Open Journal of Preventive Medicine
Vol.4 No.7(2014), Article
ID:47740,8
pages
DOI:10.4236/ojpm.2014.47061
Perception of Blood Donation among Medical and Pharmaceutical Science Students of Nnamdi Azikiwe University, Awka
S. A. Nwabueze1, C. C. Nnebue1, E. C. Azuike1, C. A. Ezenyeaku1, C. C. Aniagboso1, O. E. Ezemonye1, E. D. Azuike2
1Department of Community Medicine, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria
2Department of Nursing Sciences, Faculty of Health Sciences, Nnamdi Azikiwe University, Awka, Nigeria
Email: emmanazuike@yahoo.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
![]()
![]()

Received 12 May 2014; revised 15 June 2014; accepted 27 June 2014
ABSTRACT
Background: Safe blood is a vital component in improving healthcare globally and millions of lives are saved each year through blood donation. But most hospitals in the developing countries face challenges of constant supply of blood to carry out different life saving procedures that require blood, due to paucity of blood donors. Many studies have been done on the perception of blood donation but only a few have been on Medical and Pharmaceutical Students. Aim: To determine the perception of blood donation among Medical and Pharmaceutical Students of Nnamdi Azikiwe University, Nnewi and Agulu Campuses respectively. Material and Methods: Stratified sampling technique was used to divide the students into strata (200, 300, 400, 500, and 600), then simple random sampling was used to select different respondents from each class and self-administered questionnaires were given to the respondents. Data was collected and results were analyzed. Results: 294 respondents, 147 medical students and 147 pharmaceutical students participated in the study 141 (95.9%) of medical students and 137 (93.2%) of pharmaceutical students had heard of blood donation. 139 (94.6%) of medical students and 140 (95.2%) of pharmaceutical students knew their blood groups. 59.5% of the respondents had donated blood. The commonest motivating factor towards blood donation is “to save a friend or family member”. Conclusion: The knowledge of the students regarding blood donation was high but the practice of blood donation was low.
Keywords:Perception, Blood Donation, Students, University, Nigeria

1. Introduction
Blood is a specialized body fluid in humans that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells [1] . Human blood is an element of human life [2] . The ancient Egyptians recognized the important properties of blood and it was used to resuscitate the sick, rejuvenate the old and infirm by bathing them with it and they also used it as a tonic for the treatment of various disorders [3] .
In 1740, Drs. Karl Landsteiner and Alexander Weiner experimented with the red blood cells of Rhesus monkeys. In 1901, Dr. Karl Landsteiner discovered the ABO blood group system, which was a very important factor in blood donation [4] .
The use of stored blood began during World War 1 (1914-1918), but the first large scale blood bank was not created until 1937, in Chicago [5] . The Canadian surgeon (Major L.B Robertson) serving in Canadian Army Medical Corps in the first World War was responsible for introducing transfusion in the management of war casualties to the British Army. Blood transfusion was generally accepted as the treatment of choice for severe blood loss by the end of the war [6] . Safe blood is a critical component in improving health care and in preventing the spread of infectious disease worldwide. Millions of lives are saved each year through blood transfusion, yet the quality and safety of blood transfusion are still the concern especially in the developing countries. Most blood is tested for diseases including sexually transmitted diseases (STDs) [7] . The donor is generally notified of the test result [8] .
The World Health organization recommended that donated blood should be tested for [9] Hepatitis B surface antigen, Antibody of Hepatitis, Antibody of HIV, usually subtype 1 and 2, Serologic test for syphilis. Other blood tests are done based on requirements in different countries. In our environment, blood for donation is screened for the following infectious diseases which could be transmitted through blood transfusion: Human Immune Deficiency Virus (HIV), Hepatitis B, Malaria and Syphilis. HIV/AIDS has a great impact on blood donation and transfusion [10] .
In the developed countries, most blood donors are unpaid volunteers who give blood for a community supply. In developing countries, established supplies are limited and donors usually give blood when family or a friend needs a transfusion. Some donors donate as an act of charity. Some are paid money or in some cases, there are incentives like paid time off from work. Since most of the component of blood used for transfusion have a short shelf life, (red blood cells the most frequently used being 35 - 42 days at a refrigerated temperature and 5 days for platelets) maintaining a constant supply is needed to help ensure that hospitals have access to adequate blood [11] . The ability to transfuse blood and its components represents one of the great advances in modern medicine [12] .
