Health
Vol. 4 No. 7 (2012) , Article ID: 21184 , 7 pages DOI:10.4236/health.2012.47065
Self-assessed health and its aspects in the case of Mongolia
![]()
1Graduate School of Comprehensive Human Sciences, University of Tsukuba, Tsukuba, Japan; *Corresponding Author: c0930400@md.tsukuba.ac.jp
2Japan Society for the Promotion of Science, Tokyo, Japan
3Philanthropy Centre for Children and the Elderly, Ulaanbaatar, Mongolia
Received 20 April 2012; revised 11 May 2012; accepted 25 May 2012
Keywords: Self-Assessed Health; Socio-Demographic Status; Daily Life and Life-Style; Community Motivation; Social Environment; Health Service Utilization and Mongolia
ABSTRACT
Self health assessment is a simple indicator that is widely used for measuring an individual’s perception of his or her overall health. Many studies have been conducted by way of showing which particular aspects should be included in health self assessment, especially in developed world. In the developing world, however, very few studies have examined self health assessment. The aim of this study was to identify particular aspects and associations in self health assessment and differences between subgroups in Ulaanbaatar, Mongolia. The area sampling approach and Kish tables were used for selecting respondents. Total 500 respondents were surveyed by paper-based questionnaires. Spearman’s analysis and multiple logistic regression analysis were used to show relations between variables. Socio-demographic status, such as age and gender, proved to be important in self health assessment. Other factors affecting self health assessment included the number of family members, daily life and lifestyles, social environment, community motivation, and utilization of health services. Women, the elderly, or people with less-thannormal access to information suffer from poor self-assessed health. People who are socially inactive and who have poor living conditions are less likely to use health care services and are likely to assess their health as “poor”. In order to reduce the poor self-assessed health status it is important to address disparities in socioeconomic factors, such as age, gender, employment, and residential area. In addition, more attention should be paid to community and health services, as well as to health promotion and empowerment activities, including income-generation activities. Further research is also needed, however, for better understanding of about the local people and their health-related issues.
1. INTRODUCTION
Self-assessed health (SAH) is a simple measurement derived from gathering data in research, and in the scientific literature, SAH is also referred to as self-rated, self-perceived, or self-reported health. Although some doubts remain concerning this single measure [1,2], SAH indicators are widely used in international studies, especially in the developed world. A large number of studies present the relationship between SAH and other healthrelated aspects, including health conditions, medical diagnoses, psychosocial, and emotional status. In several studies, the relationship between mortality risks or morbidity has been studied extensively [3-6]. For example, a meta analysis from Karen De Salvo et al. suggested that “poor” SAH carries a two times higher mortality risk than an “excellent” self-assessment [7]. Additionally, some studies have shown a relationship between selfassessed health and other health aspects, such as physical health problems, physiological factors, long-standing illness, or functional capacities [8-10]. Some studies have also confirmed that such aspects as life or health service satisfaction, stress, social role, and health behavior are significantly related to SAH [11-14].
Other studies have included socio-demographic and socioeconomic inequalities with the SAH. Many studies have shown that SAH depends on gender, age, and income. Individuals with higher socio-demographic and economic status usually have better health than others do [15-18]. Even though many studies have been conducted to determine the factors of self health assessment, there is still a need to identify the local aspects of SAH in the developing world. In this article, we explored the associations among various factors influencing self health assessment in Ulaanbaatar, Mongolia.
Mongolia is the least densely populated country in the world with a population of 2.7 million people. About 63% of the total population of Mongolia lives in urban areas, including the capital city of Ulaanbaatar and other medium-sized and small towns. The remaining population lives as nomadic herders in the countryside. More than 1.1 million residents live in Ulaanbaatar [19] and the migration stream to Ulaanbaatar is increasing year by year. About 40% of the city population lives in apartment buildings, and the remaining residents dwell in a periurban area called the ger (traditional felt dwelling) districts, which lack modern infrastructure and where household incomes are 43% lower than those in urban households [20]. This kind of inhomogeneous society, with its high levels of inequality, and the considerable rise in the population of Ulaanbaatar create social and health problem. Since the end of the socialist regime, people’s lifestyle and health behavior has altered dramatically toward physical and social inactivity [21]. However, life expectancy at birth has increased in the past few years (in 2009, the life expectancy at birth was 65 years for men and 74 years for women) [22], even though adult mortality rates are rising, especially the male adult mortality rate. Cardiovascular disease, cancer, and injuries have been the leading causes of death in the last 10 years [23]. These high rates of lifestyle-related diseases have increased rapidly because of urbanization, physical activity, nutrition, and tobacco and alcohol use. Today, family practitioners deliver primary health care, services, and preventive care. Although the standard of Family Group Practice specifies one family practitioner per 1300 people, in actuality this number is doubled per family practitioner [24]. Therefore, because of work overload, family group practitioners cannot provide such services as prevention, advocacy, and training.
