermatological or intraoral abnormalities. Panoramic x-ray (Figure 1) showed a unique multilocular radiolucent image sitting in the left mandibular corpus between the central incisor (tooth 31) and the first molar (tooth 36). A concurrent radiolucency appears as a cyst of the left mandibular first premolar root (tooth 34) without root erosion. Computed Tomography Dentascan was performed to study relations with the teeth roots and cortical bone. It showed a non agressive well defined lesion measuring 36 × 18 mm continuous to the path of the inferior alveolar nerve. We therefore suggested the hypothesis of a benign nerve sheath tumor as schwannoma or neurofibroma or an odontogenic cyst.
Surgical treatment was preceded by root canal treatment of all teeth from the left mandibular second premolar (35) to the left mandibular central incisor (31) included. The patient was aware of the risk of postsurgical anesthesia/paresthesia of the left lower lip. The surgical procedure was carried under general anesthesia. A sulcular vestibular incision was performed from the left mandibular first molar (36) to the right mandibular lateral incisor (42) with subsequent discharges. Osteotomy was carried using burs until good exposure of a well circumscribed yellowish-reddish tumor intimately bonded to the inferior alveolar nerve at its distal part (Figure 2 & Figure 3). Excision of the tumour was carried in toto from the nerve which was partially respected because of the difficult dissection due to the intimate attachment of the tumour.
Microscopic examination of the surgical specimen found an encapsulated tumour composed by connective tissue arranged in crossed fascicles and by fusiform cells with aligned long nuclei. The presence of Verocay bodies, and the positive immunohistochemistry staining for the S100 protein confirmed the diagnosis of schwannoma.
As an immediate complication of the surgical procedure, total anesthesia of the left lower lip was registered. An improvement was noted during the first twelve months after surgery, but final anesthesia of the external half of the left lower lip persists.
3. Discussion
First described by Verocay in early twentieth century, schwannoma is supposed to derive from Schwann cells of the peripheral nerve sheath. Three mechanisms by which schwannomas involve bone were described: a) They may arise centrally within bone, b) they may arise within the nutrient canal and produce canal enlargement as we see in this case, or c) a soft tissue ou periosteal tumour may cause erosion or penetration into bone [3] .
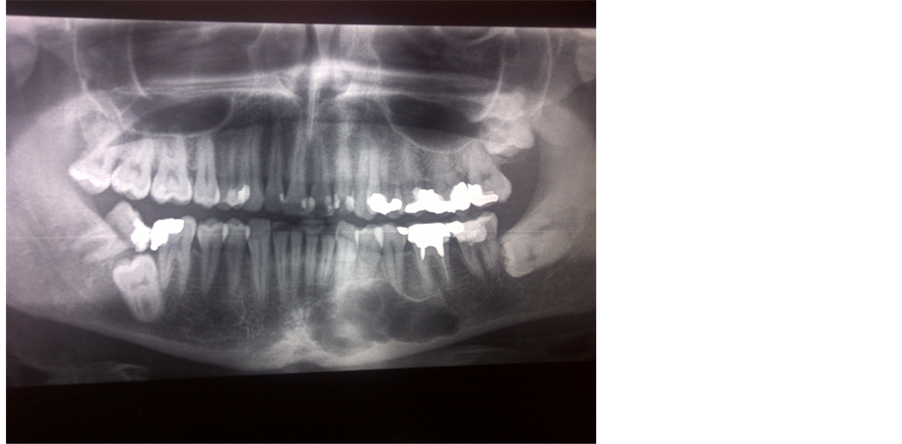
Figure 1. Panoramic x-ray: Multilocular radiolucent image of the left mandibular corpus and concurrent cyst of tooth 34.
