Open Journal of Clinical Diagnostics
Vol.2 No.4(2012), Article ID:25251,4 pages DOI:10.4236/ojcd.2012.24014
Fatal pulmonary embolism after surgery for a clavicle fracture: A case report
![]()
1Department of Orthopaedic Surgery, Mejiro Hospital, Tokyo, Japan
2Department of Cardiology, Mejiro Hospital, Tokyo, Japan
3Department of Orthopaedic Surgery, Institute of Sasaki Foundation, Kyoundo Hospital, Tokyo, Japan
4Department of Orthopaedic Surgery, Juntendo University Nerima Hospital, Tokyo, Japan
Email: sobshogo@gmail.com
Received 21 September 2012; revised 22 October 2012; accepted 30 October 2012
Keywords: Pulmonary Embolism; Clavicle Fracture
ABSTRACT
Patients undergoing upper extremity surgery generally have a low risk of pulmonary embolism. We encountered a rare case of fatal pulmonary embolism after surgical treatment of a clavicle fracture. A 46- year-old man fell off the roof of his car and suffered fractures of the left clavicle, temporal bone and ribs, as well as cerebral and lung contusions. He was admitted to a local hospital, and was later transferred to our hospital for surgical treatment of the clavicle fracture at 6 days after injury. He had no dyspnea and was ambulant. On day 7 after the injury, open reduction and internal fixation of the clavicle fracture using a plate and screws were performed under general anesthesia. Although surgery was uneventful, the patient had bradycardia postoperatively that progressed to cardiopulmonary arrest, which required resuscitation and intubation. Spontaneous cardiac output was restored 10 minutes after cardiac arrest, but the GCS score was E1V1M2. Enhanced CT of the chest revealed a 15 mm defect in the right pulmonary artery, leading to a diagnosis of pulmonary embolism. Thrombolytic therapy was started immediately. However, the patient’s condition worsened and he died 20 days postoperatively. We suggest that use of mechanical and chemical thromboprophylaxis should be considered for clavicle surgery.
1. INTRODUCTION
Pulmonary embolism (PE) is a serious complication of orthopaedic surgery. It is generally believed that patients undergoing upper extremity surgery have a low risk of PE. However, we encountered a rare case of fatal PE after surgery for a clavicle fracture.
2. CASE REPORT
The patient was a 46-year-old man with a weight of 58 kg, height of 166 cm, and body mass index of 21 kg/m2. He did not smoke. He had a 10-year history of type 2 diabetes mellitus, which was being treated with an oral antidiabetic agent. He was not taking other medications. He had no symptoms of deep vein thrombosis (DVT) or other vascular disease. There were no known thromboembolic risk factors in his family.
The patient had accidentally fallen from the roof of a stationary vehicle. When the emergency services arrived, his GCS was E4V4M6 and his vital signs were stable. He was transported to a nearby hospital with fractures of the left clavicle, temporal bone and ribs, as well as cerebral and lung contusions (Figure 1). He was admitted into the ICU for monitoring and a CT scans of the head was obtained to assess his head injury. For 2 days, the patient was confined to bed and wore compression stockings. He was ambulant thereafter and was moved to the general ward at 4 days after the accident. He was transferred to our hospital for surgical treatment of the clavicle fracture at 6 days after injury. On admission, the patient had no dyspnea and was ambulant. Routine laboratory tests,

Figure 1. Preoperative X-ray.
electrocardiogram, chest radiograph and echocardiography revealed no significant abnormalities.
Seven days after the accident, open reduction and internal fixation of the clavicle fracture was performed using a plate and screws, with the patient in the supine position under general anesthesia (Figure 2). No compression devices or stockings were used. The total operating time was 60 minutes and the duration of anesthesia was 115 minutes. The surgery was uneventful and normal vital signs were maintained during the operation.
