Open Journal of Obstetrics and Gynecology
Vol.4 No.3(2014), Article ID:43079,4 pages DOI:10.4236/ojog.2014.43018
Risk factors of intrapartal fetal death in a low-resource setting
![]()
1Department of Obstetrics and Gynecology, Faculty of Medicine and Biomedical Sciences (FMBS), The University of Yaoundé 1, Yaoundé, Cameroon
2Department of Obstetrics and Gynecology, Yaoundé Gyneco-Obstetric and Pediatric Hospital, Yaoundé, Cameroon
3Department of Pediatrics, Yaoundé Gyneco-Obstetric and Pediatric Hospital, Yaoundé, Cameroon
Email: *pfoumane2004@yahoo.fr
Copyright © 2014 Pascal Foumane et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Pascal Foumane et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 27 November 2013; revised 25 December 2013; accepted 3 January 2014
ABSTRACT
Objective: To identify the risk factors of intrapartal fetal death in a tertiary hospital in Yaoundé. Methods: It was a case-control study comparing 53 women who delivered with intrapartal fetal death to 106 women who delivered without intrapartal fetal death, carried out at the Yaoundé Gyneco-Obstetric and Pediatric Hospital, Cameroon. Results: The risk factors of intrapartal fetal death identified at bivariate analysis were: maternal age <20 years (OR = 3.1; CI = 1.1 - 8.3), absence of regular income (OR = 2.4; CI = 1.2 - 4.7), single motherhood (OR = 2.9; CI = 1.5 - 5.7), illiteracy and primary level of education (OR = 4.7; CI = 1.9 - 11.5), referral (OR = 5.0; CI = 2.5 - 9.9), parity 0 and 1 (OR = 2.3; CI = 1.1 - 4.5), no antenatal care (OR = 9.2; CI = 2.4 - 35.6), number of antenatal visits <4 (OR = 4.2; CI = 2.1 - 8.6), antenatal care in a health center (OR = 3.8; CI = 1.9 - 7.5), antenatal care by a midwife (OR = 2.5; CI = 1.3 - 4.9) or a nurse (OR = 5.2; CI = 1.4 - 18.7), absence of malaria prophylaxis (OR = 10.6; CI = 2.9 - 39.5), absence of obstetrical ultrasound (OR = 4.7; CI = 1.9 - 10.9), prematurity (OR = 3.4; CI = 1.5 - 7.3), abnormal presentation (OR = 2.6; CI = 1.1 - 5.9), ruptured membranes at admission (OR = 2.7; CI = 1.3 - 5.4), ruptured membranes >12 hours at admission (OR = 5.1; CI = 2.5 - 10.3), stained amniotic fluid (OR = 4.8; CI = 2.4 - 9.7), labor lasting more than 12 hours (OR = 18.1; CI = 8.0 - 41.0), presence of maternal complications (OR = 4.7; CI = 2.2 - 10.3), and presence of fetal complications (OR = 48.6; CI = 18.3 - 129), particularly acute fetal distress (OR = 52.3; CI = (14.6 - 186), cord prolapse (OR = 12.1; CI = 3.3 - 43.4), and birth weight <2500 g (OR = 2.8; CI = 1.2 - 6.6). Conclusion: Close attention should be offered to pregnant women, so as to identify these risk factors and promptly provide an appropriate management.
KEYWORDS
Risk Factors; Intrapartal Fetal Death; Intrapartum; Labor; Birth Outcome; Cameroon
1. INTRODUCTION
According to the World Health Organization [1], 8 out of every 1000 babies die during labor worldwide. In 2000, intrapartum mortality rate was estimated at 15 per 1000 births in Middle and Western Africa while it was only 0.6 per 1000 births in developed countries [1]. In Cameroon, a hospital-based study found an intrapartum mortality rate of 18 per 1000 births [2]. The same study identified antepartum hemorrhage, preeclampsia/eclampsia, secondary arrest of labor, fetal asphyxia and referral from another hospital as risk factors of intrapartal fetal death in Yaoundé. However, little is still known on the specific risk factors associated with intrapartal fetal death in Cameroon. The identification of these specific risk factors in our setting is an important step in reducing intrapartal fetal morbidity and mortality. The objective of this study was therefore to identify the risk factors of intrapartum fetal death in a sub-Saharan Africa setting.
