Surgical Science
Vol. 3 No. 3 (2012) , Article ID: 18043 , 10 pages DOI:10.4236/ss.2012.33029
Management of 634 Consecutive Patients with Chronic Pilonidal Sinus: A Nine-Year Experience of a Single Institute
1Department of Surgery, University of Alexandria, Alexandria, Egypt
2Surgical Division, Ahmadi Hospital, KOC, Ahmadi, Kuwait
3Department of Surgery, Faculty of Medicine, Ain-Shams University, Cairo, Egypt
4Department of Surgery, Medical Research Institute, University of Alexandria, Alexandria, Egypt
Email: mah_sakr@yahoo.com
Received October 11, 2011; revised October 29, 2011; accepted December 21, 2011
Keywords: Pilonidal Sinus; Chronic; Karydakis; Midline Closure; Recurrence
ABSTRACT
Objectives: Different surgical techniques, with variable morbidity and recurrence rates, have been advocated for the management of chronic pilonidal sinus (PNS). This study was conducted to report the outcome of surgical treatment of 634 cases of chronic PNS at a single institute between January 2001 and January 2010. Methods: Karydakis flap was performed in 244 patients (38.5%, Group 1). Excision and midline closure was performed in 371 patients (58.5%, Group 2), while the open method was used in 19 (3.0%). Data regarding patient and sinus characteristics, operative details, postoperative course, complications and recurrence were recorded. Mean follow-up was 73.5 months. Results: 571 patients were male (90.1%) and 63 were female (9.9%). Their ages ranged between 16 - 44 years (mean 25.7 years). The mean body mass index was 31.2 (range 23.6 - 41.9), and 71.5% (453/634) were hirsute. Chronic PNS was the first presentation (primary) in 504 patients (79.5%) and recurrent in 130 (20.5%).Overall complication rate was 16.1% (102/ 634) and overall recurrence rate was 8.4% (53/634). Comparing both groups showed that they were similar regarding demographic characteristics, clinical presentation, hospital stay, healing time and time off work. Operative time was insignificantly longer with Karydakis technique (mean 43.2 versus 39.1 minutes, respectively). Complications were significantly more in patients with midline closure (21%, 78/371) as compared with Karydakis procedure (9%, 22/244) (P = 0.0001). Likewise, there was a significantly (P = 0.0001) higher rate of recurrence with midline closure (12.1%, 45/371) as opposed to Karydakis technique (2.5%, 6/244). Conclusions: 1) PNS affects mainly young male adults who are usually, obese and hirsute, 2) Karydakis technique for the management of chronic PNS, whether primary or recurrent, is a non-lengthy, efficient procedure that has less overall complications and a lower recurrence rate than conventional excision and midline closure.
1. Introduction
Chronic pilonidal sinus (PNS) is a common disabling disorder that affects mainly young adults [1]. It has a high incidence in some countries, particularly in the Middle East and Gulf region owing to differing hair characteristics and growth patterns [2-4]. Today’s most widely accepted explanation for the pathogenesis of PNS was suggested by Karydakis [3] who attributed the occurrence of PNS to three main factors: the invader (loose hair), the force (causing insertion) and the skin vulnerability (depth of the natal cleft).
Despite the variety of surgical techniques proposed for the management of chronic PNS, the best method is still controversial. Surgery should not only eradicate the existing sinus and the crevice in which hair tends to accumulate, but also aim to establish complete and rapid primary healing and to prevent recurrence [5,6]. The ideal operation should also be simple, require short hospitalization, cause minimal morbidity, and allow rapid return to work and normal activities [7].
The present study was conducted to explore the clinical features of adult patients (>16 years) with chronic PNS admitted to Ahamdi Hospital, Kuwait (secondary care hospital) over a period of 9 years, and to report the outcome of surgical treatment of their disease.
2. Patients and Methods
2.1. Study Population
Between January 2001 and January 2010, 801 patients with PNS were treated at Ahmadi Hospital. Patients who were under the age of 16 years (n = 7) and those who presented with acute pilonidal abscess (n = 160) were excluded from the study. The remaining 634 adult patients presented with chronic (>3 months) PNS and represent the population of this study. Body mass index (BMI) was used as an objective indicator of obesity, according to the WHO anthropometric criteria for health [8], as follows: a BMI of 25 - 29.9 is overweight (grade 1), 30 - 39.9 is obesity (grade 2) and ≥40 is morbid obesity (grade 3). Patient disposition is shown in Figure 1.
2.2. Data Collection
Data regarding patient demographics, BMI, history, clinical presentation, sinus characteristics, previous management, operative details, post-operative course (duration of hospital stay, time from the day of surgery to resumption of work or daily activities, complications and recurrence of disease), and duration of follow-up, were retrospectively collected using hospital computer records, as well as theatre and first author’s log books.