In a cross sectional study conducted to assess the knowledge and behavior towards voluntary blood donation among students of Tertiary Institutions in Nigeria by Salaudeen et al., it was found that 61% of the total respondents had good knowledge of blood donation while 85% of the respondents had never donated. Out of the 15% that had donated, 3% donated voluntarily. Among those that had ever donated, 57% were males. Many of the donors donated for friends (57%). The majority of the respondents (75%) were compelled to donate because of emergency situation. The reasons many did not donate were lack of opportunity (45%), due to tight lecture schedule and inadequate knowledge (24%) [13] . In Cross River State, Nigeria, a study by Offiong et al. showed that 60% of respondents had fears and misconceptions about blood donation. These included fear of fainting (12%), fear of contracting HIV in the process of blood donation (65%), witchcraft (10%) and religious constraints (7%) [14] . A study in Mwanza region of Tanzania showed that out of 1141 adults involved in the study, 26.4% had already donated blood, but only 3.8% had donated voluntarily within the previous 10 years [15] . A study among students of University of Dhaka, Bangladesh revealed that 82% of the participants showed a positive attitude towards blood donation. However, only 60% of the respondents in the study had actually donated voluntarily, while 93% had a negative attitude towards paid blood donation [16] . In a study in Lithuania, Soviet Union, by Buciuniene et al., it was found that paid donors comprised of 89.9%, while non-paid ones made 10.1% of the respondents. Research findings show that 93% of the paid-donors donated blood on a regular basis, while among the non-remunerated donors, the same figure amounted merely to 20.6%. The idea of the remunerated necessity is supported by 78.3% of the paid donors while 64.7% of the non remunerated respondents believed that remuneration is not necessary. The absolute majority of the paid donors (92%) think they should be offered a monetary compensation for blood donation, while more than half of the non-remunerated donors (55.9%) claimed they would be content with a mere appreciation of the act. About 28.4% of the respondents would carry on doing it, 29.6% would do it only in emergency, 29.6% would donate blood merely for their family or friend and 12.3% would quit it completely [17] .
A study among students of the University of Crete, Greece showed that the number of students that had ever donated blood was relatively small (16.6%) because they had little knowledge about blood donation, 83.4% were ignorant of the condition and criteria applying to the blood donation in general. Also a high number of respondents (63.1%) were ignorant of the social benefits from blood donation [18] . In the study at the Blood Centre of Umee University Hospital, Sweden, no statistically significant difference was found between male and female blood donors with regards to the general reasons and motives related to donating blood. The most frequently reported reasons for giving blood the first time were influence from a friend (47.2%) and request via media (23.5%). Among the general reasons/motives with highest ranking of importance, the most commonly reported motive for donating blood was general altruism (40.3%), social responsibility/obligation (19.7%) and influence from friends (17.9%). General altruism and Social responsibility/obligation were also the most frequent reasons for continuing to donate blood (68.4% and 16.0% respectively). The most common reported obstacle to becoming a regular blood donor was laziness (19.1%) followed by fear of needles (10.5%) [19] . A study conducted among students of Chula Long Kom University in Thailand showed that 80% of participants knew about blood donation while only 11% had ever donated blood voluntarily. Among non-donors, fear of getting infection was the commonest inhibiting factor to blood donation [20] . A study in Trinidad and Tobago reported that 81.2% of the respondents had never donated blood and of the 18.8% who had previously donated, replacement for a family member or friend was the commonest reason (86.9%) [21] .
2. Methodology
2.1. Study Area
This study was conducted at the Nnamdi Azikiwe University, at Nnewi and Agulu campuses both in Anambra State, Nigeria. Nnewi and Agulu are urban areas found in Anambra State. Nnewi is an urban town located in Nnewi North local government area. It is famous for trading of automobile parts. It has a population of about 391,227 from the 2006 census [22] . There are two tertiary study centres in Nnewi, the preclinical site at Otolo Nnewi and the clinical site located inside the Nnamdi Azikiwe Teaching Hospital Nnewi. The preclinical classes are the 200 and 300 level students while the clinical site has the 400, 500 and 600 level students.
