Open Journal of Internal Medicine
Vol.07 No.02(2017), Article ID:76992,11 pages
10.4236/ojim.2017.72003
Decentralized Management of Diabetes Mellitus by General Patrician
Demba Diédhiou*, Djiby Sow, Ibrahima Mané Diallo, Ahmadou Diouara, Michel Alassane Ndour, Maimouna Ndour-Mbaye, Anna Sarr, Said Norou Diop
Department of Internal Medicine, Abass Ndao Hospital Center, Cheikh Anta Diop University, Dakar, Senegal

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: April 13, 2017; Accepted: June 16, 2017; Published: June 19, 2017
ABSTRACT
Introduction: In Senegal, the frequency of diabetes mellitus is estimated at 3.2% and its management by the general patrician (gp) is dissatisfied. The objective was to evaluate the decentralized monitoring of diabetes mellitus and other cardiovascular risk factors by a trained general practician. Patients and methods: It was a retrospective, descriptive study conducted from June 1, 2013 to 31 May, 2015 in Dakar, where included the files of subjects with diabetes mellitus regularly followed. The data collected were epidemiological, diagnostic and therapeutic. Results: It was of 125 diabetics patients with a mean age of 56.4 years old. At the inclusion, their diabetes had a mean duration of 6.3 years and a mean average HbA1c of 10.4%. The complications were a neuropathy in 58 cases (46.4%), an arteritis in 46 cases (36.8%), a nephropathy in 16 cases (12.8%) and a retinopathy in 28 cases (22.4%). Other cardiovascular risk factors were an arterial hypertension in 74 cases (59.2%), smoking in 11 cases (8.8%), kidney disease in 16 cases (12.8%), and LDL- cholesterol > 1.6 g/l in 39 cases (31.2%). In total, 87 patients (69.6%) were at high cardiovascular risk and among them, 81.6% had LDL-cholesterol > 1g/l. At inclusion, anti-diabetic treatment was oral mono-therapy in 53 cases (42.4%), an insulin therapy in 49 cases (39.2%). After 12 month of follow-up, the dual therapy anti-diabetic was increased from 13.6% to 34.4%. The others associated drugs were anti-hypertensives in 72 cases (57.6%), statins in 29 cases (23.2%) and anti-platelet agent in 46 cases (36.8%). Only 31.2% of the patients with nephropathy were under the renin angiotensin system blockers. Statins and the anti-platelet agents were prescribed respectively at 25.2% and 47.1% of the 87 patients at high cardiovascular risk. During follow-up, the target HbA1c < 7% was reached in 76 cases (60.8%). Conclusion: our study shows the importance and the interest of a trained general practician for the management of non-communicable diseases. However, it would be necessary to strengthen training in the care of other cardiovascular risk factors.
Keywords:
Diabetes Mellitus, Risk Factors, Followed Decentralized, General Patrician, Senegal

1. Introduction
Estimates of the 2015 International Federation of Diabetes reported a global prevalence of diabetes by 8.8%. In Senegal it is estimated at 3.2% [1] . Diabetes mellitus is known for its morbidity and risk of mortality especially in association with other cardiovascular risk factors. In Senegal, the peak towards specialized center had motivated since 2001 decentralization of management of diabetes mellitus with General Patrician. It is the initial coverage in the primary or secondary sanitary structures by a general practitioner formed in follow-up of first level of the simple cases of the diabetes mellitus. In Sub-Saharan Africa, works on diabetes management by the General Patrician are mostly transverse. They relate essentially diagnostic and therapeutic failure [1] [2] [3] . It is in this light that we conducted this study with goal making an assessment of decentralized management of diabetes mellitus and other cardiovascular risk factors among 125 diabetes subjects followed over a period of 12 months by a trained General Patrician.