2.3. Surgical Procedures and Post-Operative Regimen
Karydakis technique (eccentric flap) [3,9] was performed in 244 patients (Group 1), while sinus excision, through a midline elliptical incision, was performed in 390 patients, with direct primary closure (closed technique) in 371 (Group 2), and healing by secondary intention (open technique) in only 19. All procedures were performed under general anesthesia (patient preference/cultural factor) with the patient in the prone position and the buttocks strapped apart. One dose of intravenous second generation cephalosporin was given to all patients with induction of anesthesia. Apart from patients treated with the open technique, suction drains were routinelyused
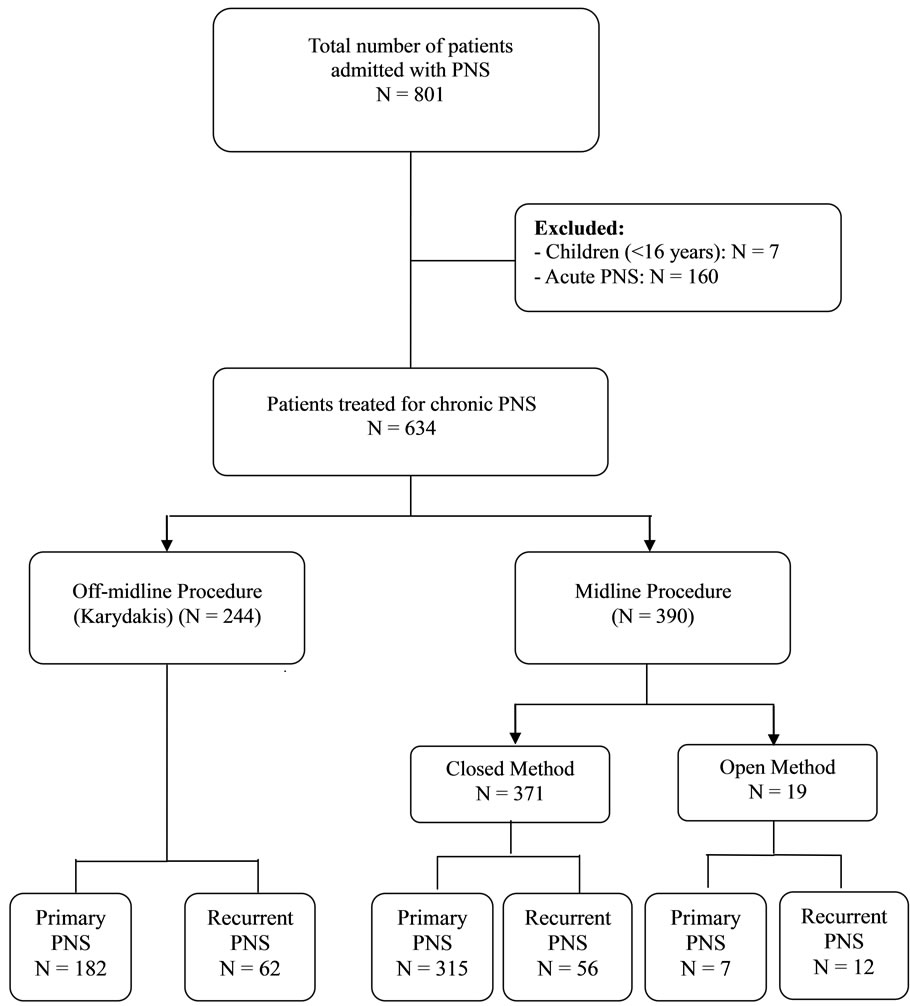
Figure 1. Patient flow diagram.
through separate stab incisions.
Post-operatively, patients were nursed supine and kept in bed for 1 - 2 days to help hemostasis by direct pressure. Antibiotics were not prescribed routinely. Patients were usually discharged from the hospital on the 2nd or 3rd day post-operatively (after drain removal), with emphasized instructions regarding personal regional hygiene and hair depilation. Sutures were removed after 10 - 12 days. Follow-up visits were scheduled at regular twoto fourweek intervals for the first 8 weeks, and at 3-month intervals thereafter for 12 months for monitoring of postoperative complications and recurrence. Patients were then reviewed yearly or earlier in case of recurrence of symptoms. Mean follow-up after surgical treatment was 73.5 months (range 12 - 120 months).
2.4. Statistical Analysis
Statistical analysis was performed using the SPSS/PC version 13 computer software (Prentice-Hall; Chicago, IL). Patients who underwent midline excision and left open (n = 19) were not included in the comparisons due to their relatively small number. Accordingly, comparisons were made between Group 1 patients who underwent Karydakis technique (n = 244) and those of Group 2 who underwent excision and midline closure (n = 371). The students t test was used to compare the mean values between the two groups. The Chi square test with Yate’s correction was used for comparison between categoral qualitative values, and the Fisher’s exact test was used to compare recurrences. The 5% level was set as the level of significance.
3. Results
There were 571 men (90.1%) & 63 women (9.9%). Their ages ranged between 16 - 44 years with a mean of 25.7 years.The mean BMI of the study population was 31.2 (range 23.6 - 41.9), and 72.9% (462/634) of patients were hirsute in nature. Chronic PNS was the first presentation (primary) in 504 patients (79.5%) and recurrent in 130 (20.5%). The overall complication rate was 16.1% (102/ 634) and overall recurrence rate was 8.4% (53/634).