Agulu is the campus where the pharmacy students stay. It is located in the Anaocha Local Government Area of Anambra State. The area is home to NAFDAC (National Agency for food, drug Administration and control) office in Anambra. There are 6 departments in the faculty and they include: Department of pharmaceutics and pharmaceutical Technology, Department of Pharmacognosy and Traditional Medicine, Department of Pharmacology and Toxicology, Department of Clinical Pharmacy and Pharmacy Management, Department of pharmaceutical and medicinal chemistry, Department of Pharmaceutical Microbiology and biotechnology.
2.2. Study Design
The study was a cross-sectional descriptive study.
2.3. Study Population
This included the medical and pharmaceutical students of Nnamdi Azikiwe University, Nnewi and Agulu Campuses respectively.
2.4. Minimum Sample Size Calculation
The minimum sample size of the population (<10,000) was determined using the formula [23] .
 where Nf is the desired sample size.
where Nf is the desired sample size.

N is the estimated population.
z is the standard normal deviate, which is 1.96 = 2.0.
p is the proportion of target population estimated to have a particular characteristic. 61% (0.61) [13] .
q is 1 − p.
d is the degree of accuracy which is 0.05.



 , with a rate of 10%.
, with a rate of 10%.
2.5. Sampling Technique
The stratified sampling technique was used. The medical and pharmaceutical students were divided into classes (200, 300, 400, 500 levels) plus 600 level for medical students. This was done using the class list, and then simple random sampling (balloting) method was used to select respondents from each class.
2.6. Data Collection Tool
A self-administered structured questionnaire was used. The questionnaire was in 3 sections: demographic characteristics, knowledge regarding blood donation, attitude towards and practice of blood donation. This study was conducted between 15th March and 15th April 2014.
2.7. Ethnical Consideration
Ethical approval was obtained from the NAUTH ethical committee.
2.8. Data Analysis
The data collected was analyzed using Statistical Software for Social Sciences (SPSS) Version 20. The following frequencies were presented in tables: the sociodemographic characteristics of the students, opinion of the students regarding blood donation, the proportion of the students that have actually donated blood or otherwise, the religious denomination of the students vis a vis the practice of blood donation, the motivating factors for blood donation and the reasons for not donating blood. Chi square test was used to test the association between the knowledge of the students regarding blood donation and the students’ course of study.
3. Results
Table 1 showed that the commonest age group was the 20 - 24 years age group for both the medical students and the pharmacy students while the least common age group is the ≥30 years age group. There were more male (60.9%) than female students (39.1%). The commonest class was the 200 level class (27.9%). The commonest religion was the Roman Catholics (48.6%).
Table 2 shows that 95.9% of the medical students and 93.2% know that blood donation is used in healthcare, but the difference is not statistically significant. 99.6% of the medical students knew their blood group while 95.2% of the pharmacy students knew their blood group, but the difference is not statistically significant. 93.2% of the medical students and 89.8% of the pharmacy students knew about cross-matching of blood, but the difference is not statistically significant. Majority of the students know that HIV can be transmitted through blood transfusion.
Table 3 shows that majority of the students believe that blood donation is a good practice in healthcare (83%).
They were more blood donors among the medical students (78.2%) than among the pharmacy students (40.8%) (Table 4).
Table 1. Demographic characteristics of the students.
Table 2. Association between the knowledge of the students regarding blood donation and their course of study.
Table 3. Attitude of the students towards blood donation.
Table 5 shows that Catholics had the highest positive response on practice of blood donation both among the medical students (85.5%) and the pharmacy students (53.3%). As expected none of the Jehovah’s witnesses has ever donated blood.
Table 6 shows that the commonest motivating factor towards blood donation among the students is “to save a friend or family member”.
Figure 1 is a bar chart showing the reasons why the students gave for not donating blood. The blue bars represent medical students while the ox-blood bars represent the pharmaceutical science students. The commonest reason for not donating blood by the students is the fear of infections, followed by the fear that they will develop fever.
4. Discussion
On the knowledge of blood donation, a high proportion of medical students (95.6%) and pharmacy students (93.2%) knew about blood donation and this is in consonance with a study conducted among students of Chula Hong Kong University in Thailand where 80.0% of the participants had knowledge of blood donation [20] . In the index study 99.6% and 95.2% of the medical and pharmacy students knew their blood groups. This is higher than 82% reported among students in India [24] . An even lower figure of 69.5% was reported in a study in Nepal [25] . However, a similar figure of 93.9% was reported among healthcare workers in Benin, Nigeria [26] . In the index study, 96.6% and 94.6% of the medical and pharmacy students respectively knew that HIV can be transmitted through blood donation. This is similar to the finding of a study in Benin which reported 91.4% [26] , but lower than 68.9% reported in Nepal [25] . 83% of respondents in the index study believe that donation is a
Table 5. Cross tabulation of the students religious denomination vs the status of haven donated blood.