For reducing diseases and improving health care services among the local residents, practices need to enhance primary health care, health services, health promotion, and health education activities. Policymakers should also be aware of the results of health-related research, considering it when making and planning medical services and formulating health care policies.
This study also investigates whether differences may exist between societies having different cultures. Residents in Mongolia are ethnically homogeneous and have a nomadic and Buddhist culture. Therefore, some differences in self health assessment may exist as compared to that of other nations. Some previous studies have also noted that cultural differences between countries may influence health evaluation [25,26].
2. METHODS
2.1. Study Population and Data Collection
Five hundred respondents living in urban and periurban communities in Ulaanbaatar, Mongolia, were selected for this survey. The respondents were surveyed through a paper-based questionnaire, and all participants were adults aged 18 years or over. The questionnaire included such aspects as SAH status, social environment, community motivation, and utilization of health services. Information on socio-demographic conditions and daily life and life-style were also collected. The set of socio demographic variables included gender, age, education, employment, marriage status, and household size. The daily life and life-style factors included experiences in using media, hobbies and other free time use, physical exercise, self-perceived quality of life, and smoking and drinking habits. The set of social environment variables included satisfaction with the residential area, community motivation, and duration of residence in one place. The measures of health service utilization included medication usage, periodic health exams, health-seeking behavior, and hospital service cost.
The sampling method was based on the area sampling approach. In the first stage of sampling, Ulaanbaatar city was chosen, which consists of 45% of all resident population of Mongolia [27]. In the second stage, three districts within the city were purposely selected because of their density and the centralization. In the last stage, households were randomly selected. Within the household, Kish tables, which provide equal probability, were used for selecting respondents. Every respondent represents one household.
2.2. Data Analysis
Self-assessed health was the key dependent variable and it was measured through a single question, “How is your health in general?” with the response categories of “very good” (1) “good” (2) “fair” (3) “bad” (4) or “very bad” (5). We included four groups of confounders in the analyses: socio-demographic variables, daily life and lifestyle factors, social environment, and health service status and utilization.
Only the factors that met the statistical significant level in the Spearman correlation analysis were put into the multivariate logistic analyses. For the multivariate logistic analyses, we dichotomized the dependent (1, 2) versus (3, 4, and 5) and independent variables into 2 categories. All relationships were presented with 95% confidence intervals (CIs), and two-sided p-values of less than 0.05 were considered to be significant. The missing data is excluded from the analyses; thus, the final analytic sample size was 457 respondents. The data was entered into data analysis software, the Statistical Analysis System (SAS 9.1).
3. RESULTS
3.1. Demographic Characteristics of the Participants
The demographic characteristics of the respondents are presented in Table 1. A majority of the respondents were women (60.0% versus 40.0%). The respondents’ age span was from 18 to 83 years and the median age of the respondents was 35 years. Respondents aged 60 and over constituted 8.5% of the total. Most of the respondents were married (68.0%). The proportion of participants with a high school education (high school graduates, 206 or 45.0%) and higher education (college graduates and beyond, 149 or 32.6%) was quite high. Regarding employment status, 14.9% of the respondents indicated that they were unemployed, and the rest of the respondents were students, pensioners, and employees. The largest proportion assessed their health as good (47.1%) or fair (36.5%), with much smaller percentages for poor or very poor (9.6%) and very good (6.8%).