His initial postoperative recovery was uneventful, and the patient was returned to the ward. However, bradycardia occurred after transfer from the recovery room, followed by cardiopulmonary arrest. Cardiopulmonary resuscitation was started immediately with intubation and administration of epinephrine. Spontaneous cardiac output was restored after 10 minutes, but the GCS score was E1V1M2. A chest radiograph showed similar findings to his preoperative film. Head CT did not reveal any new lesions. Enhanced chest CT revealed a 15 mm defect in the right pulmonary artery, suggesting a pulmonary embolus (Figure 3). No thrombus was found in the lower extremities. Thrombolytic therapy was started immediately, with heparin and urokinase being infused at 10 u/kg/h and 240,000 u/day, respectively. Although the doses were increased, head CT findings were suggestive of hypoxic cerebral damage. Repeat enhanced CT of the chest showed no change in the size of the thrombus. The patient’s condition subsequently worsened and he died at 20 days after surgery.
3. DISCUSSION
Deep venous thrombosis of the upper extremities is now believed to be more common than was previously realized. This condition is associated with anatomical abnormalities, use of central venous catheters, and transvenous cardiac pacing [1-3]. Upper extremity DVT can occur proximally in the subclavian, axillary, and brachial veins.
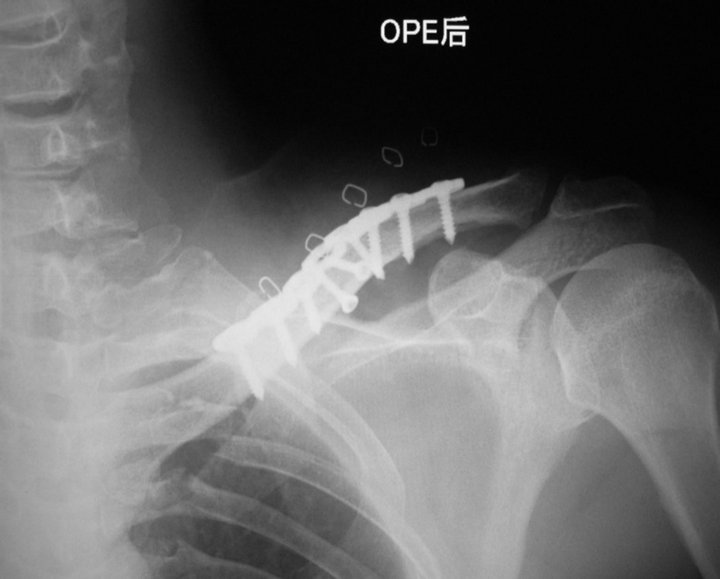
Figure 2. Postoperative X-ray.
In Japan, there have only been a few case reports of PE after upper extremity surgery, with only one case of fatal PE after upper extremity fracture being reported (Table 1). We did not consider thromboprophylaxis for upper extremity surgery. According to the Japanese Orthopaedic Association guideline on the prevention of PE and DVT, the risk of venous thromboembolism is low in patients having upper extremity surgery (Table 2).
Hingorani et al. [4] reported that the incidence of PE and the mortality rate were significantly higher in patients with upper extremity DVT compared to those with lower extremity DVT. The increase of upper extremity DVT was believed to be due to increasing use of central venous catheters for venous access in patients with cancer and other medical problems. Diabetes mellitus, obesity and a long operating time are associated with postoperative thromboembolic complications.