2. MATERIALS AND METHODS
This case-control study involved 53 women who delivered with intrapartal fetal death and 106 women who delivered without intrapartal fetal death at the Yaoundé Gyneco-Obstetric and Pediatric Hospital, Cameroon. Women with fetal death occurring during labor (cases), from January 1st 2010 to December 31th 2012, were retrolectively recruited. The two next life births that followed an intrapartal fetal death were recruited as controls. Intrapartal fetal death was considered when a parturient was admitted with positive auscultation of fetal heart tones and gave birth to a dead baby (Apgar score = 0). After the approval of the study protocol by the ethical committee of the hospital, data was collected from the patients’ files and a pretested form was filled by an investigator. The variables studied were: maternal age, parity, socio-economic level, marital status, level of education, medical and surgical past history, gestational age at delivery, number of obstetrical ultrasound examinations in the current pregnancy, number of intrauterine fetuses, presence of pregnancy-related diseases, number of antenatal visits, place of antenatal care, grade of the antenatal care provider, intermittent preventive treatment of malaria, mode of admission for delivery, fetal presentation, membranes status at admission, interval between rupture of membranes and admission, color of amniotic fluid, mode of delivery, duration of labor, grade of the delivery care provider, presence of maternal complications, presence of fetal complications, fetal weight, fetal sex. The calculated minimal sample size was 46 subjects for each group and it was based on the 1.5% of intrapartal fetal mortality rate (15 per 1000 births) estimated by World Health Organization in Middle and Western Africa [1]. The chosen precision for statistical calculations was 5%. Statistical analysis was done using Epi info 3.5.3 and SPSS 17.0 software. The difference was statistically significant for P < 0.05. Pearson’s Chi square and Fisher’s exact test were used to compare proportions. Odds ratio (OR) and its 95% Confidence Interval (CI) were calculated to assess the association between the variables and intrapartal fetal death.
3. RESULTS
During the three years’ recruitment period, we recorded 78 deliveries with intrapartal fetal death and 7959 live births, giving an incidence of intrapartal fetal death of 0.93% (9.3 for 1000 live births) in our setting. Twentyfive files were excluded, due to missing data. Fifty-three women were therefore included in the case group and 106 controls were recruited for a chosen case-control ratio of 1/2.