3.2. Statistical Analyses
According to the Spearman analysis, several significant correlations exist between SAH and the other aspects (Table 2). From the set concerning socio-demographic status, age (r = 0.30, p < 0.001) had a strong correlation with SAH. The next considerable factors were household size (r = 0.14, p = 0.002), gender (r = 0.14, p = 0.004) employment (r = 0.11, p = 0.016), and education (r = 10, p = 0.038). Marital status showed a negative correlation with the SAH (r = –0.11, p = 0.022), as unmarried persons had a significantly better SAH than married ones. Some of the factors related to daily life and lifestyles were also significantly correlated with SAH. One interesting finding concerns the Internet: those who use the Internet had self-assessed good health compared to people who did not use the Internet (r = 0.32, p < 0.001). In addition, persons who use the radio (r = 0.15, p = 0.002) and read magazines (r = 0.13, p = 0.004) had better SAH. Greater life satisfaction was associated with significantly better SAH (r = 0.17, p = 0.001). Those who exercise (r = 0.16, p = 0.001) and do not smoke (r = 0.13, p = 0.005) were significantly associated with good SAH. People without regular lifestyles were likely to

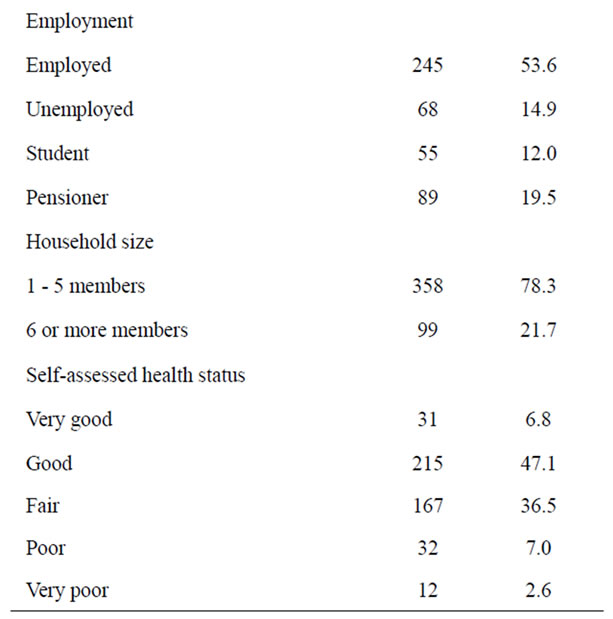
Table 1. General characteristics of the survey respondents.
have good health (r = –0. 25, p < 0.001). Some correlations were observed between SAH and social environment factors, such as duration of residents in one place (r = –0.21, p < 0.001) and drinking problems in the local area (r = 0.12, p = 0.013). Correlations were also observed in the set of community motivation. For example, respondents who had participated in physical activities during the past 30 days (r = 0.19, p < 0.001) and who had

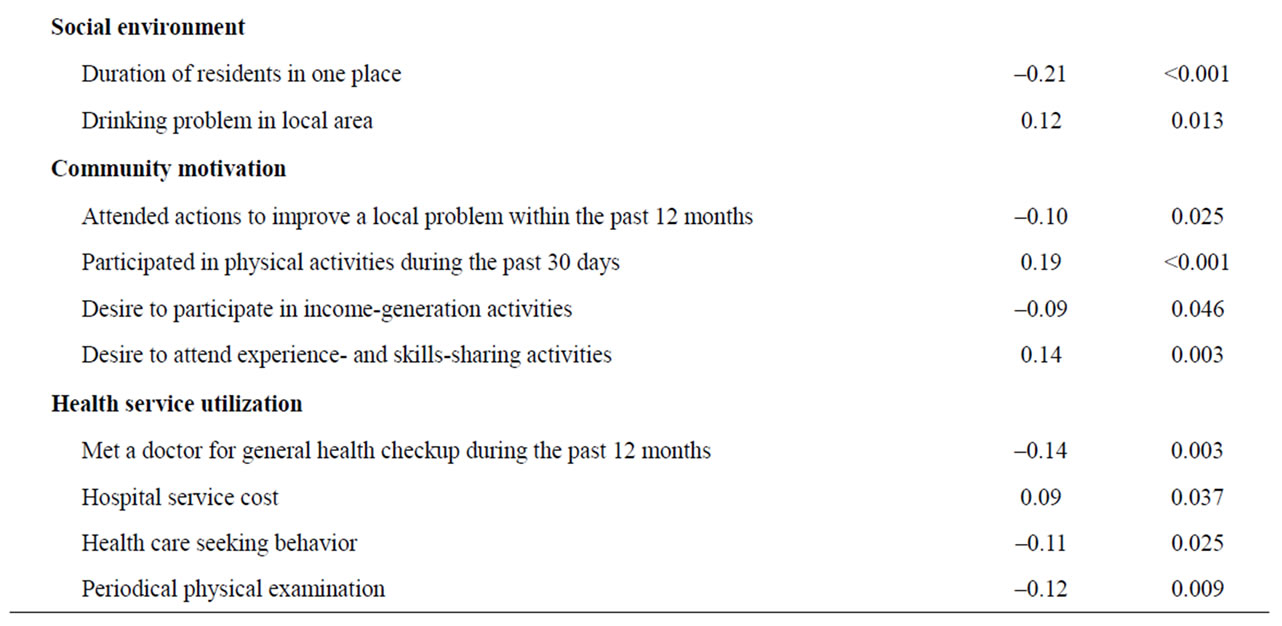
Table 2. Relationship between self-assessed health and subgroups (Spearman’s analysis).
