Open Journal of Nursing
Vol.3 No.8A(2013), Article ID:40489,4 pages DOI:10.4236/ojn.2013.38A001
The effects of EMLA cream on pain responses of preschoolers
![]()
1Department of Nursing, Eulji University Hospital, Daejeon, South Korea
2College of Nursing, Eulji University, Daejeon, South Korea
3The Research Institute of Nursing Science, College of Nursing, Seoul National University, Seoul, South Korea
4Department. of Surgery, College of Medicine, Eulji University, Daejeon, South Korea
Email: *ahanaya@eulji.ac.kr
Copyright © 2013 Se Na Ahn et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 5 September 2013; revised 5 October 2013; accepted 21 October 2013
Keywords: Venipuncture; EMLA Cream; Pain; Preschooler
ABSTRACT
The aim of present study was to assess the effects of a eutectic mixture of topical anesthetics (EMLA cream) on pain responses of preschoolers during venipuncture. The pain responses were reported by children, nurses, and the children’s mothers. The preand posttest-designed study, which included a non-equivalent control group, was carried out in a pediatric unit at E University Hospital in South Korea. Pain responses during venipuncture were measured by the self-reporting of the children using the Face Pain Rating Scale (FPRS), the Procedure Behavior Checklist by nurses (PBCL), the Visual Analog Scale (VAS) by mothers, in addition to measurements of the children’s pulse rate and level of oxygen saturation. EMLA cream was effective in decreasing the pain responses of the children as assessed by FPRS, PBCL, and VAS scores. However, pulse rate and level of oxygen saturation of the children during venipuncture were not significantly different between the two groups. EMLA cream could be a useful option for reducing pain in preschool children during invasive procedures.
1. INTRODUCTION
For children, admission to a hospital environment can cause anxiety and fear [1]. Moreover, invasive procedures such as blood collection, intravenous injection, lumbar puncture, or intramuscular injection are the most painful and tormenting experiences for children. Children’s fear of injection needles originates from physical pain; however, the fear of such pain makes children misunderstand the purpose of the injection and further increases their anxiety about hospitalization [2]. Particularly for preschoolers, their incomplete intellectual development causes more pain and fear of injection needles, because they do not fully understand the purpose of the injection, commonly associating it with a punishment for bad thoughts or behaviors [3]. In addition, it is difficult for preschoolers to accurately express the area and intensity of the pain or find the proper words to express their pain during invasive procedures. These limitations result in the improper management of pain in preschoolers during invasive procedures.
Painful situations related to intravenous injections in hospitalized children cause the same amount of anxiety and stress for their parents, who watch the entire process. Especially in Korea, where one of the parents resides with the hospitalized child, parents experience the same feelings of fear and anxiety during their children’s injection. Effective pain management reduces emotional disturbances caused by hospitalization among children and their parents; therefore, it is a significant evaluation index of the quality of nursing care. As a guardian of ill children, nurses in pediatric units must provide proper pain management during hospitalization; such management can only be initiated after accurately assessing the degree of pain of preschoolers during invasive procedures.
In Korea, several non-pharmacologically interventional studies using an animation movie, an automated doll, a storytelling movie, or a cellular phone [4-7] have been conducted to reduce pain during invasive procedures for preschoolers. In terms of pharmacological methods, a topical cream that consists of a eutectic mixture of topical anesthetics (EMLA: 2.5% lidocaine and 2.5% prilocaine) is the most frequently used treatment for dental treatments, vaccinations, emergency room visits, and pediatric renal biopsies among neonates, toddlers, and school aged children [8-11]. In this study, we investigated the effects of EMLA cream in alleviating pain during venipuncture among preschoolers. The degree of pain was measured by three different methods, including self-reporting, mothers’ reports, and nurses’ observations in addition to measurements of pulse rates (PR) and level of oxygen saturation (SpO2).