Of the 634 patients, 19 underwent excision and open technique, and were not included in comparisons due to their relatively small number (n = 19). Of the remaining 615 patients, 244 underwentKarydakis technique (Group 1) and 371 underwent midline closure (Group 2). Half of the patients (50%, 307/615) were obese [8], and approximately three quarters (73.6%, 453/615) had overabundance of hair (hirsute nature) [10]. History of smoking was documented in 50.2% of patients (309/615) and positive family history of PNS for first-degree relatives in only 16% (98/615). As seen in Table 1, no significant differences between the two groups were observed in any of the aforementioned patient characteristics in addition to age and gender. Likewise, Table 2 shows that both groups had similar clinical presentation and sinus characteristics with no statistically significant differences between them (P > 0.05). Primary PNS, as opposed to recurrent PNS, was the main clinical presentation in the two groups (74.6% versus 85.0%). Chronic
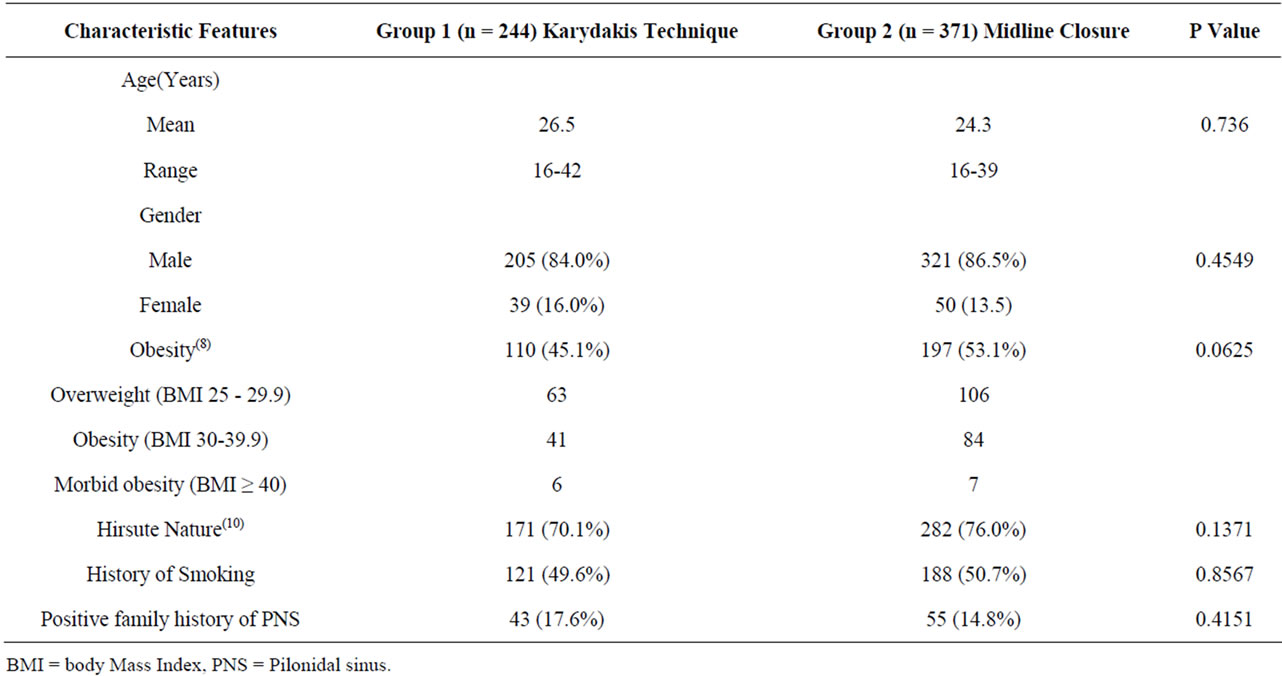
Table 1. Patient demographics and characteristics.
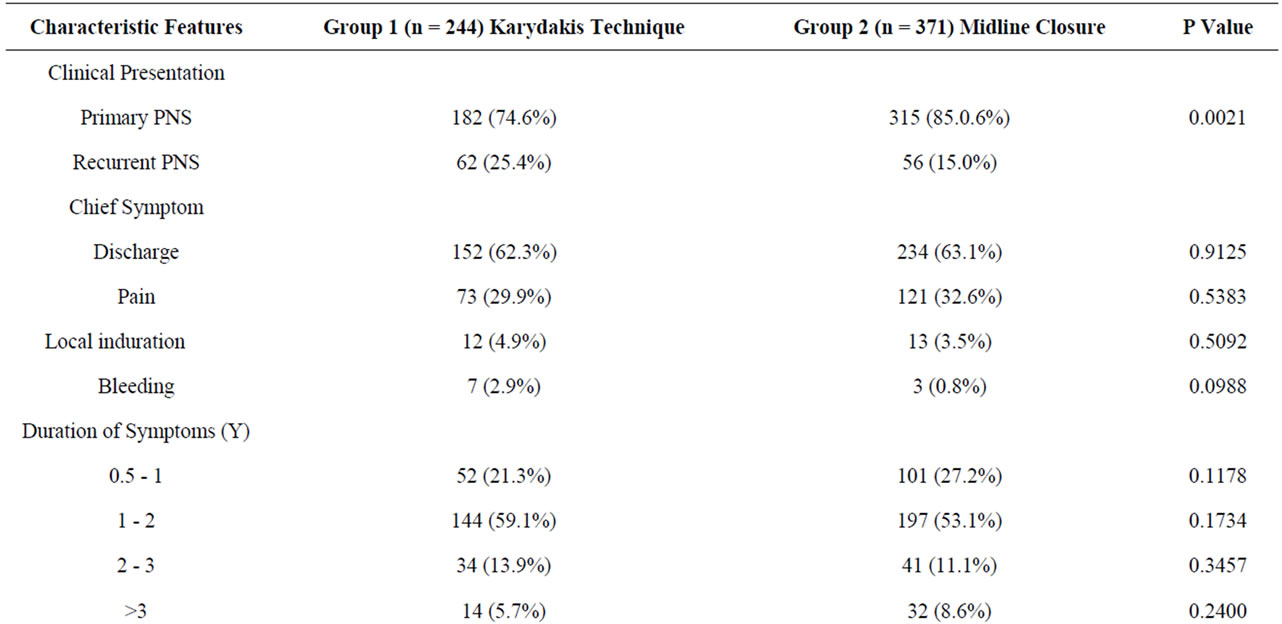
Table 2. Clinical presentation and sinus characteristics.
discharge was the main symptom in both groups (62.3% versus 63.1%) lasting mostly for 1 - 2 years. Multiple sinuses were encountered in the majority of patients (80% versus 86%, respectively), most commonly seen in the midline (51.2% versus 55.0%, respectively) (Figures 2(a) and (b)).
Table 3 shows that operative time was insignificantly longer with the Karydakis technique than with midline closure (mean 43.2 versus 39.1 minutes, respectively). Likewise, the two groups did not differ significantly from each other regarding the duration of hospital stay, time needed for complete wound healing, or required to resume work or normal physical activity. Overall complication rate was significantly lower in patients with Karydakis procedure (9%, 22/244) than those with midline closure (21%, 78/371) (X2 = 14.718, P = 0.0001). Wound infection and/or dehiscence (Figure 3) was seen in 13 patients (5.3%) in Group 1 as opposed to 47 (12.7%) in Group 2 (X2 = 8.194, P = 0.0042). Recurrence (Figure 4) was observed in 6 patients (2.5%) with Karydakis technique and in 45 (12.1%) with midline closure (P < 0.0001).