a desire to attend experience and skills sharing activities (r = 0.14, p = 0.003) were likely to assess their health as good. Some negative correlations were also observed between community motivation and SAH. The persons who participated in actions to improve local problems (r = –0.10, p = 0.025) and who had a desire to participate in income-generation activities (r = –0.09, p = 0.046) were likely to assess their health as poor. Some negative correlations were found in terms of health service use. Persons who had periodic physical examinations (r = –012, p = 0.009), and who had met a doctor for their general health within the last 12 months (r = –0.14, p = 0.003) were likely to assess their health as poor. Persons who think that hospital service is expensive were also likely to assess their health as poor (r = 0.09, p = 0.037). The interaction between variables were also tested (Table 3). However some statistically significant relationships were existed between variables, this study revealed the independently related factors to SAH. Table 4 presents the odds ratios (ORs) for socio demographic status, factors of daily life and lifestyles, social environment, community motivation, and health service utilization. Age (OR = 5.78, CI: 1.92 - 16.5), gender (OR = 1.81, CI: 1.09 - 3.00), and household size (OR = 1.75, CI: 1.01 - 3.02)
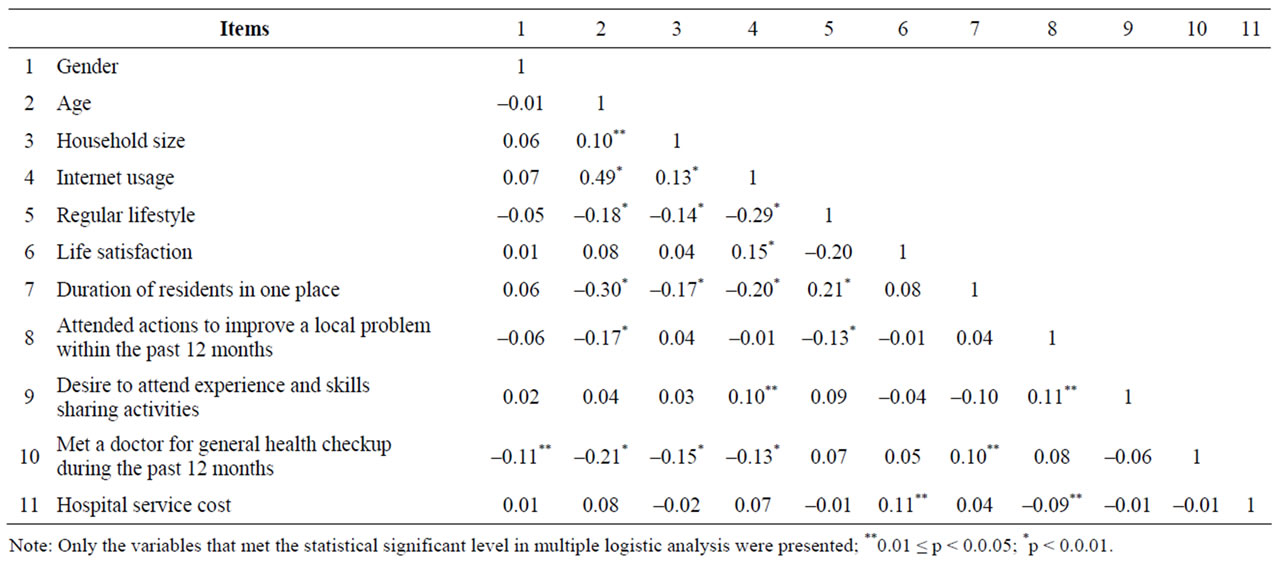
Table 3. Correlation between subgroups (Spearman’s analysis).