The risk factors of intrapartal fetal death identified at bivariate analysis were (Table 1): maternal age <20
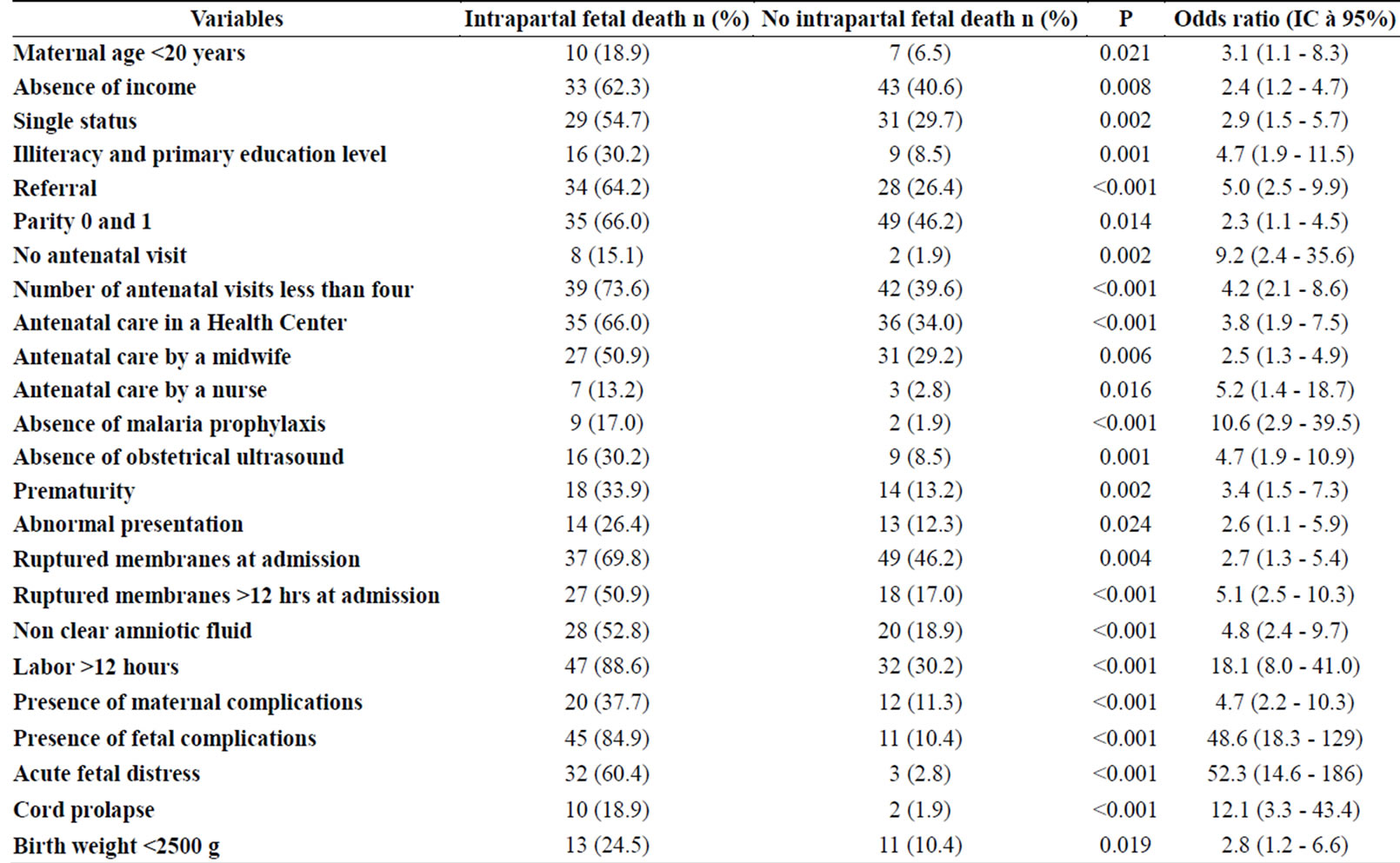
Table 1. Comparison of significant variables between the group with intrapartal fetal death (n = 53) and the group without intrapartal fetal death (n = 106).
years (P = 0.021; OR = 3.1; CI = 1.1 - 8.3), absence of regular income (P = 0.008; OR = 2.4; CI = 1.2 - 4.7), single motherhood (P = 0.002; OR = 2.9; CI = 1.5 - 5.7), illiteracy and primary level of education (P < 0.001; OR = 4.7; CI = 1.9 - 11.5), referral (P < 0.001; OR = 5.0; CI = 2.5 - 9.9), parity 0 and 1 (P = 0.014; OR = 2.3; CI = 1.1 - 4.5), no antenatal care (P = 0.002; OR = 9.2; CI = 2.4 - 35.6), number of antenatal visits < 4 (P < 0.001; OR = 4.2; CI = 2.1 - 8.6), antenatal care in a health center (P < 0.001; OR = 3.8; CI = 1.9 - 7.5), antenatal care by a midwife (P = 0.006; OR = 2.5; CI = 1.3 - 4.9) or a nurse (P = 0.016; OR = 5.2; CI = 1.4 - 18.7), absence of malaria prophylaxis (P < 0.001; OR = 10.6; CI = 2.9 - 39.5), absence of obstetrical ultrasound examination (P < 0.001; OR = 4.7; CI = 1.9 - 10.9), prematurity (P = 0.002; OR = 3.4; CI = 1.5 - 7.3), abnormal presentation (P = 0.024; OR = 2.6; CI = 1.1 - 5.9), ruptured membranes at admission (P = 0.004; OR = 2.7; CI = 1.3 - 5.4), ruptured membranes >12 hours at admission (P < 0.001; OR = 5.1; CI = 2.5 - 10.3), stained amniotic fluid (P < 0.001; OR = 4.8; CI = 2.4 - 9.7), labor lasting more than 12 hours (P < 0.001; OR = 18.1; CI = 8.0 - 41.0), presence of maternal complications (P < 0.001; OR = 4.7; CI = 2.2 - 10.3), and presence of fetal complications (P < 0.001; OR = 48.6; CI = 18.3 - 129), particularly acute fetal distress (P < 0.001; OR = 52.3; CI = (14.6 - 186), cord prolapse (P < 0.001; OR = 12.1; CI = 3.3 - 43.4), and birth weight < 2500 g (P = 0.019; OR = 2.8; CI = 1.2 - 6.6).
4. DISCUSSION
Young maternal age and low parity are found to be risk factors of intrapartal fetal death. In fact, the lack of reproductive experience is known to be associated with adverse pregnancy outcome [3,4]. Teenagers have been found to be associated with adverse pregnancy outcome with a risk of intrapartum fetal death decreasing as maternal age decreases [3]. Similar conclusions have also been made concerning parity [4].