Table 4 summarizes the characteristics related to first surgery in patients who presented with recurrent PNS (n = 130). The mean age at first surgery was 22 ± 2.5 years. Regarding the type of surgery, most patients underwent excision and midline closure (75.4%) and 17.7% of patients underwent excision and open technique. Only 9 patients (6.9%) had 2 previous procedures. Wound complications after the primary surgery were recorded in approximately one third of the patients (36.2%), and most recurrences (105/130, 80.8%) were seen within the first 3 years post-operatively.
Figure 5 shows that the complication rate was significantly higher with midline closure as compared to Karydakis technique for patients with primary PNS (18.4%
 (a)
(a) (b)
(b)
Figure 2. (a) (b). Two different male patients with primary chronic PNS presenting with multiple midline sinuses. Note the presence of hair.
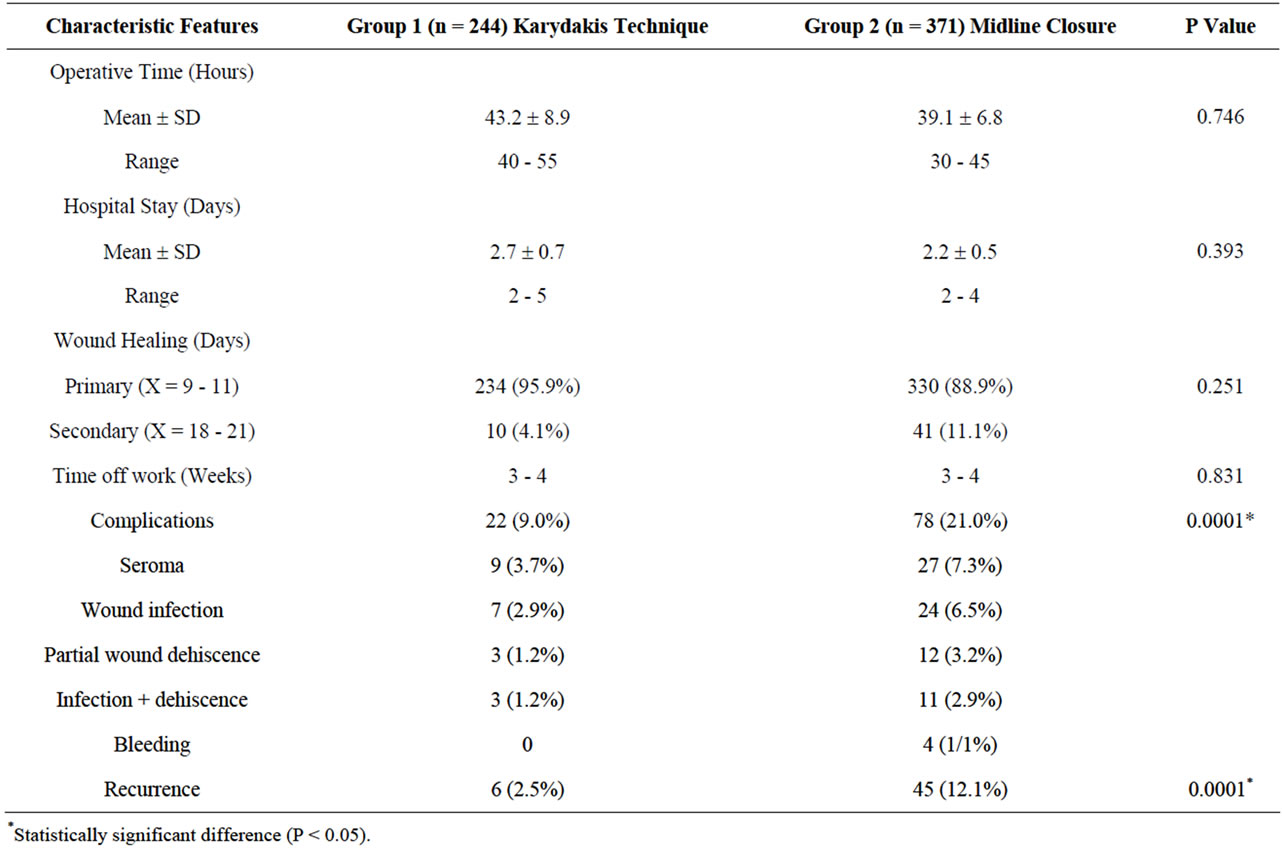
Table 3. Operative time and postoperative course.
(58/315) versus 8.2% (15/182), respectively) (X2 = 8.729, P = 0.0031) and also for those with recurrent PNS (35.7% (20/56) versus 11.3% (7/62), respectively) (X2 = 8.611, P = 0.0033). Similarly, as shown in Figure 6" target="_self"> Figure 6, the recurrence rate was significantly higher with midline closure than Karydakis technique for both primary PNS (11.4% (36/315) versus 2.2% (4/182), respectively, P = 0.0001) and recurrent PNS (16.1% (9/56) versus 3.2% (2/62), respectively, P = 0.0243). However, within the Karydakis Group, results were similar for both primary

Figure 3. A 24-year-old gentleman with partial wound dehiscence after sinus excision and midline closure. Note hirsute nature of the patient.

Figure 4. Recurrent chronic PNS (white arrow) in a 36- year-old female patient. Note the scar of previous surgery (midline closure)(red arrow).
and recurrent PNS in terms of complication rate (8.2% versus 11.3%, respectively) and recurrence rate (2.25 versus 3.2%, respectively). On the other hand, though patients with primary and recurrent PNS who underwent midline closure had similar recurrence rate (11.4% versus 16.1% respectively), yet those with recurrent disease had a significantly (X2 = 7.562, P = 0.0060) higher complication rate (35.7% (20/56) versus 18.4% (58/315).