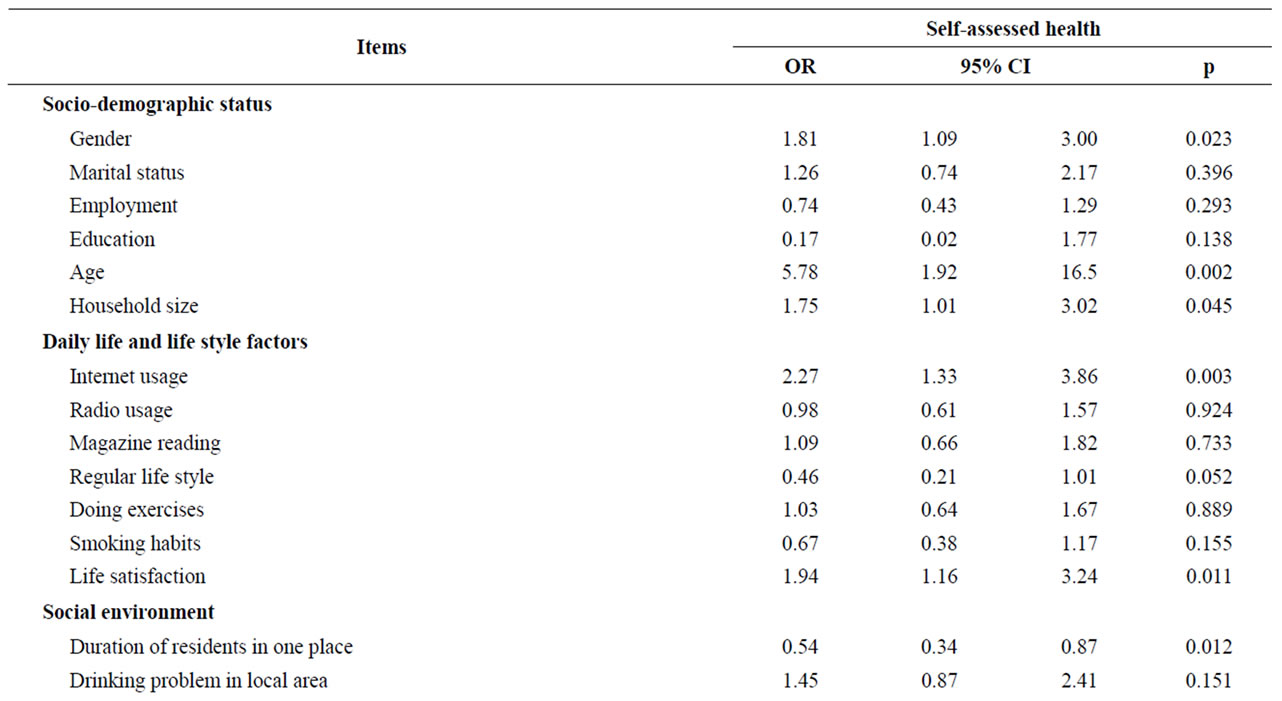
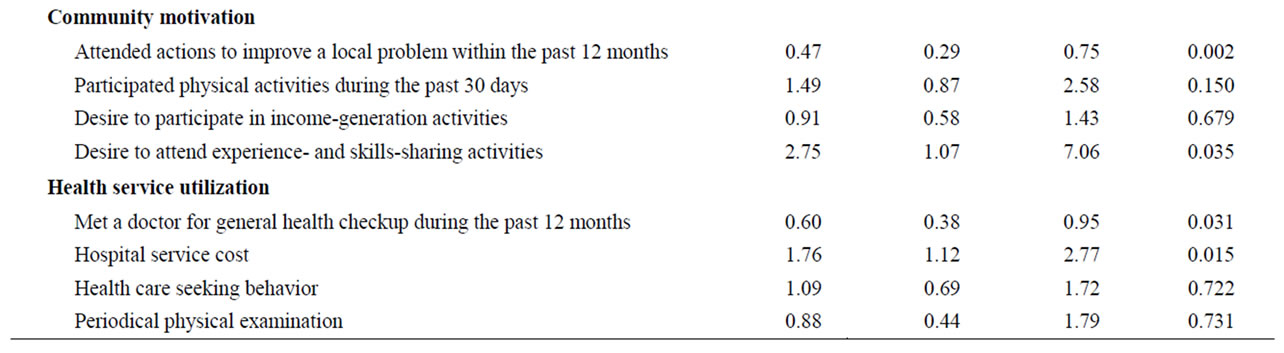
Table 4. Factors related to self-assessed health (multiple logistic regression analysis).
were significantly associated with SAH. Also using the Internet (OR = 2.27, CI: 1.33 - 3.86) and life satisfaction (OR = 1.94, CI: 1.16 - 3.24) were statistically associated with SAH in the set of daily life and lifestyle factors. Persons who had stayed in one place for more than 10 years assessed their health as good (OR = 0.54, CI: 0.34 - 0.87). Those who had attended community actions within the past 12 months to improve their local area assessed their health as poor (OR = 0.47, CI: 0.29 - 0.75). The people who desire to attend experience and skillssharing activities rated their health as good (OR = 2.75, CI: 1.07 - 7.06). The analyses also showed that those who had seen a doctor within the past 12 months were independently associated with SAH (OR = 0.60, CI: 0.38 - 0.95). Furthermore, hospital service cost was significantly related to the SAH (OR = 1.76, CI: 1.12 - 2.77).