Our patient had type 2 diabetes mellitus, but was not obese, and his surgery did not exceed one hour in dura-
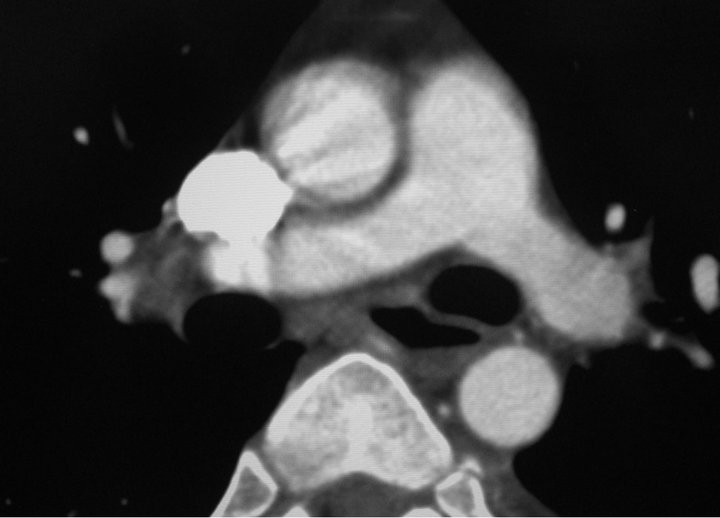
Figure 3. The enhanced chest CT revealed a 15 mm defect of contrast in the right pulmonary artery.

Table 1. Case reports of PE after U/E fracture surgery in Japan.
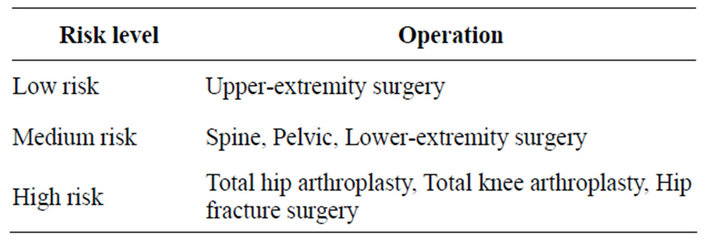
Table 2. The risk of VTE (The guideline on prevention of PE/DVT in Japan 2004).
tion. The presence of malignancy or a coagulation disorder was considered unlikely. Since the patient was ambulant, the use of elastic stockings, pneumatic compression devices on the lower extremities, and chemical prophylaxis was not considered.
Routine investigations to rule out thrombosis in patients undergoing surgery for upper extremity fractures are difficult in practice. We suggest that mechanical and chemical thromboprophylaxis should be considered for clavicle surgery. Early diagnosis and treatment of thrombosis can significantly reduce morbidity and mortality in this subset of patients and therefore must be considered very important.
REFERENCES
- Kim, S.J., Yoo, K.Y., et al. (2010) Fatal pulmonary embolism caused by thrombosis of contralateral axillary vein after arthroscopic right rotator cuff repair. Korean Journal of Anesthesiology, 59, S172-S175. doi:10.4097/kjae.2010.59.S.S172
- Monreal, M., Lafoz, E., Ruiz, J., et al. (1991) Upperextremity deep venous thrombosis and pulmonary embolism. A prospective study. CHEST, 99, 279-284. doi:10.1378/chest.99.2.280
- Prandoni, P., Polistena, P. Bernardi, E., et al. (1997) Upper-extremity deep vein thrombosis. Archives of International Medicine, 157, 57-62. doi:10.1001/archinte.1997.00440220061008
- Hingorani, A., Ascher, E., Hanson, J., et al. (1997) Upper Extremity versus lower extremity deep venous thrombosis. The American Journal of Surgery, 174, 214-217. doi:10.1016/S0002-9610(97)00088-3
- Janssen, R.P.A. and Sala, H.A.G.M. (2007) Fatal pulmonary embolism after anterior cruciate ligament reconstruction. The American Journal of Sports Medicine, 35, 1000- 1002. doi:10.1177/0363546506298581
- Teramoto, H., et al. (2004) A case of post operative pulmonary embolism associated with humeral surgical neck fracture. Central Japan Journal of Orthopaedic Surgery & Traumatology, 47, 807-808.
- Takizawa, T., et al. (2006) Pulmonary embolism after surgical treatment of Galeazzi fracture dislocation. A case report. Central Japan Journal of Orthopaedic Surgery & Traumatology, 49, 303-304.
- Satoshi S. (2007) A case report of death by pulmonary embolism after finger fracture in 19 years old. Kossetsu, 29, 628-630.