Table 6. Greatest motivating factor for blood donation.
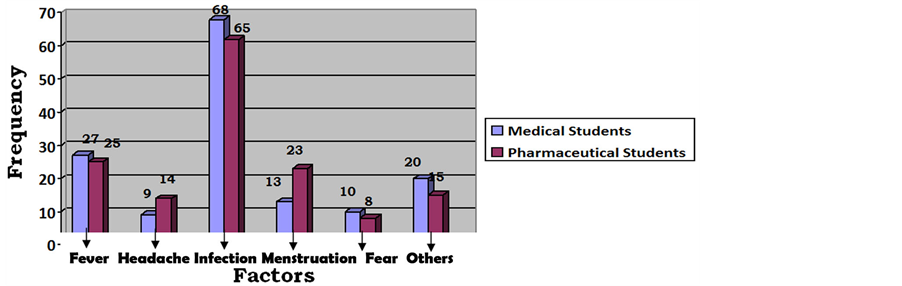
Figure 1. Reasons for not donating blood.
good practice in healthcare and should be encouraged. A similar figure of 81.6% was reported in Benin, Nigeria [26] , a higher figure (97.6%) was reported among students in India [25] . A probe into the practice of blood donation among the students in this index study revealed that 59.5% of the respondents have donated blood previously. This is higher than the reported figures of 18.7%, 18.1%, 22.1%, and 24.6% in several studies [24] [25] [26] . In the index study when asked reasons for not donating blood, 56.3% of medical respondents and 42.2% of pharmaceutical respondents had fear of infection as their reason for not donating blood. This is relatively in line with a study done on community mobilization for blood donation in Cross Rivers State Nigeria where fear of contracting HIV (65.0%) was the commonest reason for not donating blood [14] .
On the greatest motivating factor for blood donation, 49.6% of the medical respondents who answered the question and 45.0% of the pharmacy students believed that their greatest motivator was to save a friend or a family member. This is in consonance with the study at the blood centre of Umee University Hospital, Sweden, where 47.2% of the respondents said their motivator for donating blood was to save a friend [19] .
5. Conclusions and Recommendations
This study has demonstrated that although the students have good knowledge of blood donation, the actual practice of blood donation is not high and their reasons for not donating blood are issues that can be handled effectively. It is therefore recommended that: Religious Organizations should provide a platform to educate their members on the need to donate blood. They should challenge their members to show selflessness and acts of kindness, and also to dispense with unnecessary fears over blood donation as the practice is safe. Government should embark on widespread enlightenment campaign on the social implications of voluntary blood donation. The media should be more involved in this advocacy, as well as health, professional and non-governmental organizations as a corporate social responsibility. More studies should be carried out and published on blood donation to enable people appreciate the paucity of blood donors. This would encourage a good number to make themselves available to donate blood and to help others in need. Students Union Governments and other Organizations in the Universities should include blood donation drive in their activities.
Limitations: Only 294 students participated in this study. This was because of resources. We suggest that further studies with larger number of students and involving more departments be conducted. This will generate more reliable results.
References
- The Franklin Institute Incorporation (2014) “Blood” The Human Heart. http://www.fi.edu/learrn/heart/blood.blood.html
- Zmijewski, C.M. and Haesler, W.E. (1982) Blood Banking Science. Appleton Century Croft, New York.
- Smith, B.R. (2008) Blood. Microsoft Corporation, Redmond.
- Landsteiner, K. and Weiner, A.S. (1940) An Agglutinable Factor in Human Blood Recognized by Immunosera in Rhesus Blood. The Society for Experimental Biology, 42, 223. http://dx.doi.org/10.3181/00379727-43-11151
- Mc-Carthy, P.R. (2007) Blood Donation. Microsoft Corporation, Redmond.