2. Patients and Methods
It was a retrospective, descriptive study conducted from June 1, 2013 to 31 May, 2015 in a health center of Pikine (Dakar). The health center Baye Talla Diop (Ex Dominique) contains the departments of general medicine (adult and child), exploration and gynecology-obstetrics. The department of general medicine contains a common hospitalization, a unit of consultation and a care service of the wounds among which is the diabetic foot ulcer. His staff contains 8 doctors among whom 6 specialists and 1 general practitioner trained in diabetology, and 24 nurses. There is a continuous medical service of 24 hours in charge of the follow-up of the general cases and medical emergencies. In it, it is added a consultation specialized once a week and by specialty (cardiology, dermatology, neurology, orthopedics, nephrology, odontology, ophthalmology, diabetology). The consultations of diabetology are made by appointment every Wednesday and Thursday with deadlines of meeting between 2 to 3 weeks. The appointments of control are made all 3 to 4 months. The therapeutic education in diabetology takes place during the consultation. It concerns all the new diabetics but also the accompanying persons and the family of the patients. All the explorations which the diabetic needs for the follow-up of his disease are available at the level of the health center of Pikine. It was wearing on the evaluation or an audit of decentralized support of diabetes mellitus and other cardiovascular risk factors by the General Practitioner of this heath center formed in practice of diabetology. It is the initial coverage in the primary or secondary sanitary structures by a general practitioner formed in follow-up of first level of the simple cases of the diabetes mellitus. This doctor had benefited from several sessions of continuing medical education in diabetology and metabolism, organized by the Ministry of public health and social action of Senegal, the Buddy Doctor Initiative Program of Novo Nordisk and the Marc Sankale Center of Dakar (national reference center for the treatment of endocrine and metabolic diseases in Senegal since 1960). The study included all the files of followed subjects with diabetes mellitus received in the consultation and regularly monitored during the study period at the health center of Pikine. The follow-up was considered regular if the patients respected return them quarterly of control. Incomplete records, those of irregular and lost to follow-up patients were not included in the assessment. For the calculation of the size of the sample, we proceeded as follows by the Open EPI software: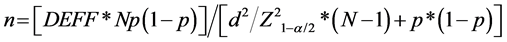 .
.
The size of diabetic population following in the Pikine heath care center is 950 diabetic subjects. The hypothetical frequency of diabetes mellitus in the Senegalese population according by the International Diabetes Federation (IDF) is estimated to 3.2% and the estimated confidence limits is 5%. The factor of calculation is 1. For a level confidence of 99.99%, the representative size was 118 diabetic patients.
All patients had received a quarterly monitoring and this was for 12 months. A standard questioner was prepared as the basis for collecting data from the monitoring folder. The data collected for this study were:
- Epidemiological data: age, sex, other cardiovascular risk factors such age (> 50 years for men and > 60 years for women), chronic kidney disease, smoking, high blood pressure, micro albuminuria > 30 mg/24 hours, LDL-cholesterol > 1.6g/l, HDL-cholesterol < 0.4g/l. We have also assessed the existence of an arteritis such as ischemic stroke, arteriopathy of the lower limbs, suggestive electrocardiographic and clinical signs of coronary heart disease. The existence of a coronary heart disease or a sudden death at first degree in the family was also taken into account [4] . The subjects were considered arterial hypertensive if their blood pressure was or not stabilized under anti-hypertensive treatment or if they had a blood pressure ≥ 140 and/or 90 mmHg [5] . Dyslipidemia was defined by the presence of one or more of the following anomalies or a known history of dyslipidemia according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) [6] . It’s a total cholesterol > 2 g/l, triglyceride > 1.5 g/l, HDL-cholesterol < 0.5 g/l in women or < 0.4 g/l in men and a LDL-cholesterol > 1.6 g/l. Waist size according to the classification of the NCEP ATP III of 2001 [6] and the body mass index (BMI) according to the classification of the International Obesity Task Force [7] were also evaluated. The high cardiovascular risk was defined according to the recommendations of the College of the high authority of health (HAS) in 2012. He is a diabetic type 2 with renal impairment or an arteritis or with at least two of the following risk factors: age, family history of early heart disease, smoking, high blood pressure, HDL- cholesterol < 0.4 g/l, and microalbuminuria > 30 mg/24 hours.