2. METHORDS AND MEASUREMENTS
The participants in this study were hospitalized children between the ages of 36 and 72 months and their mothers at the E University Hospital. The duration of the study was from July 2010 to November 2010. Included preschoolers were unable to fully communicate using words; had no mental retardation or mental illness; were without skin diseases in the area of the intravenous injection; and were accompanied by mothers who understood the purpose of study and signed the consent for study participation. In the experimental group, prior to the venipuncture process, 2 g EMLA cream was applied to a 5-cm region around the area of the intravenous injection using Tegaderm film (3M, USA) for 60 minutes. Venipuncture was conducted in a treatment room, and mothers accompanied their children during the entire process. A pulse oximeter was connected to the child’s finger on the opposite limb of the site of the intravenous injection. Venipuncture was conducted on visible vessels on the back of the hand using a 24-gauge angiocatheter (BD, USA). To maintain consistency throughout the study procedure, all venipunctures were conducted by the same researcher. During each venipuncture, the researcher’s assistant both observed and recorded the maximum PR, the minimum SpO2 level, and the child’s behaviors. After the venipuncture, the children and their mothers were asked to record the level of pain during the time of injection. A total of 23 pairs (child and mother) participated in the experiment, and 26 pairs who were admitted to the same unit after the study period composed the control group. In the control group, the same processes were performed, but no EMLA cream was applied. Before the initiation of the study, approval from the Institutional Review Board of E University Hospital was obtained.
A questionnaire was constructed to measure the pain reactions of children using various scales, including the Faces Pain Rating Scale (FPRS), the Procedure Behavior Check List (PBCL), the Visual Analogue Scale (VAS), and PR and SpO2 measurements. The FPRS is the scale developed by Wong and Baker [12], ranging from 0 to 5 with faces showing different degrees of pain. After each venipuncture, children were asked to pick up the face showing the degree of pain felt. The reliability and validity of the scale during its development were 0.74 and 0.60, respectively. The PBCL, developed by Lebaron and Zeltzer [13], was constructed with seven domains: muscle tension, screaming, crying, use of restraints, expression of pain, delaying with words, and physical restraints, with a 4-point range. Reliability was measured as 0.87 at the time its development and 0.94 in this study. The VAS, developed by Huskisson [14], was used to measure the pain of children perceived by their mothers. On a 100-mm horizontal line with 0 (no pain at all) on the left and 100 (most pain) on the right, the mothers were told to indicate the degree of pain experienced by their children during the intravenous injection. The length indicated by the mothers from 0 was converted into a score. Higher scores meant that the pain of children perceived by their mothers was severe. At the time of its development, the reliability of the VAS was 0.62. PR and SpO2 measured by a pulse oximeter (Mediana, Oxymax N-560) were used as indicators for physiological pain responses, since they are known for their general simplicity and validity for measuring acute, sharp pain [15]. Higher PR with lower SpO2 levels indicated greater degrees of pain.
3. RESULTS
Twenty-three pairs of children and their mothers were included in the experimental group compared to 26 pairs in the control group. The general characteristics of the participants and the differences in pain responses were analyzed using the χ2, Fisher’s exact, and the MannWhitney U tests. There were no significant differences in the general characteristics of the subjects between the two groups (Table 1). With the application of EMLA cream prior to the venipuncture procedure, children showed significantly lower pain scores as assessed by themselves, nurses, and their mothers. The FPRS scores by the children (p = 0.008), the PBCL pain behaviors by the nurses (p = 0.001), and the VAS scores by the mothers (p = 0.006) were significantly lower in the experimental group compared to those in the control group. However, the changes in the children’s PR (Table 2) and SpO2 were not significantly different between the two groups, although both PR and SpO2 of the experimental group were more stable during the time of the injections.