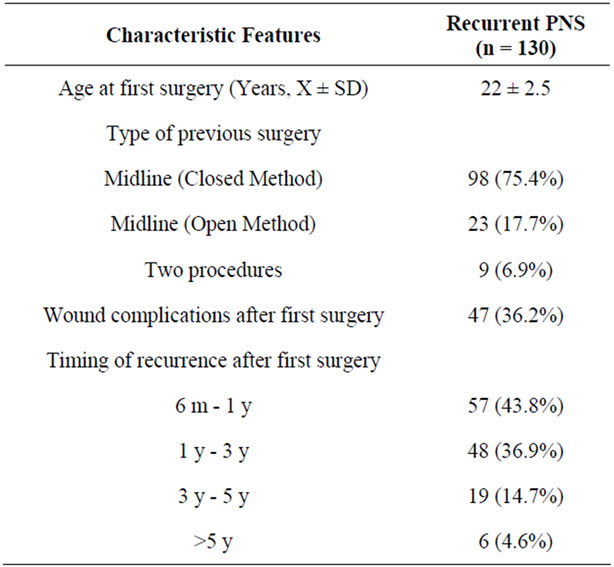
Table 4. Characteristics related to first surgery in patients who presented with recurrent PNS.
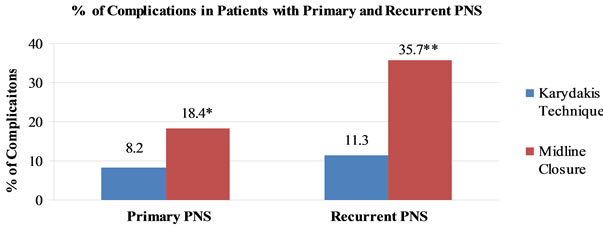
Figure 5. Bar chart showing the complication rate among patients with primary and recurrent PNS undergoing Karydakis technique versus excision and midline closure. Note significant differences between both groups (*X2 = 8.729, P = 0.0031, **X2 = 8.611, P = 0.0033).
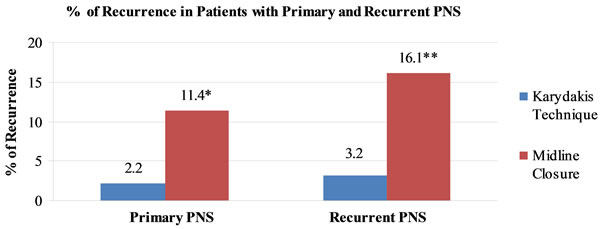
Figure 6. Bar chart showing the recurrence rate among patients with primary and recurrent PNS undergoing Karydakis technique versus excision and midline closure. Note significant differences between both groups (*P = 0.0001, **P = 0.0243).
4. Discussion
Initially thought to be congenital in origin, it is now appreciated that hair insertion not only causes PNS, but also prevents spontaneous recovery, delays healing, and is the main cause of recurrence [3]. The natural depth of the natal cleft is very vulnerable to hair insertion because of a number of congenital or acquired characteristics that vary widely from one person to another according to age, gender, race, body constitution and the type of operation performed previously [3]. The most obvious contributing factors to the high incidence of PNS observed herein were the hirsute body habitus of the population (mostly young men), poor personal hygiene, family history, and obesity which results in a tendency to increased depth of the natal cleft, increased friction, and a tendency to softness and maceration in depth. Obesity has been reported in the literature not only to predispose to the development of PNS [11], but also to be associated with prolonged surgery [12], longer hospital stay [12], higher postoperative complication [12], and recurrence rates [13].
Surgery for chronic PNS should not only eradicate the existing sinus and the crevice in which hair tends to accumulate, but also aim to eliminate factors that predispose to formation of other sinuses [3,12]. Day surgery with simple lay-open, curettage, brushing, or phenol injection may eliminate the hairs and cure the sinus but the midline wound may take several weeks to heal, and there is a significant recurrence rate because of the open portal for hair insertion [7]. Thus, the advantage of simple day surgery may be overweighed by the longer time to return to work and the greater likelihood of a further operation with longer hospitalization for recurrence.
For sinus excision through a midline approach, the wound can be primarily closed, marsupialized, or left open to heal by secondary intention [14]. Excision with an open wound involves prolonged hospitalization or clinic attendance for many painful dressings and takes months to heal. Both this method and excision with marsupialization leave a portal in the midline for further hair entry and have a significant recurrence rate [15-19]. Several studies have demonstrated superiority of excision with primary closure over excision with an open wound, by providing less bleeding, lower infection, reduced wound pain, fewer postoperative visits, shorter time off work, and faster healing time [16,18,20-22], albeit with a higher recurrence rate [23-25], reaching up to 50% [1,4,12,26,27]. Still however, midline excision and primary closure remains the most commonly adopted technique worldwide [28]. In the present study, recurrence rate with the closed method was 12.1% (45/371). After surgical excision, the base of the unhealed surgical wound is believed to become filled with granulation tissue, hair, and skin debris, which is a nidus for the ongoing foreign body reaction that takes place to create the chronic disease. The known predisposing intergluteal anatomy that draws hair into the PNS cavity or surgical wound, is also thought to precipitate the extensive chronic and recurrent disease.
A successful procedure for treating and preventing recurrence of PNS would therefore be one that results in removal (excision or displacement) of the vulnerable raphe, and avoidance of any wound scar in the depth of the intergluteal fold. It should also be as simple as possible to shorten the duration of in-hospital stay and minimize time off work. This is achieved by the asymmetric eccentric Karydakis flap, which reduces the depth of the natal cleft and ensures that all parts of the wound and all suture holes are away from the midline. In his own review of more than 6000 cases, Karydakis [3] demonstrated fast healing with a wound complication rate of 8% and recurrence rate of 2%. In this study, 95.9% of patients who underwent Karydakis operation had primary wound healing within 9 - 11 days and a hospital stay of about 3 days. Recurrence was observed in only 2.5% of patients, which is significantly lower than that observed with midline closure (12.1%). Likewise, Can et al. [6] who operated on 200 patients with PNS reported a 4.6% recurrence rate with Karydakis flap and 18.4% with midline closure. Akinci et al. [29] reported an even lower recurrence rate (0.9%) after Karydakis procedure in a large series of 112 patients. Patel and colleagues [30] using Karydakis’ method, avoided recurrence and unhealed midline wound, albeit with an inpatient stay of 5 days. Anyanwi et al. [31] treated also 28 patients by this procedure and reported no recurrences after a median follow-up of 3 years. Applying the same technique, both Kitchen [32] and Al-Jaberi [33] reported a recurrence rate of 4%. Moreover, Sakr et al. [12] reported a recurrence rate of 3.13% with the Karydakis flap used exclusively for obese patients and a hospital stay for a mean of 3.2 days.