- Study of diabetes mellitus: age at diagnosis, type of diabetes, his mean duration. Glycemic level and chronic complications were also evaluated. The typing of diabetes, in the absence of immunology and the dosage of the peptide C, was presumptive based on clinical and evolutionary argument (age of patient, his morphotype, time of installation of the symptoms, family history and evolution under treatment).
- Management of diabetes mellitus and his evolution: realization of a dietary education, practice of physical activity, the drug treatment of diabetes mellitus such oral anti diabetic (ADO), insulin and other cardiovascular risk factors. The patients were well balanced on the basis of a fasting blood sugar < 1.21 g/l and an HbA1c < 7% as recommended by the American Diabetes Association [8] . The Eight Joint National Committee recommendations were used to judge normality of blood pressure [5] . For the descriptive analysis, data were presented in percentage for the qualitative variables and mean for the quantitative variables. Entry and operation were carried out by the software SPSS STATISTICS 18.0.
3. Results
3.1. Clinical Profile of Patients at the Inclusion
One hundred twenty five (125) patients were included. Their diabetes had less than 6 years duration in 72 cases (57.6%) and more than 10 years in 32 cases (25.6%). On the glycemic level, it was a hyperglycemic in 94 cases (75.2%), a ketosis in 22 cases (17.6%), and ketoacidosis in 9 cases (7.2%). A1c Hemoglobin (HbA1c) level was less than 6.5% in 3 cases (2.4%), between 7 and 9% in 41 cases (32.8%) and > 9% in 81 cases (64.8%). The Table 1 shows the characteristics of the study population at inclusion.
3.2. Assessment of Complications and Other Cardiovascular Risk Factors
The research of chronic complication was 100% for coronary heart diseases (via electrocardiogram), 96% for kidney disease (microalbuminuria and creatinine) and 80% for retinopathy. In our patients, we found a moderate (17.6%) and severe (12%) high blood pressure, a severe to morbid obesity in 12 cases (9.6%). According to the classification of the NCEP ATP III of 2001 [6] , waist size were higher in 3.2% of men and 80.8% of women. The patients had diabetic neuropathy in 58 cases (46.4%). An arteritis was found in 46 cases (36.8%) of which 32.8% were a suggestive signs of coronary disease.
Persistent impairment of kidney function was found in 16 cases (12.8%) and a micro albuminuria > 30 mg/24 hours in 16 cases (12.8%). Lipid abnormalities were a LDL-cholesterol > 1.6 g/l in 39 cases (31.2%), HDL-cholesterol < 0.4 g/l in 11 cases (8.8%), total cholesterol > 2 g/l in 73 cases (58.4%), triglycerides > 1.5 g/l in 14 cases (11.2%). Patients with suggestive signs of coronary artery diseases had a mean age of 58.8 years, an average duration of diabetes of 8.9 years, obesity or overweight in 55% and high blood pressure in 77.5% of cases. Their mean
Table 1. Characteristics of the population study at inclusion.
LDL-cholesterol was to 1.5 g/l, mean total cholesterol to 2.3 g/l, mean triglycerides to 0.9 g/l and mean rate of HbA1c to 10.4%.
In total, 87 patients (69.6%) presented at least 3 cardiovascular risk factors or an arteritis (coronary disease, stroke, arteriopathy of the lower limbs). They were all type 2 diabetes mellitus. Among them, 81.6% had LDL-cholesterol > 1g/l.
3.3. Assessment of Management:
Among the subject, 62 subjects (49.6%) had received a dietary education and 20 (16%) practice regularly physical activity. At inclusion, antidiabetic treatment consisted of an oral monotherapy in 53 cases (42.4%), a dual oral therapy in 11 cases (8.8%). Insulin was given in 43 cases (34.4%) and combined with oral antidiabetic agents in 6 cases (4.8%). In 12 cases (9.6%), the patients observed at dietary measures. After 12 month of follow-up, the dual therapy associated with insulin or oral antidiabetic was increased from 13.6% to 34.4%. An increase of the dosage in oral or insulin monotherapy was found in 70 patients (56%) (Figure 1). The others associated drugs were an antihypertensive in 72 cases (57.6% of which 23.2% were in calcic inhibitor, 15.2% in the Renin angiotensin system blockers and 19.2% in a fixed dual therapy). A salt diet alone was given in 17 cases (13.6%). The statin was prescribed in 43.5% of 46 diabetics subjects with arteritis, and in 25.2% of the 87 patients with high cardiovascular risk. The antiplatelet agents were prescribed in 60.8% of diabetics subjects with an arteritis and in 47.1% of them at high cardiovascular risk. During follow-up, the target HbA1c < 7% was reached in 76 cases (60.8%) (Figure 2). A normalization of blood pressure was found in 77 cases (61.6%).