4. DISCUSSION
In the developing world, use of SAH as a measure in research is not common; therefore, in general the literature does not contain much on this topic. The first benefit of this study is that it included adult populations in the urban and peri-urban area of Mongolia, one of the developing countries in central Asia. Second, it examined the aspects associated with SAH status among the participants in the local area, which is the first in the country to report SAH and its determinants.
We found that several aspects are associated with SAH. First, there was a significant association between sociodemographic status and self health assessment. In particular, SAH depended upon age and gender, as shown in other studies [13,16]. As the age increased, the participants were less likely to assess their health as “good.” After age 60, SAH declined for both men and women. Although lower SAH among the elderly may reflect physical functions and changes, it is nonetheless beneficial to promote a healthier lifestyle and empowerment programs for the local community, especially for the older populations in urban and peri-urban areas in Mongolia. The other noteworthy finding was related to gender, which affects SAH. The disparity in the life expectancy of the sexes in Mongolia is very high, as females are expected to live about nine years longer than males [22]; therefore, women were more likely to report poor health compared with men. This suggests that gender inequalities may exist in health care in Mongolia. Furthermore, attention should be paid to other social affairs of women and the local community, such as access to health-related information, health services, and social welfare. On the other hand, lifestyle habits and the roles of women and men in the family and society may influence the self health assessment; hence, this aspect needs further examination. Household size was also important to SAHas the respondents with five or more family members were more likely to report their health as poor. Although the average family size has dropped over the past few decades, poor families often want more children and have larger family sizes than middle-income or richer families in Mongolia. Large family size has been considered one of the causes of poverty in developing countries [28]; thus, for improving health status among poor families, improvement is needed in prevention activities, health services—especially reproductive health services— and in addressing gender inequalities and inadequate information. However, the multiple logistic analyses showed that age, gender, and household size have a significant relationship with SAH, as well as employment, education, and marital status. Poor self health assessment is correlated to unemployment and poor education, as in other studies [15,29]. We also found that non-married people were healthier than those who are married. This finding may be because most of the non-married respondents were young people in this study, and there may also be cultural and social reasons among married people, such as the living conditions of the families, household sizes, and culture-oriented marital duties.
Second, some aspects related to daily life and lifestyle factors also had a significant relationship with SAH in this study. Respondents who use the Internet, listen to the radio, and read magazines have a higher SAH. According to the 2010 Population and Housing Census of Mongolia, 30.6% of the total population uses the Internet regularly [27]. However, in Mongolia, Internet service is still limited in some areas, especially peri-urban and rural areas. Hence, people who have better living conditions can access the Internet and get more information than others can. Also among older people, the level of Internet and computer usage is very low. In addition, we found a relationship between SAH and life satisfaction. The people who have better SAH enjoy their lives more than those who have poor self health assessment. The next factor that correlated with SAH was regular lifestyle. In Mongolia, people’s lifestyles have changed dramatically since the collapse of the socialist regime in 1990. Many people have become more physically inactive, with accompanying poor health habits, and not many communitybased organizations exist, especially for the unemployed and the elderly [21]. These factors may explain the result that people who do not have regular lifestyles, but who are active have better SAH than those who have regular lifestyles. Even though a healthier life—such as having a regular lifestyle, exercising, and not smoking—correlated with better SAH, these factors were not proven as predictors of SAH by the multiple logistic analyses in this study.
Third, we found that the persons who do not live more than 10 years in one place demonstrated poor health. The population in Ulaanbaatar increased by 31% from 2000 to 2007. People who migrated into the capital city usually settled into peri-urban areas, and life was not secure for many of them [30]. The migrants, especially those who live in peri-urban areas, may need attention as they are more likely to suffer from SAH.
Furthermore, community motivation, such as attending community activities and having a desire to attend experienceand skills-sharing activities showed a significant relationship with SAH. From these findings, we may deduce that the people who suffered from poor SAH had not attended actions to improve local problems within the past year. Other studies have also found that social participation is important for health and that people who attend more social activities tend to report better health [31]. The people who have better SAH also have a desire to attend experienceand skills-sharing activities compared to the people who suffer from poor SAH.
Last, but not least, it should be noted that some factors related to health service utilization also have a significant relationship with SAH. In particular, the people who had been to a doctor for a general health checkup during the preceding 12 months had poorer health than others, and poor SAH also correlated to periodic physical exams. This finding implies that among the local residents, health promotion and health prevention activities are not promoted and that only those who have poor health use hospital services. In addition, we found that poor SAH and high costs for hospital service were related. This finding may indicate that it is still hard for people with low income to get health care services compared with high-income residents.