- Pinkerton, P.H. (2008) Canadian Surgeon and the Introduction of Blood Transfusion in War Surgery. Transfusion Medicine Reviews, 22, 77-86. http://dx.doi.org/10.1016/j.tmrv.2007.09.004
- Elert, G. (2014) Volume of Blood in a Human. http://www.webcitation.org
- Miller, R., Hewitt, P.E., Warwick, R., Moore, M.C. and Vincent, B. (1998) Review of Counseling in a Transfusion Service: The London (UK) Experience. Vox Sanguinis, 74, 133-139. http://dx.doi.org/10.1046/j.1423-0410.1998.7430133.x
- American Association of Blood Banks (2014) Donor Screening and Testing. www.aabb.org/resources/governmentregulatory//donoreligibility
- World Health Organization (2009) Screening Donated Blood for Transfusion-transmissible Infections. WHO, Geneva.
- Lockwood, W.B., Hudgens, R.W., Szymankski, I.O., Teno, R.A. and Gray A.D. (2003) Effect of Rejuvenation and Frozen Storage on 42-Days Old As-3 RBC. Transfusion, 43, 1527-1532. http://dx.doi.org/10.1046/j.1537-2995.2003.00551.x
- Olaiya, M.A., Alakija, W. and Afala, A. (2004) Knowledge, Attitude, Beliefs and Motivations towards Blood Donation among Blood Donors in Lagos, Nigeria. Transfusion Medicine, 14, 13-17. http://dx.doi.org/10.1111/j.0958-7578.2004.00474.x
- Salaudeen, A.G. and Odeh, E. (2011) Knowledge and Behaviour towards Voluntary Blood Donation among Students of Tertiary Institution in Nigeria. Nigerian Journal of Clinical Practice, 14, 303-307. http://dx.doi.org/10.4103/1119-3077.86773
- Offiong, J.G., Auquo, E.E. and Olaniran, N.S. (1997) Community Mobilization for Blood Donation, Cross River State, Nigeria. International Journal of Obstetrics and Gynaecology, 59, 119-125.
- Jacobs, B. and Berege, Z.A. (1995) Attitude and Beliefs about Blood Donation among Adults in Mwanza Region, Tanzania. East African Medical Journal, 72, 345-348.
- Hosain, G.M., Anisuzzaman, M. and Begum, A. (1997) Knowledge and Attitude towards Voluntary Blood Donation among Dhaka University Students in Bangladesh. East African Medical Journal, 74, 549-553.
- Buciuniene, I., Laimute, S. and Aurelija, B. (2006) Blood Donors’ Motivation and Attitude to Non-Remembered Blood Donation in Lithuania. Biomed Central Public Health, 6, 166. http://dx.doi.org/10.1186/1471-2458-6-166
- Merkouri, A., Tsouras, C. and Androulakus, M. (2005) ICUS Nurses Web Journal, 23, 100-190.
- Sojka, B.N. and Sojka, P. (2008) The Blood Donation Experience: Self-Reported Motives for and Obstacles to Donating Blood. Vox Sanguinis, 94, 56-63.
- Wanitkit, V. (2002) Knowledge about Blood Donation among a Sample of Thai University Students. The International Journal of Transfusion Medicine. Vox Sanguinis, 83, 97-99. http://dx.doi.org/10.1046/j.1423-0410.2002.00209.x
- Sampath, S., Ramsaran, V. and Parasram, S. (2007) Attitude towards Blood Donation in Trinidad and Tobago. Transfusion Medicine, 17, 97-99. http://dx.doi.org/10.1111/j.1365-3148.2007.00731.x
- National Population Commission (2008) 2006 National Census Report. www.population.gov.ng
- Araoye, M.O. (2004) Research Methodology with Statistics for Health and Social Sciences. Nathadex Publishers, Ilorin.
- Jose, A.P., Angadi, M.M., Masali, K.K., Bhat, S., Shashank, K.J. and Wajantri, P. (2013) Knowledge Attitude and Practices on Voluntary Blood Donation among College Students in Bijapur, Karnataka. IJCRR, 5, 26-31.
- Amatya, M. (2013) Study on Knowledge, Attitude and Practice of Blood Donation among Students of Different Colleges of Kathmandu, Nepal. International Journal of Pharmaceutical and Biological Archives, 4, 424-428.
- Nwogoh, B., Aigberadion, U. and Nwannadi, A.I. (2013) Knowledge, Attitude and Practice of Voluntary Blood Donation among Healthcare Workers at the University of Benin Teaching Hospital, Benin-City, Nigeria. Journal of Blood Transfusion, 2013, Article ID: 797830. http://dx.doi.org/10.1155/2013/797830