In the present study, more postoperative complications were encountered in patients with midline closure mainly wound infection with or without wound dehiscence. Similar results of low complication rate with Karydakis method, though with a shorter period off-work (2 weeks) than that observed herein (3 - 4 weeks), were reported by other authors [30,31,33,34]. However, it is worth mentioning that neither of these two procedures offers any advantage over the other in terms of operative time, duration of hospital stay, time needed for wound healing, or to return to normal physical activity.
Numerous plastic flap-based procedures aimed at stopping hair insertion by flattening the natal cleft, including rotation flap, rhomboid flap, and Z-plasty were reported to provide a low recurrence rate [11]. Although beyond the scope of this study, it is noteworthy that Karydakis flap is simpler and does not require time-consuming, sophisticated surgery, extensive mobilization, or real transposition. Moreover, a trap for loose hair is created, especially at the lower part of the natal cleft, if these methods leave the lower part of the wound in the midline, together with an un-excised part of the vulnerable raphe [3].
Some of the variables associated with recurrence of PNS are believed to be related to the “patient” such as obesity, hirsute nature, smoking, positive family history, and age at first surgery. Other factors are related to the “primary procedure”, such as type of surgery, post-operative wound complications (mainly infection) and the timing of recurrence postoperatively [35]. All such variables were similar between the two groups under comparison, and so were the “sinus characteristics” that included the chief symptom, duration of symptoms, as well as location and number of sinuses. In 2010, Nursal et al. [36] reported that younger age, recurrent cases, sinus discharge on physical examination, and post-operative infection were independent predictors of recurrence. In addition, Cubukcu et al. [13] reported that obese patients have a higher risk of PNS recurrence; however, Doll et al. [37] did not find obesity to have any negative influence on recurrence rate, and emphasized that long-term recurrence rate was significantly elevated when family history was positive and when surgery was needed at a younger age. In this study, 43.81% of the patients admitted with recurrent PNS developed their recurrence within the first year post-operatively, and 80.7% by 3 years. Only 4.6% of recurrences occurred after 5 years. Similar to our findings, Doll et al. [38], who followed-up their patients for up to 20 years, reported that 71% of recurrences occur in the first 4 years post-operatively and recommended a follow-up of at least five years.
Relatively few data exist that focus on an optimal surgical approach that should be followed in cases of recurrent PNS [39]. In a previous communication, we reported that Karydakis technique was superior to midline closure for the management of chronic PNS by yielding significantly lower recurrence and post-operative complication rates [4]. In this study, we compared also the results of Karydakis technique versus midline closure in patients with “primary” and “recurrent” PNS separately, and demonstrated that complication and recurrence rates were significantly less with the Karydakis flap in both subgroups. Over a 5-year period, Sondenaa et al. [35], treated 44 patients with recurrent PNS using excision and primary midline closure. They reported a high re-recurrence rate of 59.1% (26/44) during the first year post-operatively and attributed this high incidence, at least in part, to the high rate of post-operative infection. Post-operative complications are encountered more when midline closure is used to treat patients with recurrent PNS as compared to those with primary disease. Tension on the suture line and risk of accumulating hair in the midline clefts are considered the main problems associated with direct midline closure [40].
On the other hand, Karydakis technique has been shown to have a low recurrence rate ranging between 0% and 4.6% [4,12,27,29,41,42]. These reports however, do not reflect the results obtained exclusively for management of recurrent disease. Sakr et al. [4] for example, recorded recurrence in 2 out of 79 (2.5%) patients with chronic PNS treated with Karydakis flap (mean followup 30.4 months); however, only 16.5% of the patients (13/79) were treated for recurrent PNS. The low re-recurrence rate (3.2%) associated with Karydakis technique reported herein confirms the advantage of Karydakis flap over midline closure in managing recurrent cases, since it flattens the natal cleft, removes the vulnerable raphe, and avoids any wound scar in the depth of the inter-gluteal fold. Karydakis technique provides equal benefits of low complication and recurrence rates when used to treat both primary and recurrent PNS. Fashioning the flap with an appropriate thickness, tension-free flap fixation, and the prevention of collection by meticulous hemostasis and short-time suction drainage appear to be the keys to avoiding complications and recurrence after Karydakis procedure [27].
Based on the data presented, it may be concluded that 1) PNS affects mainly young, male, adults, who are usually, obese and hirsute, 2) the majority of patients with recurrent disease present within 3 years of the first surgery, 3) contrary to Karydakis technique, midline closure yields more post-operative complications when used to treat recurrent PNS as compared to primary PNS, and 4) Karydakis technique for the management of chronic PNS is a non-lengthy, efficient procedure that has less overall post-operative complications and a lower recurrence rate than conventional excision and midline closure, irrespective of the location of the sinuses, and whether PNS is primary or recurrent. Identifying independent variables responsible for post-operative morbidity and recurrence merit further investigation.
REFERENCES
- H. S. Khairi and J. H. Brown, “Excision and Primary Suture of Pilonidal Sinu,” Annals of the Royal College of Surgeons of England, Vol. 77, No. 4, 1995, pp. 242-244.
- D. P. Berry, “Pilonidal Sinus Disease,” Journal of Wound Care, Vol. 1, No. 3, 1992, pp. 29-32.