4. DISCUSSION
For hospitalized children, venipuncture is a treatment that cannot be avoided. The fear and anxiety toward pain during the venipuncture process not only delay the child’s procedure but also reduce the child’s trust of physicians. The present study was conducted to measure the effects of applying a topical anesthetic during venipuncture for preschoolers. Results showed that the degree of pain reported by children, nurses, and mothers in the
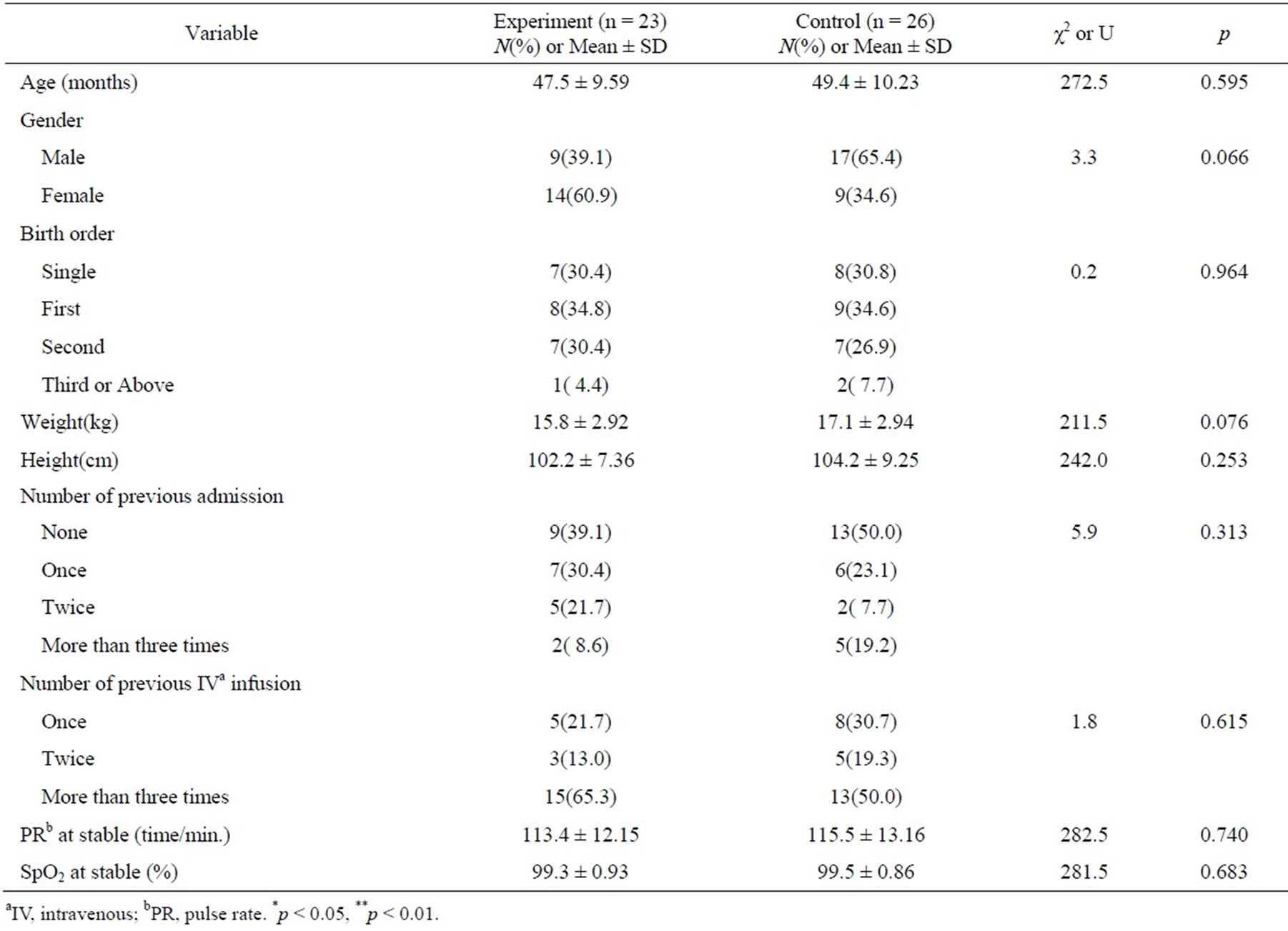
Table 1. General characteristics of the participants.