4. Discussion
We bring the data of a quarterly monitoring over a period 12 months, in a series of 125 diabetics subjects by a General Patrician. The limitations of the study are constituted by the fact that it is an observational study conducted from patients’ files. Only the files of patients who have respected the follow-up were included. This has led to a selection bias with results that will not reflect necessarily the context of daily practice. In addition, restraining the diagnosis of coronary disease on only anomalies electrocardiographic certainly created false negatives. This kind of work doesn’t require in Senegal the approval of ethic committee because it is a retrospective work on patient’s file.
Figure 1. Evolution of oral antidiabetic (ADO) and insulin prescription during the follow up.
Figure 2. Evolution of the mean of HbA1c during the 12 months of follow up.
4.1. Socio-Demographic Aspects
The profile of our patients is similar to data from Sub-Saharan African [2] [9] [10] . It was diabetes subject in mean age between 40 and 50 years old, mean duration of diabetes mellitus in way of 7 year and most often poor glycemic control. For example, we will cite two multicenter studies representative of the African region. The DiabCare Africa study [2] was conducted with 2352 type 2 diabetic patients selected in East (Tanzania, Kenya), Center (Cameroon) and West Africa (Ghana, Senegal and Nigeria). The patients were already followed in their structure to recruiting. The authors reported a mean age of 53 ± 16 years, a mean duration of diabetes of 8 ± 6 years. Only 29.2% of them had an HbA1c < 6.5% rate. The other international observational study IDMPS (International Diabetes Management Practice Study) [9] was conducted among 2265 diabetics Africa subjects (Algeria, Egypt, Morocco, Tunisia, Senegal and Cameroon). He was found similar data with a mean age 57.4 ± 1 years, duration of diabetes of 8.6 years. The target of HbA1c < 7% was reached in 31% of cases. Elsewhere in the Western countries, the STENO 2 study [11] , report a mean rate of HbA1c at inclusion to 8.4% ± 1.6% and 8.8% ± 1.7% respectively for intensive and conventional treatment groups. The differences are the fact that some of our patients had diabetes mellitus recent discovery without drug treatment.
4.2. Assessment of Complications and Other Cardiovascular Risk Factors
Type 2 diabetes mellitus is specially known to be purveyor of chronic complications or associated with cardiovascular risk factors [12] . However, evaluating practice diabetes in Africa, particularly with General practitioner, often reported a non-exhaustive screening of these parameters [2] [10] . This is in part explained by inadequate health coverage and access to care in most of these countries. This assessment of complications and other cardiovascular risk factors was 93% in the IDMPS study [9] . In this series, it was a high blood pressure (57%), dyslipidemia (47%), and microangiopathie (14%). African literature reveals a wide variability in the frequency of chronic complications of diabetes [13] [14] [15] . In a systematic review on the prevalence and complications of diabetes mellitus in North Africa, the authors reported a retinopathy (8.1% to 46.3%), and neuropathy (21.9% to 60%), [13] . Our high frequency of coronary disease is explained by a systematization of the electrocardiogram and an accounting of any anomalies suggestive of coronary heart disease. In addition, impairment of kidney function was found in 12.8% of cases. According the SURDIAGENE and DIABHYCAR group [16] , this setting of bad prognosis would be correlated with the number of risk factors and the high cardiovascular risk of the diabetes subjects.