- G. E. Karydakis, “Easy and Successful Treatment of Pilonidal Sinus after Explanation of Its Causative Process,” Australian and New Zealand Journal of Surgery, Vol. 62, No. 6, 1992, pp. 385-389. doi:10.1111/j.1445-2197.1992.tb07208.x
- M. Sakr, M. Habib and A. Shaheed, “Assessment of Karydakis Technique as Compared with Midline Closure for the Management of Chronic Pilonidal Sinus,” Journal of Pelvic Medicine & Surgery, Vol. 12, No. 4, 2006, pp. 201-206. doi:10.1097/01.spv.0000217399.78641.43
- S. Chintapatla, N. Safarani, S. Kumar and N. Haboubi, “Sacrococcygeal Pilonidal Sinus: Historical Review, Pathological Insight and Surgical Options,” Techniques in Coloproctology, Vol. 7, No. 1, 2003, pp. 3-8. doi:10.1007/s101510300001
- M. F. Can, M. M. Sevinc and M. Yilmaz, “Comparison of Karydakis Flap Reconstruction versus Midline Closure in Sacrococcygeal Pilonidal Disease: Results of 200 Military Service Members,” Surgery Today, Vol. 39, No. 7, 2009, pp. 580-586. doi:10.1007/s00595-008-3926-0
- G. Nessar, C. Kayaalp and C. Seven, “Elliptical Rotation Flap for Pilonidal Sinus,” The American Journal of Surgery, Vol. 187, No. 2, 2004, pp. 300-303. doi:10.1016/j.amjsurg.2003.11.012
- W. P. T. James, “Review: WHO Recognition of the Global Obesity Epidemic,” International Journal of Obesity, Vol. 32, 2008, pp. 120-126. doi:10.1038/ijo.2008.247
- G. E. Karydakis, “New Approach to the Problem of Pilonidal Sinus,” Lancet, 1973, No. 7843, 1973, pp. 1414-1415. doi:10.1016/S0140-6736(73)92803-1
- R. L. Rosenfield, “Clinical Practice. Hirsutism,” New England Journal of Medicine, Vol. 353, 2005, pp. 2578-2588. doi:10.1056/NEJMcp033496
- A. E. Humphries and J. E. Duncan, “Evaluation and Management of Pilonidal Disease,” Surgical Clinics of North America, Vol. 90, No. 1, 2010, pp. 113-124. doi:10.1016/j.suc.2009.09.006
- M. Sakr, H. El-Hammadi, M. Moussa, S. Arafa and M. Rasheed, “The Effect of Obesity on the Results of Karydakis Technique for the Management of Chronic Pilonidal Sinus,” International Journal of Colorectal Disease, Vol. 18, No. 1, 2003, pp. 36-39. doi:10.1007/s00384-002-0407-6
- A. Cubukcu, N. N. Gonullu, M. Paksoy, A. Alponat, M. Kuru and O. Ozbay, “Role of Obesity on the Recurrence of Pilonidal Sinus Disease in Patients Who Were Treated by Excision and Limberg Flap Transposition,” International Journal of Colorectal Disease, Vol. 15, No. 3, 2000, pp. 173-175. doi:10.1007/s003840000212
- T. G. Allen-Mersh, “Pilonidal Sinus: Finding the Right Track for Treatment,” British Journal of Surgery, Vol. 77, No. 2, 1990, pp. 123-132. doi:10.1002/bjs.1800770203
- M. Fuzun, I. Bakir, M. Soylu, T. Tansung, E. Kaymak and O. Harmancioglu, “Which Technique for Pilonidal Sinus—Open or Closed?” Diseases of the Colon & Rectum, Vol. 37, No. 11, 1994, pp. 1148-1150.
- K. Sondenaa, E. Andeersen and J. A. Soreide, “Morbidity and Short Term Results in a Randomized Trial of Open Compared to Closed Treatment of Chronic Pilonidal Sinus,” European Journal of Surgery, Vol. 158, 1992, pp. 351-355.
- J. A. Solla and D. A. Rothenberger, “Chronic Pilonidal Disease. An Assessment of 150 Cases,” Diseases of the Colon & Rectum, Vol. 33, No. 9, 1990, pp. 753-761. doi:10.1007/BF02052321
- I. P. Bissett and W. H. Isbister, “The Management of Patients with Pilonidal Disease—A Comparative Study,” Australian and New Zealand Journal of Surgery, Vol. 57, No. 12, 1987, pp. 939-942. doi:10.1111/j.1445-2197.1987.tb01298.x
- H. Spivac, V. L. Brooks, M. Nussbaum and I. Friedman, “Treatment of Chronic Pilonidal Disease,” Diseases of the Colon & Rectum, Vol. 39, No. 10, 1996, pp. 1136-1139. doi:10.1007/BF02081415
- M. J. Notaras, “A Review of Three Popular Methods of Treatment of Postanal (pilonidal) Disease,” British Journal of Surgery, Vol. 57, No. 12, 1970, pp. 886-890. doi:10.1002/bjs.1800571204
- H. T. Khawaja, S. Bryan and P. C. Weaver, “Treatment of Natal Cleft Sinus: A Prospective Clinical and Economical Evaluation,” BMJ, Vol. 304, 1992, pp. 1282-1283. doi:10.1136/bmj.304.6837.1282
- K. K. Hameed, “Outcome of Surgery for Chronic Natal Cleft Pilonidal Sinus: A Randomized Trial of Open Compared with Closed Technique,” Medical Forums, Vol. 12, 2001, pp. 20-23.
- H. A. Mohamed, I. Kadry and S. Adly, “Comparison between Three Therapeutic Modalities for Non-Complicated Pilonidal Sinus Disease,” Surgeon, Vol. 3, No. 2, 2005, pp. 73-77. doi:10.1016/S1479-666X(05)80065-4
- M. Miocinovic, M. Horzic and D. Bunoza, “The Treatment of Pilonidal Disease of the Sacrococcygeal Region by the Method of Limited Excision and Open Wound Healing,” Acta Medica Croatica, Vol. 54, No. 1, 1999, pp. 27-31.