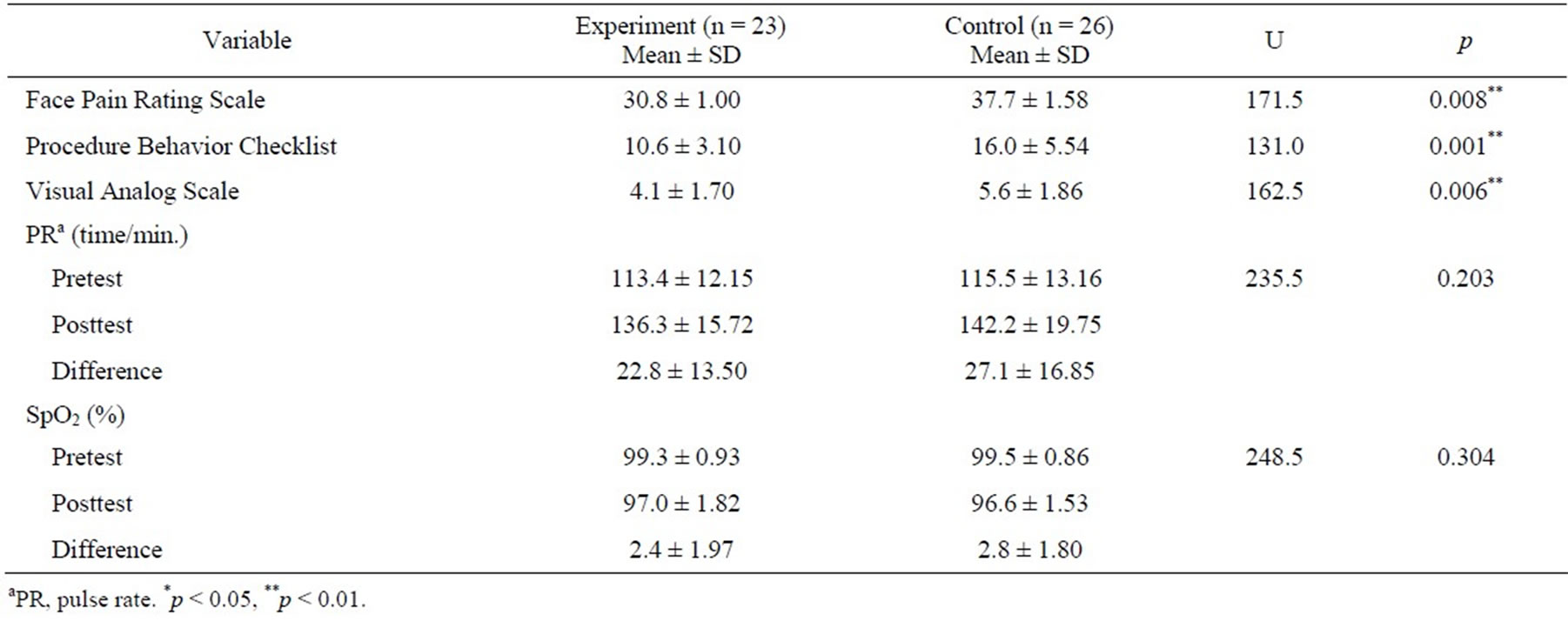
Table 2. Changes in pain responses.
experimental group was significantly lower than that in the control group. These findings are similar to those from previous studies of preterm infants, neonates, toddlers, and school-aged children [8-11,16-18], suggesting that the pain responses assessed by the child, the child’s mother, and nurses could be used as indicators of the effectiveness of pain relief, and the use of EMLA cream could be an effective pain reduction intervention for venipuncture in all children.
However, there are several limitations concerning the common usage of EMLA cream for venipuncture. Nurses in pediatric units must obtain a prescription from a pediatrician in every case. Nurses may occasionally misunderstand the side effects of EMLA cream. Additionally, although one study reported that it only takes 5 minutes for EMLA cream to be effective for pain relief in cases of venipuncture [19], it is commonly known that it usually takes 1 hour for EMLA cream to be effective [20]. In addition, unlike in adults, intravenous injection is much harder in children due to the smaller size of the vessels and a lack of cooperation. Therefore, even if the area of injection is previously selected and prepared with the application of a topical anesthetic, if the initial attempt fails, another area must be found, making it impossible to prepare the skin site with a topical anesthetic. Nevertheless, application of EMLA cream before venipuncture appears to be an effective method of pain relief for preschoolers. Various strategies to improve the usage of EMLA cream prior to venipuncture should be developed and implemented to enhance the quality of medical care for hospitalized children.