4.3. Assessment of Management
Healthy lifestyle and physical activity are an essential link in the support of disorders of carbohydrate metabolism and insulin resistance. Dahjio et al. [17] in Cameroon had assessed the impact of 12 weeks of a physical activity program among type 2 diabetics subjects aged 50 years and more. They reported a statistically significant improvement of anthropometric parameters. It is a reduction of the weight, waist, visceral fat, and Glycemic level, increased lean mass and physical performance. Several other large interventional studies had already proved this impact in the pre diabetes [18] and diabetes [19] [20] . In the Look AHEAD Trial [19] , is reported a significant weight loss (−6.15% vs −0.88%), an improvement in physical performance (+12.74% vs +1.96%), reduction in HbA1c (−0.36% vs -0.09%), a reduction of systolic blood pressure (5.33 vs 2.97 mmHg), an increase of HDL-cholesterol (+3.67 vs +1.97 mg/dl), and a decrease in triglycerides (−25.56 vs −19.75 mg/dl) in the intensive intervention vs standard intervention group.
On the drug medication, alone or in combination therapy, metformin remains the pillar of anti-diabetic therapy initiation. A transient insulin therapy at the outset is authorized in case of deep poor glycemic control [21] [22] . However, our study reported a low rate of 40% of patients on insulin in the light of the 64.8% of patients with HbA1c > 9% at inclusion. Therapeutic inertia is the explanation and remains a reality in diabetes mellitus, especially in sub-Saharian Africa [2] [3] [9] [10] . After 12 month of follow-up, the evolving profile of antidiabetic pharmacology seems like the finding reported in DiabCare Africa [2] . The only difference lies in the fact that more than 60% of our patients had reached the target of HbA1c < 7%. This would probably explain the high proportion (40%) of patients in oral mono-therapy after 12 months of follow-up. This satisfactory rate in terms of target HbA1c is the reflection of a selection bias. Only regular patients and having access to care were selected in this study. The latest recommendation from the American Diabetes Association of 2017 [23] placed at the same level of performance the four anti-hypertension classes (ACE inhibitors, angiotensin receptor blockers, thiazide-like diuretics, or calcium channel blockers) in the management of arterial hypertension in diabetic patients without albuminuria. In the case of diabetic nephropathy, inhibitors of the renin angiotensin blockers at maximum tolerated dose are indicated. This was not the case in our series, since only 31.2% patients with micro albuminuria were under blocker of the renin angiotensin system. In our series, 69.6% of the patients were carriers of least 3 cardiovascular risk factors or an arteritis. Among them, 81.6% had LDL-cholesterol > 1 g/l. In diabetics at high cardiovascular risk, the benefit of a statin and an anti-platelet is demonstrated in both primary and secondary prevention [23] . A meta-analysis including data from over 18.000 patients with diabetes from 14 randomized trial of statin therapy, demonstrate a 9% reduction in all-cause mortality and 13% reduction in vascular mortality for each mmol/L (39 mg/dl) reduction in LDL-cholesterol [24] . Thus, current recommendations for using aspirin as primary prevention include both men and women aged > 50 years with diabetes and at least one additional major risk factor (family history of premature acute sign of cardiovascular disease, hypertension, dyslipidemia, smoking, or chronic kidney disease/albuminuria) who are not at increased risk of bleeding [25] [26] [27] [28] .
5. Conclusion
Our study shows in a country where the number of specialists is still low, the importance and interest of the follow-up of no communicable diseases by a trained General Practician. Our study reports diabetic subjects at high cardiovascular risk.
6. Suggestion
Management in adequate conditions and based on recommendations could help to achieve glycemic targets and control other cardiovascular risk factors. However, efforts should be carried out in continuous medical education to optimize the overall support of the diabetic patients by the general practitioner.
Conflict of Interest
The authors have nothing to disclose.