- M. Oncel, N. Kurt, M. Kemet, E. Colak, M. Eser and H. Uzun, “Excision and Marsupialization versus Sinus Excision for the Treatment of Limited Chronic Pilonidal Disease: A Prospective Randomized Trial,” Techniques in Coloproctology, Vol. 6, No. 3, 2002, pp. 165-169. doi:10.1007/s101510200037
- J. R. Notaro, “Management of Recurrent Pilonidal Disease,” Seminars in Colon & Rectal Surgery, Vol. 14, No. 4, 2003, pp. 173-185. doi:10.1053/j.scrs.2004.03.002
- M. F. Can, M. M. Sevinc, O. Hancerliogullari, M. Yilmaz and G. Yagci, “Multicenter Prospective Randomized Trial Comparing Modified Limberg Flap Transposition and Karydakis Flap Reconstruction in Patients with Sacrococcygeal Pilonidal Disease,” The American Journal of Surgery, Vol. 200, No. 3, 2010, pp. 318-327. doi:10.1016/j.amjsurg.2009.08.042
- S. A. M. Abdulrahman, A. S. Mohammed and H. A. Hamdoun, “Pilonidal Sinus in Males: To Preserve or Obliterate the Natal Cleft,” Saudi Medical Journal, Vol. 23, 2002, pp. 875-876.
- O. F. Akinici, A. Coskun and A. Uzunkoy, “Simple and Effective Treatment of Pilonidal Sinus: Asymmetric Excision and Primary Closure Using Suction Drain and Subcuticular Skin Closure,” Diseases of the Colon & Rectum, Vol. 43, 2000, pp. 706-707.
- H. Patel, M. Lee, I. Bloom and T. G. Allen-Mersh, “Prolonged Delay in Healing after Surgical Treatment of Pilonidal Sinus Is Avoidable,” Colorectal Disease, Vol. 1, No. 2, 1999, pp. 107-110. doi:10.1046/j.1463-1318.1999.00030.x
- A. C. Anyanwi, S. Hossain, A. Williams and A. C. Montgomery, “Karydakis Operation for Sacrococcygeal Pilonidal Sinus Disease: Experience in a District General Hospital,” Annals of the Royal College of Surgeons of England, Vol. 80, 1998, pp. 197-199.
- P. R. B. Kitchen, “Pilonidal Sinus: Experience with the Karydakis Flap,” British Journal of Surgery, Vol. 83, No. 10, 1996, pp. 1452-1455. doi:10.1002/bjs.1800831040
- T. M. El-Jaberi, “Excision and Simple Closure of Chronic Pilonidal Sinus,” European Journal of Surgery, Vol. 167, No. 2, 2001, pp. 133-135. doi:10.1080/110241501750070600
- A. Senapati, N. P. Cripps and M. R. Thompson, “Bascom’s Operation in the Day-Surgical Management of Symptomatic Pilonidal Sinus,” British Journal of Surgery, Vol. 87, No. 8, 2000, pp. 1067-1070. doi:10.1046/j.1365-2168.2000.01472.x
- K. Sondenaa, I. Nesvik, E. Andersen, L. Pollard and J. R. Soreide, “Recurrent Pilonidal Sinus: Etiology and Treatment,” Digestive Surgery, Vol. 12, No. 2, 1995, pp. 117-120. doi:10.1159/000172329
- T. Z. Nursal, A. Ezer, K. Caliskan, N. Torer, S. Belli and G. Moray, “Prospective Randomized Controlled Trial Comparing V-Y Advancement Flap with Primary Suture Methods in Pilonidal Disease,” American Journal of Surgery, Vol. 199, No. 2, 2010, pp. 170-177. doi:10.1016/j.amjsurg.2008.12.030
- D. Doll, E. Matevossian, K. Wietelmann, T. Evers, M. Kriner and S. Petersen, “Family History of Pilonidal Sinus Predisposes to Earlier Onset of Disease and a 50% Long-Term Recurrence Rate,” Diseases of the Colon & Rectum, Vol. 52, No. 9, 2009, pp. 1610-1615. doi:10.1007/DCR.0b013e3181a87607
- D. Doll, C. M. Krueger, S. Schrank, H. Dettmann, S. Petersen and W. Duesel, “Timeline of Recurrence after Primary and Secondary Pilonidal Sinus Surgery,” Diseases of the Colon & Rectum, Vol. 50, No. 11, 2007, pp. 1928-1934. doi:10.1007/s10350-007-9031-4
- G. E. Theodoropoulos, K. Vlahos, A. C. Lazaris, E. Tahteris and D. Panoussopoulos, “Modified Bascom’s Asymmetric Midgluteal Cleft Closure Technique for Recurrent Pilonidal Disease: Early Experience in a Military Hospital,” Diseases of the Colon & Rectum, Vol. 46, No. 9, 2003, pp. 1286-1291. doi:10.1007/s10350-004-6729-4
- T. W. Khanzada and A. Samad, “Recurrence after Excision and Primary Closure of Pilonidal Sinus,” Pakistan Journal of Medical Sciences, Vol. 23, No. 3, 2007, pp. 375-379.
- A. Gurer, I. Gomceli, M. Ozdogan, et al., “Is routine Cavity Drainage Necessary in Karydakis Flap Operation? A Prospective, Randomized Trial,” Diseases of the Colon & Rectum, Vol. 48, No. 9, 2005, pp. 1797-1799. doi:10.1007/s10350-005-0108-7
- S. Petersen, R. Koch, S. Stelzner, et al., “Primary Closure Techniques in Chronic Pilonidal Sinus: A Survey of the Results of Different Surgical Approaches,” Diseases of the Colon & Rectum, Vol. 45, No. 11, 2002, pp. 1458-1567. doi:10.1007/s10350-004-6451-2