This study has some limitations: first, we did not consider hospital-diagnosed morbidity and medical conditions. Second, income was not included in the analysis, because household income was missing for a substantial minority of the study sample. Third, we did not assess children’s status, as the survey did not include children under age 17. Finally, we chose SAH as a dependent variable.
5. CONCLUSIONS
The present study analyzed the particular aspects that affect SAH in Mongolia. Although, the sample size was relatively small, the study findings were important, a step toward identifying the aspects involved in self health assessment. In addition, the results of this study may reveal the population health status.
In order to reduce the gap in health status, it is important to address disparities in socioeconomic factors, such as age, gender, employment, and residential area. The level of disease prevention and periodic exams is very low in the community, and to improve SAH, more attention should be paid to community and health services, as well as to health promotion and empowerment activities, including income-generation activities. Finally, we suggest that because there is still much to do, these kinds of studies should be continued in Mongolia in order to provide understanding of the mechanisms that affect poor SAH in both urban and rural areas.
6. ACKNOWLEDGEMENTS
We thank all the study participants and all our lab members, who participated and collaborated in this study. Their comments and suggestions were very valuable.
![]()
![]()
REFERENCES
- Subramanian, S.V., Huijts, T. and Avendano, M. (2010) Self-reported health assessments in 2002 World Health Survey: How do they correlate with education? Bulletin of the World Health Organization, 88, 131-138. doi10.2471/BLT.09.067058
- Jürges, H., Avendano, M. and Mackenbach, J.P. (2008) Are different measures of self-rated health comparable? An assessment in five European countries. European Journal of Epidemiology, 23, 773-781. doi10.1007/s10654-008-9287-6
- McFadden, E., Luben, R., Bingham, S., Kinmonth, A.L. and Khaw, K.T. (2009) Does the association between selfrated health and mortality vary by social class? Social Science and Medicine, 68, 275-280. doi10.1016/j.socscimed.2008.10.012
- Benjamins, M.R., Hummer, R.A., Eberstein, I.W. and Nam, C.B. (2004) Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Social Science and Medicine, 59, 1297-1306. doi10.1016/j.socscimed.2003.01.001
- Liavaag, A.H., Dørum, A., Fosså, S.D., Tropé, C. and Dahl, A.A. (2009) Morbidity associated with “self-rated health” in epithelial ovarian cancer survivors. BMC Cancer, 9, 2. doi10.1186/1471-2407-9-2
- Idler, E.L. and Benyamini, Y. (1997) Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21-37. doi10.2307/2955359
- De Salvo, K.B., Bloser, N., Reynolds, K., He, J. and Muntner, P. (2005) Mortality prediction with a single general self-rated health question: A meta-analysis. Journal of General Internal Medicine, 20, 267-265.
- Arnadottir, S.A., Gunnarsdottir, E.D., Stenlund, H. and Lundin-Olsson, L. (2011) Determinants of self-rated health in old age: A population-based, cross-sectional study using the international classification of functioning. BMC Public Health, 11, 670. doi10.1186/1471-2458-11-670
- Mackenbach, J.P., Simon, J.G., Looman, C.W.N. and Joung, I.M.A. (2002) Self-assessed health and mortality: Could psychosocial factors explain the association? International Journal of Epidemiology, 31, 1162-1168. doi10.1093/ije/31.6.1162
- Manor, O., Matthews, S. and Power, C. (2000) Self-rated health and limiting longstanding illness: Inter-relationships with morbidity in early adulthood. International Journal of Epidemiology, 30, 600-607. doi10.1093/ije/30.3.600
- Sundaram, V., Helweg-Larsen, K., Laursen, B. and Bjerregaard, P. (2004) Physical violence, self rated health, and morbidity: Is gender significant for victimisation? Journal of Epidemiology and Community Health, 58, 65-70. doi10.1136/jech.58.1.65
- Ford, J., Spallek, M. and Dobson, A. (2008) Self-rated health and a healthy lifestyle are the most important predictors of survival in elderly women. Age and Ageing, 37, 194-200. doi10.1093/ageing/afm171