Cite this paper
Diédhiou, D., Sow, D., Diallo, I.M., Diouara, A., Ndour, M.A., Ndour-Mbaye, M., Sarr, A. and Diop, S.N. (2017) Decentralized Management of Diabetes Mellitus by General Patrician. Open Journal of Internal Medicine, 7, 25-35. https://doi.org/10.4236/ojim.2017.72003
References
- 1. Diop, S.N. and Diédhiou, D. (2015) Diabetes Mellitus in Sub-Saharan Africa: Epidemiological and Socioeconomic Aspects. Médecine et Maladies Infectieuses, 9, 123-129.
https://doi.org/10.1016/S1957-2557(15)30030-4 - 2. Sobngwi, E., Ndour-Mbaye, M., Boateng, K.A., et al. (2012) Type 2 Diabetes Control and Complications in Specialized Diabetes Care Centers of Six Sub-Saharan African Countries: The Diabcare Africa study. Diabetes Research and Clinical Practice, 95, 30-36.
https://doi.org/10.1016/j.diabres.2011.10.018 - 3. Ndour-Mbaye, M., Sarr, A., Diop, S.N., et al. (2011) DiabCare Senegal: A Survey on Diabetes Management in Senegal. Médecine et Maladies Infectieuses, 5, 85-89.
- 4. Afssaps, High Authority of Health. (2006) Medicinal Treatment of the Type 2 Diabetes. Recommendations.
- 5. James, P.A., Oparil, S., Carter, B.L., et al. (2014) Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). The Journal of the American Medical Association, 311, 507-520.
https://doi.org/10.1001/jama.2013.284427 - 6. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation, 106, 3143-3421.
- 7. Cole, T.J., Bellizzi, M.C., Flegal, M.E., et al. (2000) Establishing a Standard Definition for Overweight and Obesity Worldwide: International Survey. British Medical Journal, 320, 1240-1243.
https://doi.org/10.1136/bmj.320.7244.1240 - 8. American Diabetes Association (ADA) (2008) Medical Management of Hyperglycemia in Type 2 Diabetes: A Consensus Algorithm for the Initiation and Adjustment of Therapy. Diabetes Care, 31, S1-S11.
- 9. Gagliardino, J.J., Atanasov, P.K., Chan, J.C.N., et al. (2017) Resource Use Associated with Type 2 Diabetes in Africa, the Middle East, South Asia, Eurasia and Turkey: Results from the International Diabetes Management Practice Study (IDMPS). BMJ Open Diabetes Research and Care, 5, 1-10.
https://doi.org/10.1136/bmjdrc-2016-000297 - 10. Diop, S.N., Wade, A., Lokrou, A., Diédhiou, D. and Adoueni, V.K. (2013) Management of Type 2 Diabetes in Clinical Practices in Sub-Saharan Africa: Results of the AMAR-AFO Study in Senegal and Ivory Cost. Médecine et Maladies Infectieuses, 7, 363-367.
https://doi.org/10.1016/S1957-2557(13)70603-5 - 11. Gaede, P., Lund-Andersen, H., Parving, H.H. and Pedersen, O. (2008) Effect of a Multifactorial Intervention on Mortality in Type 2 Diabetes. The New England Journal of Medicine, 358, 580-591.
https://doi.org/10.1056/NEJMoa0706245 - 12. Adebamowo, S.N., Adeyemo, A.A., Tekola-Ayele, F., et al. (2016) Impact of Type 2 Diabetes on Impaired Kidney Function in Sub-Saharan African Populations. Frontiers in Endocrinology, 7, 1-6.
https://doi.org/10.3389/fendo.2016.00050 - 13. Bos, M. and Agyemang, C. (2013) Prevalence and Complications of Diabetes Mellitus in Northern Africa, a Systematic Review. BMC Public Health, 13, 387.
https://doi.org/10.1186/1471-2458-13-387 - 14. Burgess, P.I., MacCormick, I.J.C., Harding, S.P., Bastawrous, A., Beare, N.A.V. and Garner, P. (2013) Epidemiology of Diabetic Retinopathy and Maculopathy in Africa: A Systematic Review. Diabetic Medicine, 30, 399-412.
https://doi.org/10.1111/j.1464-5491.2012.03756.x - 15. Noubiap, J.J.N., Naidoo, J. and Kengne, A.P. (2015) Diabetic Nephropathy in Africa: A Systematic Review. World Journal of Diabetes, 6, 759-773.