REFERENCES
- Duff, A. (2003) Incorporating psychological approaches into routine paediatric venipuncture. Archives of Disease in Childhood, 88, 931-937. http://dx.doi.org/10.1136/adc.88.10.931
- Bijttebier, P. and Vertommen, H. (1998) The impact of previous experience on children’s reactions to venipunctures. Journal of Health Psychology, 3, 39-46. http://dx.doi.org/10.1177/135910539800300103
- Carlson, K., Broome, M. and Vessey, J. (2000) Using distraction to reduce reported pain, fear, and behavioral distress in children and adolescents: A multisite study. Journal of the Society of Pediatric Nurses, 5, 75-85. http://dx.doi.org/10.1111/j.1744-6155.2000.tb00089.x
- Lim, O.W. and Cho, K.J. (2006) The effects of character distraction on intravenous injection pain of hospitalized preschooler. Journal of Korean Academy of Child Health Nursing, 12, 215-222.
- Lee, B.I. and Kwon, I.S. (2005) Effects of distraction using operating doll on preschool children’s pain during an IV catheter insertion. Journal of Korean Academy of Child Health Nursing, 11, 490-497.
- Koo, H.Y., Park, H.R. and Lim, J.H. (2007) Effects of distraction using balloon art on pain during intravenous injections in preschool children. Journal of Korean Academy of Child Health Nursing, 13, 66-72.
- Lim, J. and Shin, Y. (2007) Effects of distraction by a cellular phone on pain and fear during venipuncture procedure for hospitalized preschool children. Journal of Korean Academy of Child Health Nursing, 13, 506-511.
- Chung, Y., Park, K. and Kim, J. (2006) Effects of EMLA cream to decrease venipuncture related pain and anxiety in children. Journal of Korean Academy of Child Health Nursing, 12, 253-259.
- Kim, S., Shin, S. and Park, Y. (1994) The effect of the local anesthetic cream in alleviating pain from vaccinetion. Yeungnam University Journal of Medicine, 11, 270- 276.
- Ahn, J., Lee, K. and Park, Y. (1994) The effect of local anesthetic ointment (EMLA) for renal biopsy among children. Kidney Research and Clinical Practice, 13, 431.
- Kim, H., Ko, S., Hong, S., et al. (2002) The topical anesthesia with EMLA cream in children: A case report. Journal of the Korean Academy of Pediatric Dentistry, 29, 69-75.
- Wong, D. and Baker, C. (1988) Pain in children: Comparison of assessment scales. Pediatric Nursing Journal, 14, 9-17.
- Lebaron, S. and Zeltzer, L. (1984) Assessment of acute pain and anxiety in children and adolescents by self-reports, observer reports, and a behavior checklist. Journal of Consulting and Clinical Psychology, 52, 729-738.
- Huskisson, E. (1974) Measurement of pain. Lancet, 2, 1127-1131.
- Johnston, C. and Strada, M. (1986) Acute pain response in infant: A multidimensional description. Pain, 24, 373- 382.
- Nagengast, S. (1993) The use of EMLA cream to reduce and/or eliminate procedural pain in children. Journal of Pediatric Nursing, 8, 406-407
- Rogers, T. and Ostrow, C. (2004) The use of EMLA cream to decrease venipuncture pain in children. Journal of Pediatric Nursing, 19, 33-39. http://dx.doi.org/10.1016/j.pedn.2003.09.005
- Fan, H., Chen, H., Chen, S., et al. (2013) The effect of EMLA cream on minimizing pain during venipuncture in premature infants. Journal of Tropical Pediatrics, 59, 72-73. http://dx.doi.org/10.1093/tropej/fms040
- Dutta, S. (1999) Use of eutectic mixture of local anesthetics in children. Indian Journal of Pediatrics, 66, 707- 715.
- Britt, R.B. (2005) Using EMLA cream before venipuncture. Nursing, 35, 17.
NOTES
*Corresponding author.