- Piko, B. (2000) Health-related predictors of self-perceived health in a student population: The importance of physiccal activity. Journal of Community Health, 25, 125-137. doi10.1023/A:1005129707550
- Siahpush, M., Spittal, M. and Singh, G.K. (2008) Happiness and life satisfaction prospectively predict self-rated health, physical health, and the presence of limiting, longterm health conditions. American Journal of Health Promotion, 23, 18-26. doi10.4278/ajhp.061023137
- Mackenbach, J.P., Stirbu, I., Roskam, A-J.R., Schaap, M.M., Menvielle, G., Leinsalu, M. and Kunst, A.E. (2008) Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine, 358, 2468-2481. doi10.1056/NEJMsa0707519
- McFadden, E., Luben, R., Bingham, S., Wareham, N., Kinmonth, A.L. and Khaw, K.T. (2008) Social inequalities in self-rated health by age: Cross-sectional study of 22457 middle-aged men and women. BMC Public Health, 8, 230. doi10.1186/1471-2458-8-230
- Singh-Manoux, A., Dugravot, A., Shipley, M.J., Martikainen, P., Goldberg, M. and Zins, M. (2007) The association between self-rated health and mortality in different socioeconomic groups in the Gazel cohort study. International Journal of Epidemiology, 36, 1222-1228. doi10.1093/ije/dym170
- Kennedy, B.P., Kawachi, I., Glass, R. and Prothrow-Stith, D. (1998) Income distribution, socioeconomic status, and self rated health in the United States: Multilevel analyses. British Medical Journal, 317, 917-921. doi10.1136/bmj.317.7163.917
- Statistical Yearbook 2009 (2009) National Statistic Office of Mongolia. http://www.nso.mn/v3/
- Kamata, T., Reichert, J.A., Tsevegmid, T., Kim, Y. and Sedgewick, B. (2010) Enhancing policies and practices for ger area development in Ulaanbaatar. The World Bank Report, Washington DC.
- Gan-Yadam, A., Tanaka, E., Sugisawa, Y., Watanabe, T., Tong, L., Shinohara, R., Hirano, M., Tomisaki, E., Motita, K., Onda, Y., Kawashima, Y., Mochizuki, Y., Nanba, M. and Anme, T. (2011) Gender differences in health seeking behaviour and empowerment needs. Japanese Journal of Human Sciences of Health-Social Services, 18, 52-58.
- WHO (2011) WHO Report, World Health Statistics. http://www.who.int/healthinfo/statistics/mortality_life_tables/en/
- Asian Development Bank (2008) Mongolia: Health and social protection. http://www.oecd.org/dataoecd/33/32/42227662.pdf
- Ministry of Health Mongolia (Third Health Sector Development Project) (2009) Legal Analysis for Status of Family Group Practice. http://www.hsdp.moh.mn/eng/Downloads/File/huvi/Report%20of%20legal%20analysis%20on%20status%20of%20FGP_eng.pdf
- Kunst, A.E., Bos, V., Lahelma, E., Barley, M., Lissau, I., Regidor, E., Mielck, A., Cardano, M., Dalstra, J.A.A., Guerts, J.J.M., Helmert, U., Lennartsson, C., Ramm, J., Spadea, T., Stronegger, W.J. and Mackenbach, J.P. (2005) Trends in socio-economic inequalities in self assessed health in ten European countries. International Journal of Epidemiology, 34, 295-305. doi10.1093/ije/dyh342
- Zimmer, Z., Natividad, J., Lin, H. and Chayovan, N. (2000) A cross-national examination of the determinants of selfassessed health. Journal of Health and Social Behavior, 41, 465-481. doi10.2307/2676298
- National Statistic Office of Mongolia (2010) Population and Housing Census of Mongolia 2010. http://www.toollogo2010.mn/index.php?language=en
- Lanjouw, P. and Ravallion, M. (1995) Poverty and household size. Economic Journal, 105, 1415-1434. doi10.2307/2235108
- Kaleta, D., Makowiec-Dabrowska, T. and Jecier, A. (2008) Employment status and self rated health. International Journal of Occupational Medicine and Environment Health, 21, 227-236. doi10.2478/v10001-008-0023-y
- Anqing, S. (2011) Rural out-migration and family life in cities in Mongolia. East Asian and Pacific Region/CMU. The World Bank, Washington DC. http://www-wds.worldbank.org/external/default/WDSContenServer/WDSP/IB/2011/11/02/000333037_20111102005453/%20Rendered/PDF/651590WP0P12230on0v20final00PUBLIC0.%20pdf
- Lee, H.Y., Jang, S.-N., Lee, S., Cho, S.-I. and Park, E.-O. (2008) The relationship between social participation and self-rated health by sex and age: A cross-sectional survey. International Journal of Nursing Studies, 45, 1042-1054. doi10.1016/j.ijnurstu.2007.05.007