The absence of regular income, low level of education and single motherhood were identified risk factors of intrapartal fetal death in this study. Low socioeconomic status and low level of education are major contributors to intrapartum fetal death, 99% of the 1.02 million worldwide intrapartum fetal deaths each year occurring in low and middle income countries [5]. The poor are at a higher risk and have the lowest coverage of skilled care at birth [5]. Improving the socioeconomic and educational levels of women in developing countries might be a strategy to reduce the rate of fetal death occurring during labor.
The absence of antenatal care, insufficient number of antenatal visits, antenatal care in a health center, antenatal care by a midwife or a nurse, absence of malaria prophylaxis, absence of obstetrical ultrasound examination are risk factors of intrapartal fetal death identified in this study and they are related to poor antenatal care. According to a published systematic review analyzing interventions to reduce intrapartum related fetal deaths, over three-quarters of intrapartum-related deaths occur in settings with weak health systems and 327,200 intrapartum-related neonatal deaths can be averted by providing comprehensive emergency obstetric care and emergency newborn care for births already occurring in health facilities [6]. In fact, a great number of women are followed and delivered in unequipped health centers which are usually clandestine, with personnel (mainly nurses) which is unskilled in essential emergency obstetric and neonatal care. Pregnant women are often referred to tertiary level hospitals, like our study setting, in case of labor complications with ruptured membranes. Much is still to be done to fight against poor antenatal and birth care in our setting, Yaoundé.
Prematurity, abnormal fetal presentation, ruptured membranes at admission, ruptured membranes more than 12 hours at admission, stained amniotic fluid, labor lasting more than 12 hours, presence of maternal complications, presence of fetal complications, acute fetal distress, cord prolapse, and birth weight less than 2500 grams are also identified risk factors of intrapartal fetal death in our study. Some of these factors are related to poor antenatal and/or poor obstetric care during labor. The available literature identified most of these as risk factors of intrapartal fetal death [6,7].
However, our results must be considered with some limitations. This was a retrolective data collection with missing data leading to the exclusion of 25 files. Also, logistic regression was not used during the analysis. These might account for some bias in our results.
5. CONCLUSIONS
Intrapartal fetal death is associated with specific risk factors in our setting. They are related to the lack of reproductive experience (young age and low parity), low socioeconomic and education levels (single status, low education level, absence of regular income), poor antenatal care and the occurrence of pregnancy or labor related complications.
Close attention should be paid to pregnant women by experienced and competent health care providers, so as to identify the risk factors of intrapartal fetal death stated by this work, and promptly consider an appropriate management.
DECLARATION OF INTEREST
The authors report no declaration of interest.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES
- WHO (2006) Neonatal and perinatal mortality, country, regional and global estimates. World Health Organization, Geneva. www.who.int/making_pregnancy_safer/en/b
- Sandjong T.I.D., Tebeu, P.M., Mbu, R.E., Mboudou, E., Guegang, G.E., Nkwabong, E., et al. (2009) Intrapartum fetal death in Cameroon: An assessment in two referral hosptals in Taoundé, Cameroon. Clinics in Mother and Child Health, 6, 1123-1127.
- Wilson, R.E., Alio, A.P., Kirby, R.S. and Salihu, H.M. (2008) Young maternal age and risk of intrapartum stillbirth. Archives of Gynecology and Obstetrics, 278, 231- 236. http://dx.doi.org/10.1007/s00404-007-0557-4
- Walsh, C.A., McMenamin, M.B., Foley, M.E., Daly, S.F., Robson, M.S. and Geary, M.P. (2008) Trends in intrapartum fetal death, 1979-2003. American Journal of Obstetrics and Gynecology, 198, e1-e7.
- Lawn, J.E., Lee, A.C., Kinney, M., Sibley, L., Carlo, W.A., Paul, V.K., et al. (2009) Two million intrapartumrelated stillbirths and neonatal deaths: Where, why, and what can be done? International Journal of Gynecology & Obstetrics, 107, S5-S19. http://dx.doi.org/10.1016/j.ijgo.2009.07.016
- Lawn, J.E., Kinney, M., Lee, A.C., Chopra, M., Donnay, F., Paul, V.K., et al. (2009) Reducing intrapartum-related deaths and disability: Can the health system deliver? International Journal of Gynecology & Obstetrics, 107, S123-S142. http://dx.doi.org/10.1016/j.ijgo.2009.07.021
- Brailovschi, Y., Sheiner, E., Wiznitzer, A., Shahaf, P. and Levy, A. (2012) Risk factors for intrapartum fetal death and trends over the years. Archives of Gynecology and Obstetrics, 285, 323-329. http://dx.doi.org/10.1007/s00404-011-1969-8
NOTES
*Corresponding author.