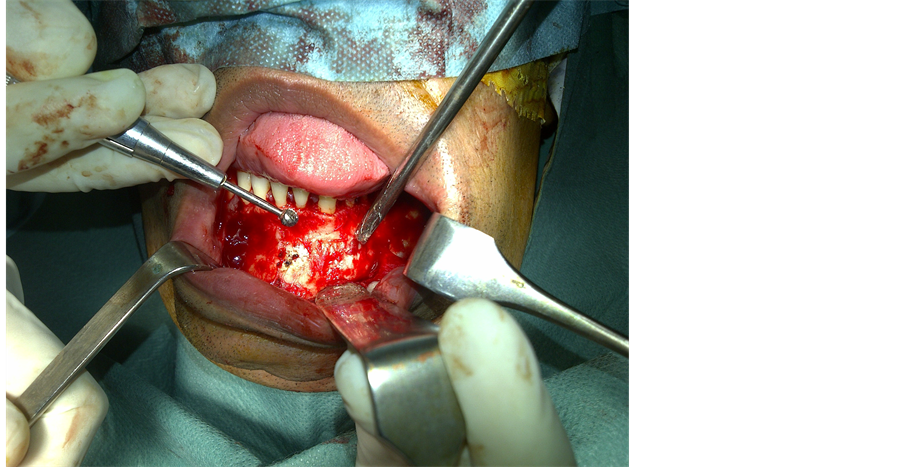
Figure 2. Per operative view: External corticotomy of the left mandibular corpus.
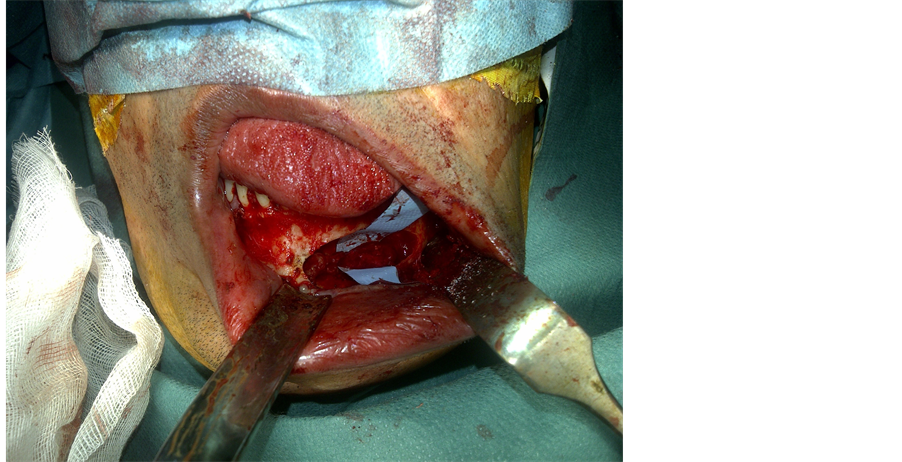
Figure 3. Per operative view: The nerve sheath tumour before nerve dissection.
Schwannoma development is mostly asymptomatic. This benign slow-growing tumour may be present for some years before declaring any symptom as swelling, pain or sensitive disorder as lower lip numbness. Females are more often concerned than males [4] . Literature records report an age range between 3- and 86-year-old. It seems that mandible is more often involved due to the length of the inferior alveolar canal through the mandibular bone [5] . Literature data note a marked predilection of schwannomas for the posterior part of the mandible [1] .
Since the clinical presentation is often unspecific or completely absent, schwannoma of the mandible is often a radiological discovery during a mandibular x-ray for dental care. The radiographic appearance is often a well-defined unilocular non specific radiolucent image with root divergence and root resorption only in teeth contacting the lesion [6] . Panoramic x-ray of our patient showed a multilocular aspect and a concurrent image of an inflammatory dental cyst of the mandibular left first premolar root (tooth 34). This association is reported to be very rare [4] . We therefore evoked : an odontogenic tumour or a fibrosseous lesion. Computed tomography showed a tumour connected to the mandibular canal which was enlarged and allowed us to suggest a nerve sheath tumour even if their occurrence is infrequent.
The diagnosis of schwannoma is made by histological analysis and specific immunohistochemistry staining. The histological features of intraosseous and soft tissue schwannomas are identical [2] . Histological examination establishes the benign nature of the tumor. The essential features of a conventional schwannoma include: a) exclusive composition of Schwann cells, b) arrangement of cells in a compact, often palisade fashion (Antoni A tissue), and occasionally, in a loose texture in which multiple processes are evident (Antoni B tissue), c) Verocay bodies, d) presence of hyalinized and/or ecstatic vessels, often accompanied by hemosiderin deposits, and e) encapsulation of affected fascicles by residual collagenous perineurium [3] . Immunochemistry is focalized on the S100 protein staining which is generally positive for cells of neural crest origin like schwannoma and neurofibroma. It is important that histological examination differentiate between neurofibroma and schwannoma since schwannoma presents less risk of recurrence after surgery. Encapsulation helps to differentiate between these entities. Schwannoma is always encapsulated. In contrast, only 4% of neurofibromas are encapsulated [7] .