https://doi.org/10.4239/wjd.v6.i5.759 - 16. Ragot, S., Saulnier, P.J., Velho, G., et al. for the SURDIAGENE and DIABHYCAR Study Groups (2016) Dynamic Changes in Renal Function Are Associated with Major Cardiovascular Events in Patients with Type 2 Diabetes. Diabetes Care, 39, 1259-1266.
https://doi.org/10.2337/dc15-2607 - 17. Dahjio, Y., Noubiap, J.J.N., Azabji-Kenfack, M., et al. (2016) Impact of a 12-Week Aerobic Exercise Training Program on Anthropometric and Metabolic Parameters of a Group of Type 2 Diabetes Cameroonian Women Aged ≥50 Years. Annals of Translational Medicine, 4, 364.
https://doi.org/10.21037/atm.2016.09.26 - 18. Li, G., Zhang, P., Wang, J., et al. (2008) The Long-Term Effect of Lifestyle Interventions to Prevent Diabetes in the China Da Qing Diabetes Prevention Study: A 20-Year Follow-Up Study. Lancet, 371, 1783-1789.
https://doi.org/10.1016/S0140-6736(08)60766-7 - 19. The Look AHEAD Research Group. (2010) Long Term Effects of a Lifestyle Intervention on Weight and Cardiovascular Risk Factors in Individuals with Type 2 Diabetes: Four Year Results of the Look AHEAD Trial. Archives of Internal Medicine, 170, 1566-1575.
- 20. American Diabetes Association (2017) Lifestyle Management. In Standards of Medical Care in Diabetes 2017. Diabetes Care, 40, S33-S43.
https://doi.org/10.2337/dc17-s007 - 21. Harper, W., Clement, M., Goldenberg, R., et al. (2013) For the Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Pharmacologic Management of Type 2 Diabetes. Canadian Journal of Diabetes, 37, S61-S68.
https://doi.org/10.1016/j.jcjd.2013.01.021 - 22. American Diabetes Association (2017) Pharmacologic Approaches to Glycemic Treatment. In Standards of Medical Care in Diabetes 2017. Diabetes Care, 40, S64-S74.
https://doi.org/10.2337/dc17-s011 - 23. American Diabetes Association. (2017) Cardiovascular Disease and Risk Management. In Standards of Medical Care in Diabetes 2017. Diabetes Care, 40, S75-S87.
- 24. Cholesterol Treatment Trialists’ Collaborators, Kearney, P.M., Blackwell, L., Collins R., et al. (2008) Efficacy of Cholesterol-Lowering Therapy in 18.686 People with Diabetes in 14 Randomized Trials of Statins: A Meta-Analysis. Lancet, 371, 117-125.
https://doi.org/10.1016/S0140-6736(08)60104-X - 25. Huxley, R.R., Peters, S.A.E., Mishra, G.D. and Woodward, M. (2015) Risk of All-Cause Mortality and Vascular Events in Women versus Men with Type 1 Diabetes: A Systematic Review and Meta-Analysis. The Lancet Diabetes & Endocrinology, 3, 198-206.
https://doi.org/10.1016/S2213-8587(14)70248-7 - 26. Peters, S.A.E., Huxley, R.R. and Woodward, M. (2014) Diabetes as Risk Factor for Incident Coronary Heart Disease in Women Compared with Men: A Systematic Review and Meta-Analysis of 64 Cohorts Including 858,507 Individuals and 28,203 coronary Events. Diabetologia, 57, 1542-1551.
https://doi.org/10.1007/s00125-014-3260-6 - 27. Kalyani, R.R., Lazo, M., Ouyang, P., et al. (2014) Sex Differences in Diabetes and Risk of Incident Coronary Artery Disease in Healthy Young and Middle-Aged Adults. Diabetes Care, 37, 830-838.
https://doi.org/10.2337/dc13-1755 - 28. Peters, S.A.E., Huxley, R.R. and Woodward, M. (2014) Diabetes as a Risk Factor for Stroke in Women Compared with Men: A Systematic Review and Meta-Analysis of 64 Cohorts, Including 775,385 Individuals and 12,539 Strokes. Lancet, 383, 1973-1980.
https://doi.org/10.1016/S0140-6736(14)60040-4