Surgery is the only treatment we can propose for this condition. Even if a consensual treatment isn’t yet established, enucleation is recommended since schwannomas are well encapsulated tumours. Wide excision isn’t recommended since recurrence is rare. If happened, recurrence could be linked to an incomplete tumour removal [2] .
Patients should be well informed of the risk of post-operative anesthesia or paresthesia of a part of the lower lip before any surgical try. This condition can be very discomfortable and not well accepted by the patient. Malignant transformation of a schwannoma is a very rare condition, and such transformation has not been reported in an intrabony schwannoma [2] .
In the reported case, we have seen a rare location of intraosseous schwannoma born in the inferior alveolar nerve in the left part of the mandibular corpus. Imaging methods allowed us to evoke a lesion linked to the inferior alveolar nerve, even if an ameloblastoma or another odontogenic lesion remained a probable differential diagnosis, especially because of the presence of a concurrent radiolucent image linked to a small inflammatory dental cyst of the root of tooth 34. Histology examination found a well encapsulated tumour composed by fusiform cells, and the presence of Verocay bodies. Immunochemistry staining was strongly positive for S100 protein.
The surgical procedure was easily carried after the consent of the patient who was prepared to a possible deficiency of the left lower lip sensitivity. Outcome after 12 months was characterized by a partial recovery of the lip sensitivity and no recurrence. The patient is still regularly followed, no recurrence was observed 24 months after surgery.
4. Conclusions
Even if they are rare, nerve sheath tumours as schwannoma must be considered in asymptomatic cases with large radiolucent image of the jaw, even if clinical and x-ray examination suggest a dental origin. Treatment of schwannomas is based on limited surgery that should, as much as possible, respect the nerve.
Pathology should differentiate between schwannoma and neurofibroma which presents recurrences and imposes wide surgery. However, patients should be aware of the risk of a loss of sensibility of the half of lower lip, which is very uncomfortable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflict of Interest
The authors declare that they have no competing interests.
References
- Buric, N., Jovanovic, G., Pesic, Z., Krasic, D., Radovanovic, Z., Mihailovic, D., et al. (2009) Mandible Schwannoma (Neurilemmoma) Presenting as Periapical Lesion. Dentomaxillofacial Radiology, 38, 178-181. http://dx.doi.org/10.1259/dmfr/59344498
- Zhang, L., Xia, B.Q., Sun, H., Wang, L.Z., Zhao, Z.L., Li, B., et al. (2012) Intraosseous Schwannomas of the Jaws: 2 Case Reports and Review of the Literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 114, 13-17. http://dx.doi.org/10.1016/j.oooo.2011.09.026
- Santos, P.P., Freitas, V.S., Pinto, L.P., Freitas Rde, A. and de Souza, L.B. (2010) Clinicopathologic Analysis of 7 Cases of Oral Schwannoma and Review of the Literature. Annals of Diagnostic Pathology, 14, 235-239. http://dx.doi.org/10.1016/j.anndiagpath.2010.02.009
- Pimkhaokham, A., Piriyasupong, P., Swasdison, S., Pimkhaokham, S. and Tung, P. (2006) Central Neurilemmoma of the Jaw in Concurrence with Radicular Cyst: A Case Report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology, 102, 34-36. http://dx.doi.org/10.1016/j.tripleo.2006.01.025
- Kodani, I., Ueyama, Y., Mori, T., Doi, R., Osaki, M., Kataoka, S., et al. (2003) Intraosseous Schwannoma of the Mandible. Asian Journal of Oral and Maxillofacial Surgery, 15, 64-67. http://dx.doi.org/10.1016/S0915-6992(03)80035-3
- De Lacerda, S.A., Brentegani, L.G., Rosa, A.L., Vespúcio, M.V. and Salata, L.A. (2006) Intraosseous Schwannoma of Mandibular Symphysis: Case Report. Brazilian Dental Journal, 17, 255-258. http://dx.doi.org/10.1590/S0103-64402006000300015
NOTES

*Corresponding author.

